Abstract
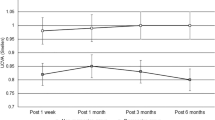
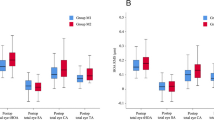
The objective of the study is to observe the changes in the effective optical zone (EOZ) after small incision lenticule extraction (SMILE) and explore possible correlations with some influencing factors. In total, 133 eyes after SMILE were divided into the mild to moderate myopia group (− 1.75 D to − 5.75 D, 70 eyes) and the high myopia group (− 6.00 D to − 9.50 D, 63 eyes). The postoperative EOZ was calculated by utilizing the corneal tangential curvature map. Changes in EOZ (△-OZ) were monitored and compared between the two groups. Pearson correlation analysis was conducted to determine the correlation between △-OZ and corneal high-order wavefront aberrations. Multicollinearity analysis and ridge regression analysis were performed to assess the correlation between △-OZ and some corneal parameters. After SMILE, the horizontal EOZ (H-EOZ), vertical EOZ (V-EOZ), and average EOZ (A-EOZ) were significantly smaller than the programmed optical zone (POZ) in both groups (p < 0.05). The difference between V-EOZ and POZ (△V-OZ) and the difference between A-EOZ and POZ (△A-OZ) showed more significant changes in the high myopia group than in the mild to moderate myopia group, and △V-OZ was significantly larger than the difference between H-EOZ and POZ (△H-OZ) in the high myopia group. In both groups, the total high-order aberration (T-HOA) and spherical aberration (SA) both increased after SMILE, and they had a similar significant negative correlation with A-EOZ. Moreover, there was a significant negative correlation between △-OZ and Km (X1), Q-value (X2), spherical equivalent (SE, X3), ablating depth (AD, X4) and △e (X6), and a significant positive correlation between △-OZ and △Q (X5). △H-OZ was expressed as Y1, △V-OZ as Y2, and △A-OZ as Y3. The multiple linear regression equations were as follows: Y1 = 3.683 − 0.065X1, Y2 = 1.549 − 0.469X2 − 0.059X3, Y3 = 4.015 − 0.07X1 − 0.03X3, Y1 = 1.337 − 0.005X4 + 0.413X5, Y2 = 1.265 + 0.469X5, and Y3 = 0.852 − 0.002X4 − 0.398X6. The correlation degree with △A-OZ was ranked as Km > △Q > Q-value > AD > e-value > △e > SE > △Km, as represented by the ridge regression analysis. The EOZ was irregularly reduced after SMILE, which should be taken into consideration in the design of POZ, especially for high myopia. Consideration of the refractive diopter and corneal topography is advised for the design of POZ, the latter of which has greater reference significance.



Similar content being viewed by others
Data availability
The data used to support the findings of this study are included in the article.
References
Zhang JH, Wang SR, He YX, Yao BY, Zhang Y (2020) The best optical zone for small-incision lenticule extraction in high myopic patients. J Cataract Refract Surg 46(9):1302–1307
Partal AE, Manche EE (2003) Diameters of topographic optical zone and programmed ablation zone for laser in situ keratomileusis for myopia. J Refract Surg 19(5):528–33
Hou L, Wang Y, Lei Y, Zheng X (2018) Comparison of effective optical zone after small-incision lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis for myopia. J Cataract Refract Surg 44:1179–1185
Boxer Wachler BS, Huynh VN, El-Shiaty AF, Goldberg D (2002) Evaluation of corneal functional optical zone after laser in situ keratomileusis. J Cataract Refract Surg 28:948–953
Racine L, Wang L, Koch DD (2006) Size of corneal topographic effective optical zone: comparison of standard and customized myopic laser in situ keratomileusis. Am J Ophthalmol 142(2):227–232
Fu D, Wang L, Zhou X, Yu Z (2018) Functional optical zone after small-incision lenticule extraction as stratified by attempted correction and optical zone. Cornea 37(9):1110–1117
Hou J, Wang Y, Lei Y (2016) Corneal epithelial remodeling and its effect on corneal asphericity after transepithelial photorefractive keratectomy for myopia. J Ophthalmol 2016:8582362
Damgaard IB, Ang M, Mahmoud AM, Farook M, Roberts CJ, Mehta JS (2019) Functional optical zone and centration following SMILE and LASIK: a prospective, randomized, contralateral eye study. J Refract Surg 35(4):230–237
Ramírez M, Hernández-Quintela E, Naranjo-Tackman R (2012) Epi-LASIK: a confocal microscopy analysis of the corneal epithelium and anterior stroma. Ophthalmic Surg Lasers Imaging 43(4):319–322
Romito N, Trinh L, Goemaere I, Borderie V, Laroche L, Bouheraoua N (2020) Corneal remodeling after myopic SMILE: an optical coherence tomography and in vivo confocal microscopy study. J Refract Surg 36(9):597–605
Alarcón A, Rubiño M, Pééérez-Ocón F, Jiménez JR (2012) Theoretical analysis of the effect of pupil size, initial myopic level, and optical zone on quality of vision after corneal refractive surgery. J Refract Surg 28(12):901–906
Fan-Paul NI, Li J, Miller JS, Florakis GJ (2002) Night vision disturbances after corneal refractive surgery. Surv Ophthalmol 47(6):533–546
Smadja D, Santhiago MR, Mello GR, Touboul D, Mrochen M, Krueger RR (2013) Corneal higher order aberrations after myopic wavefront-optimized ablation. J Refract Surg 29(1):42–48
Kim JH (2019) Multicollinearity and misleading statistical results. Korean J Anesthesiol 72(6):558–569
Jain RK (1985) Ridge regression and its application to medical data. Comput Biomed Res 18(4):363–368
Partal AE, Manche EE (2003) Diameters of topographic optical zone and programmed ablation zone for laser in situ keratomileusis for myopia. J Refract Surg 19:528–533
Tabernero J, Klyce SD, Sarver EJ, Artal P (2007) Functional optical zone of the cornea. Invest Ophthalmol Vis Sci 48(3):1053–1060
Fan R, Chan TC, Prakash G, Jhanji V (2018) Applications of corneal topography and tomography: a review. Clin Exp Ophthalmol 46(2):133–146
Camellin M, Arba MS (2011) Aspheric optical zones: the effective optical zone with the SCHWIND AMARIS. J Refract Surg 27(2):135–146
Yan H, Gong LY, Huang W, Peng YL (2017) Clinical outcomes of small incision lenticule extraction versus femtosecond Iaser-assisted LASIK for myopia: a meta-analysis. Int J Ophthalmol 10(9):1436–1445
Dackowski EK, Lopath PD, Chuck RS (2020) Preoperative, intraoperative, and postoperative assessment of corneal biomechanics in refractive surgery. Curr Opin Ophthalmol 31(4):234–240
Qian Y, Chen X, Naidu RK, Zhou X (2020) Comparison of efficacy and visual outcomes after SMILE and FS LASIK for the correction of high myopia with the sum of myopia and astigmatism from 10.00 to 14.00 dioptres. Acta Ophthalmol 98(2):e161–e172
Pedersen IB, Ivarsen A, Hjortdal J (2017) Changes in astigmatism, densitometry, and aberrations after SMILE for low to high myopic astigmatism: a 12-month prospective study. J Refract Surg 33(1):11–17
Fuller DG, Alperin D (2013) Variations in corneal asphericity (Q value) between African-Americans and whites. Optom Vis Sci 90(7):667–673
Xiong Y, Li J, Wang N, Liu X, Wang Z, Tsai FF, Wan X (2017) The analysis of corneal asphericity (Q value) and its related factors of 1,683 Chinese eyes older than 30 years. PLoS ONE 12(5):e0176913
Gatinel D, Adam PA, Chaabouni S, Munck J, Thevenot M, Hoang-Xuan T, Pieger S, Fujieda M, Bains HS (2010) Comparison of corneal and total ocular aberrations before and after myopic LASIK. J Refract Surg 26(5):333–340
Funding
This work was supported by the National Natural Science Foundation of China (No. 82000937), the Hunan Provincial Innovation Foundation for Postgraduate (CX20200317), the Education Foundation of Hunan Province (2020JGZDO11), and the Education Foundation of Xiangya Hospital (2020JGA008).
Author information
Authors and Affiliations
Contributions
YYF was involved in the analysis and interpretation of data, providing statistical expertise, and drafting the manuscript. YWY was involved in the conception and design of the study, analysis and interpretation of data, and critical revision of the manuscript. YZ was involved in the collection and analysis of data. YJL and YL were involved in funding acquisition. AQX and QMF were involved in the data collection. TH, KXD, and SFH were involved in the instrumentation. XYW was involved in the supervision and conception of the study. DW was involved in the supervision, conception and design of the study, and funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yewei Yin and Yanyan Fu are co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fu, Y., Yin, Y., Zhao, Y. et al. Changes of the effective optical zone after small-incision lenticule extraction and a correlation analysis. Lasers Med Sci 38, 14 (2023). https://doi.org/10.1007/s10103-022-03666-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-022-03666-1