Abstract
Purpose
To find a new approach of pan-retinal photocoagulation (PRP) with less damage to the retina in the treatment of severe non-proliferative diabetic retinopathy (NPDR), this study compared functional changes in the retina after subthreshold and threshold PRP treatment in severe NPDR eyes.
Methods
Post hoc analysis of a randomized clinical trial was conducted in this study. Seventy eyes of 35 patients with bilateral, symmetric, severe NPDR were enrolled. Two eyes from the same patient were randomized into two groups, one eye received subthreshold PRP (S-PRP) and the other eye received threshold PRP (T-PRP). Comprehensive ophthalmological evaluations were performed on the baseline and every 3 months for 1 year. Visual field (VF) and full-field electroretinography (ERG) were performed on the baseline and repeated at month 12.
Results
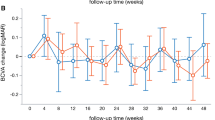
During the 12-month follow-up, 4 eyes (11.4%) in the S-PRP group and 3 eyes (8.6%) in the T-PRP group progressed to proliferative diabetic retinopathy (PDR) stage, and there was no statistical difference in PDR progression rate between the two groups (P = 0.69). In addition, the changes in best-corrected visual acuity (BCVA) from baseline to month 12 between the two groups had no statistical difference (P = 0.30). From baseline to month 12, changes in central VF between the two groups had no statistical difference (P = 0.25), but changes in total score points of peripheral VF in the S-PRP group (− 242.1 ± 210.8 dB) and the T-PRP group (− 308.9 ± 209.7 dB) were statistically significant (P = 0.03). At month 12, ERG records showed that the amplitude of dark-adapted 0.01 ERG, dark-adapted 3.0 ERG, oscillatory potentials, light-adapted 3.0 ERG, and 30 Hz flicker ERG of both groups were significantly decreased from the baseline (P < 0.05). In addition, the amplitude of each ERG record in the S-PRP group decreased significantly less than those in the T-PRP group (P < 0.05).
Conclusions
Subthreshold PRP is as effective as threshold PRP for preventing severe NPDR progress to PDR within 1 year with less damage to periphery VF and retinal function.
Trial registration.
ClinicalTrials.gov Identifier: NCT01759121.




Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Code availability
Not applicable.
References
Klein BEK (2007) Overview of epidemiologic studies of diabetic retinopathy. In: Ophthalmic epidemiology. Ophthalmic Epidemiol, pp 179–183
Flaxel CJ, Adelman RA, Bailey ST et al (2020) Diabetic Retinopathy Preferred Practice Pattern®. Ophthalmology 127:P66–P145. https://doi.org/10.1016/j.ophtha.2019.09.025
(1991) Early photocoagulation for diabetic retinopathy: ETDRS Report Number 9. Ophthalmology. https://doi.org/10.1016/S0161-6420(13)38011-7
Blumenkranz MS, Yellachich D, Andersen DE et al (2006) Semiautomated patterned scanning laser for retinal photocoagulation. Retina 26:370–376. https://doi.org/10.1097/00006982-200603000-00024
At J, Blumenkranz MS, Paulus Y et al (2008) Effect of pulse duration on size and character of the lesion in retinal photocoagulation. Arch Ophthalmol 126:78–85. https://doi.org/10.1001/archophthalmol.2007.29
Muqit MMK, Young LB, McKenzie R et al (2013) Pilot randomised clinical trial of Pascal TargETEd Retinal versus variable fluence PANretinal 20 ms laser in diabetic retinopathy: PETER PAN study. Br J Ophthalmol 97:220–227. https://doi.org/10.1136/bjophthalmol-2012-302189
Muqit MMK, Marcellino GR, Henson DB et al (2010) Single-session vs multiple-session pattern scanning laser panretinal photocoagulation in proliferative diabetic retinopathy: The Manchester Pascal study. Arch Ophthalmol 128:525–533. https://doi.org/10.1001/archophthalmol.2010.60
Muqit MMK, Marcellino GR, Henson DB et al (2011) Randomized clinical trial to evaluate the effects of pascal panretinal photocoagulation on macular nerve fiber layer: Manchester pascal study report 3. Retina 31:1699–1707. https://doi.org/10.1097/IAE.0b013e318207d188
Muqit MMK, Marcellino GR, Gray JCB et al (2010) Pain responses of Pascal 20 ms multi-spot and 100 ms single-spot panretinal photocoagulation: Manchester Pascal Study, MAPASS report 2. Br J Ophthalmol 94:1493–1498. https://doi.org/10.1136/bjo.2009.176677
Hamada M, Ohkoshi K, Inagaki K et al (2018) Subthreshold photocoagulation using endpoint management in the PASCAL® System for diffuse diabetic macular edema. J Ophthalmol 2018:7465794. https://doi.org/10.1155/2018/7465794
Lai K, Zhao H, Zhou L et al (2020) Subthreshold pan-retinal photocoagulation using endpoint management algorithm for severe non-proliferative diabetic retinopathy: a paired controlled pilot prospective study. Ophthalmic Res. https://doi.org/10.1159/000512296
McCulloch DL, Marmor MF, Brigell MG et al (2015) ISCEV Standard for full-field clinical electroretinography (2015 update). Doc Ophthalmol 130:1–12. https://doi.org/10.1007/s10633-014-9473-7
Lavinsky D, Sramek C, Wang J, et al (2014) Subvisible retinal laser therapy: titration algorithm and tissue response. Retina. https://doi.org/10.1097/IAE.0b013e3182993edc
Varma R, Torres M, Peña F et al (2004) Prevalence of diabetic retinopathy in adult Latinos: the Los Angeles Latino eye study. Ophthalmology 111:1298–1306. https://doi.org/10.1016/j.ophtha.2004.03.002
Royle P, Mistry H, Auguste P, et al (2015) Pan-retinal photocoagulation and other forms of laser treatment and drug therapies for non-proliferative diabetic retinopathy: systematic review and economic evaluation. Health Technol Assess (Rockv) 19. https://doi.org/10.3310/hta19510
Vergmann AS, Grauslund J (2020) Changes of visual fields in treatment of proliferative diabetic retinopathy: a systematic review. Acta Ophthalmol 98:763–773. https://doi.org/10.1111/aos.14474
DUNCAN JL (2001) Electrophysiologic testing in disorders of the retina, optic nerve, and visual pathway. Br J Ophthalmol. https://doi.org/10.1136/bjo.85.8.1013e
Tzekov R, Arden GB (1999) The electroretinogram in diabetic retinopathy. Surv Ophthalmol 44:53–60. https://doi.org/10.1016/S0039-6257(99)00063-6
Messias A, Filho JAR, Messias K et al (2012) Electroretinographic findings associated with panretinal photocoagulation (PRP) versus PRP plus intravitreal ranibizumab treatment for high-risk proliferative diabetic retinopathy. Doc Ophthalmol 124:225–236. https://doi.org/10.1007/s10633-012-9322-5
Messias K, de Barroso RM, Jorge R, Messias A (2018) Retinal function in eyes with proliferative diabetic retinopathy treated with intravitreal ranibizumab and multispot laser panretinal photocoagulation. Doc Ophthalmol 137:121–129. https://doi.org/10.1007/s10633-018-9655-9
Messias A, Ramos Filho JA, Messias K et al (2012) Electroretinographic findings associated with panretinal photocoagulation (PRP) versus PRP plus intravitreal ranibizumab treatment for high-risk proliferative diabetic retinopathy. Doc Ophthalmol 124:225–236. https://doi.org/10.1007/s10633-012-9322-5
Khojasteh H, Vishte RA, Mirzajani A et al (2020) Electroretinogram changes following sequential panretinal photocoagulation for proliferative diabetic retinopathy. Clin Ophthalmol 14:967–975. https://doi.org/10.2147/OPTH.S248678
Perlman I, Gdal-on M, Miller B, Zonis S (1985) Retinal function of the diabetic retina after argon laser photocoagulation assessed electroretinographically. Br J Ophthalmol. https://doi.org/10.1136/bjo.69.4.240
Acknowledgements
The authors are grateful to Li Ma, Guandi Chen, and Jinger He.
Funding
This study was funded by the Natural Science Foundation of Guangdong Province (2021A515011106).
Author information
Authors and Affiliations
Contributions
Conception and design: Chenjin Jin.
Data collection: Kunbei Lai, Chuangxin Huang, Fabao Xu, Cong Li
Analysis and interpretation: Hongkun Zhao and Lijun Zhou
Revise: Chenjin Jin, Lin Lu and Minzhong Yu
Obtained funding and overall responsibility: Chenjin Jin
Corresponding author
Ethics declarations
Ethic approval
This study was performed in line with the principles of the Declaration of Helsinki and was approved by the Institutional Review Board of Zhongshan Ophthalmic Center.
Consent to participate
Written consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, H., Zhou, L., Lai, K. et al. Comparison of functional changes of retina after subthreshold and threshold pan-retinal photocoagulation in severe non-proliferative diabetic retinopathy. Lasers Med Sci 37, 3561–3569 (2022). https://doi.org/10.1007/s10103-022-03635-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03635-8