Abstract
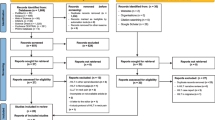
Exercise is often pointed out as an effective form of treatment in the clinical management of chronic neck pain (CNP). However, due to its complex range of causal factors and great diversity of signs and symptoms, other resources such as photobiomodulation therapy (PBMT) have been routinely used for the treatment of CNP. The aim of this study was to systematically review the literature on the use of the association of PBMT and therapeutic exercises in relation to pain intensity and neck disability in individuals with CNP. PubMed, Medline (via Ovid), Embase (via Ovid), Cinahl (via Ebsco), and Central (via Cochrane library) databases were searched using the following terms: “laser,” “low-level laser,” “photobiomodulation,” “light emitting diodes,” “phototherapy,” “exercise,” “chronic neck pain.” After verification and implementation of eligibility criteria, seven manuscripts were considered eligible for data analysis. These manuscripts had methodological quality between 5 and 8 points on the PEDro scale. Most studies used low infrared laser therapy to perform PBMT, with a wide range of parameters and energy density between 2 and 7 J/cm2 and a total treatment time between 2 and 6 weeks. Four studies showed significant benefits in terms of pain intensity at short-term follow-up and one at intermediate-term follow-up. However, only one showed a minimal clinically important change. No studies have shown significant improvement in disability. This review demonstrates that the association of PBMT with therapeutic exercises in general promotes significant benefits only for the intensity of pain. However, it does not seem to promote a minimally effective clinical difference in individuals with CNP.

Similar content being viewed by others
References
GBD 2017 (2018) Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1789–1858. https://doi.org/10.1016/S0140-6736(18)32279-7
Cohen SP, Hooten WM (2017) Advances in the diagnosis and management of neck pain. BMJ 358:j3221. https://doi.org/10.1136/bmj.j3221
Andias R, Silva AG (2019) A systematic review with meta-analysis on functional changes associated with neck pain in adolescents. Musculoskeletal Care 17:23–36. https://doi.org/10.1002/msc.1377
Catley MJ, O’Connell NE, Berryman C et al (2014) Is tactile acuity altered in people with chronic pain? A systematic review and meta-analysis. J Pain 15:985–1000. https://doi.org/10.1016/j.jpain.2014.06.009
May S, Gardiner E, Young S et al (2008) Predictor variables for a positive long-term functional outcome in patients with acute and chronic neck and back pain treated with a McKenzie approach: a secondary analysis. J Man Manip Ther 16:155–160. https://doi.org/10.1179/jmt.2008.16.3.155
Peterson C, Bolton J, Humphreys BK (2012) Predictors of outcome in neck pain patients undergoing chiropractic care: comparison of acute and chronic patients. Chiropr Man Therap 20:27. https://doi.org/10.1186/2045-709X-20-27
Pillastrini P, Castellini G, Chiarotto A et al (2019) Comparative effectiveness of conservative and pharmacological interventions for chronic non-specific neck pain: protocol of a systematic review and network meta-analysis. Medicine (Baltimore) 98:e16762. https://doi.org/10.1097/MD.0000000000016762
Geneen LJ, Moore RA, Clarke C et al (2017) Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev 4:4. https://doi.org/10.1002/14651858.CD011279.pub3
O’Riordan C, Clifford A, Van De Ven P et al (2014) Chronic neck pain and exercise interventions: frequency, intensity, time, and type principle. Arch Phys Med Rehabil 95:770–783. https://doi.org/10.1016/j.apmr.2013.11.015
Chow RT, Barnsley L (2005) Systematic review of the literature of low-level laser therapy (LLLT) in the management of neck pain. Lasers Surg Med 37:46–52. https://doi.org/10.1002/lsm.20193
Chow RT, Johnson MI, Lopes-Martins RA et al (2009) Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet 374:1897–1908. https://doi.org/10.1016/S0140-6736(09)61522-1
Kadhim-Saleh A, Maganti H, Ghert M et al (2013) Is low-level laser therapy in relieving neck pain effective? Systematic review and meta-analysis. Rheumatol Int 33:2493–2501. https://doi.org/10.1007/s00296-013-2742-z
Gross AR, Dziengo S, Boers O et al (2013) Low level laser therapy (LLLT) for neck pain: a systematic review and meta-regression. Open Orthop J 20:396–419. https://doi.org/10.2174/1874325001307010396
Ferraresi C, Huang YY, Hamblin MR (2016) Photobiomodulation in human muscle tissue: an advantage in sports performance? J Biophotonics 9:1273–1299. https://doi.org/10.1002/jbio.201600176
Hawkins D, Abrahamse H (2006) Effect of multiple exposures of low-level laser therapy on the cellular responses of wounded human skin fibroblasts. Photomed Laser Surg 24:705–714. https://doi.org/10.1089/pho.2006.24.705
Khoo NK, Shokrgozar MA, Kashani IR et al (2014) In vitro therapeutic effects of low level laser at mRNA level on the release of skin growth factors from fibroblasts in diabetic mice. Avicenna J Med Biotechnol 6:113–118
Ozdemir F, Birtane M, Kokino S (2001) The clinical efficacy of low-power laser therapy on pain and function in cervical osteoarthritis. Clin Rheumatol 20:181–184. https://doi.org/10.1007/s100670170061
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Cochrane Back Review Group (2021) www.back.cochrane.org. Accessed 10 January 01 2021
van Tulder M, Becker A, Bekkering T et al (2016) Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 15:S169–91. https://doi.org/10.1007/s00586-006-1071-2
Maher CG, Sherrington C, Herbert RD et al (2003) Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 83:713–721
Macedo LG, Elkins MR, Maher CG et al (2010) There was evidence of convergent and construct validity of Physiotherapy Evidence Database quality scale for physiotherapy trials. J Clin Epidemiol 63:920–925. https://doi.org/10.1016/j.jclinepi.2009.10.005
Shiwa SR, Costa LO, da Costa L, C, et al (2011) Reproducibility of the Portuguese version of the PEDro Scale. Cad Saude Publica 27:2063–2068. https://doi.org/10.1590/s0102-311x2011001000019
PEDro - Physiotherapy Evidence Database (2021) https://pedro.org.au. Accessed 10 January 2021
Alayat MS, Elsoudany AM, Ali ME (2017) Efficacy of multiwave locked system laser on pain and function in patients with chronic neck pain: a randomized placebo-controlled trial. Photomed Laser Surg 35:450–455. https://doi.org/10.1089/pho.2017.4292
Waseem I, Tanveer F, Fatima A (2020) Can addition of low level laser therapy to conventional physical therapy be beneficial for management of pain and cervical range of motion in patients with trigger point of upper trapezius? Anaesth Pain Intens Care 24(1):64–68. https://doi.org/10.35975/apic.v24i1.1228
Sumen A, Sarsan A, Alkan H et al (2015) Efficacy of low level laser therapy and intramuscular electrical stimulation on myofascial pain syndrome. J Back Musculoskelet Rehabil 28:153–158. https://doi.org/10.3233/BMR-140503
Dundar U, Evcik D, Samli F et al (2007) The effect of gallium arsenide aluminum laser therapy in the management of cervical myofascial pain syndrome: a double blind, placebo-controlled study. Clin Rheumatol 26:930–934. https://doi.org/10.1007/s10067-006-0438-4
Altan L, Bingöl U, Aykaç M et al (2005) Investigation of the effect of GaAs laser therapy on cervical myofascial pain syndrome. Rheumatol Int 25:23–27. https://doi.org/10.1007/s00296-003-0396-y
Ilbuldu E, Cakmak A, Disci R et al (2004) Comparison of laser, dry needling, and placebo laser treatments in myofascial pain syndrome. Photomed Laser Surg 22:306–311. https://doi.org/10.1089/pho.2004.22.306
Hakgüder A, Birtane M, Gürcan S et al (2003) Efficacy of low level laser therapy in myofascial pain syndrome: an algometric and thermographic evaluation. Lasers Surg Med 33:339–343. https://doi.org/10.1002/lsm.10241
Pool JJ, Ostelo RW, Hoving JL et al (2007) Minimal clinically important change of the Neck Disability Index and the Numerical Rating Scale for patients with neck pain. Spine (Phila Pa 1976) 32:3047–51. https://doi.org/10.1097/BRS.0b013e31815cf75b
Blanpied PR, Gross AR, Elliott JM et al (2017) Neck Pain: revision 2017. J Orthop Sports Phys Ther 47:A1–A83. https://doi.org/10.2519/jospt.2017.0302
MacDermid JC, Walton DM, Avery S et al (2009) Measurement properties of the neck disability index: a systematic review. J Orthop Sports Phys Ther 39:400–417. https://doi.org/10.2519/jospt.2009.2930
Funding
This work was partially supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), finance code 001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
da Silva Júnior, J., Vieira Dibai-Filho, A., de Santana, G. et al. Association of photobiomodulation therapy and therapeutic exercises in relation to pain intensity and neck disability in individuals with chronic neck pain: a systematic review of randomized trials. Lasers Med Sci 37, 1427–1440 (2022). https://doi.org/10.1007/s10103-021-03454-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03454-3