Abstract
To evaluate the effectiveness of photobiomodulation (PBM) on primary burning mouth syndrome (pBMS). We searched Chinese and English studies published before February 10, 2020. The databases used include PubMed, EMBASE, the Cochrane Library, Web of Science, Wanfang Database, and China National Knowledge Infrastructure (CNKI). Randomized controlled clinical trials (RCTs) that used the PBM to treat pBMS and reported specific treatment outcomes were considered for inclusion. We eventually included 12 RCTs, and 574 samples were included in these studies. The primary outcomes investigated were pain reduction and life quality improvement. A meta-analysis performed on 9 groups in 5 trials showed that PBM was effective in reducing pain compared with placebo (MD − 1.86, 95% CI − 2.59 to − 1.13, Z = 4.99, P < 0.00001). Meta-analysis was also performed on 7 groups in 4 trials and showed that PBM was effective in improving life quality compared with placebo (MD − 3.43, 95% CI − 5.11 to − 1.75, Z = 4.00, P < 0.0001). Qualitative analysis of the included RCTs found that PBM might also play a role in the decrease of TNF-α and IL-6 in saliva. Three studies that compared PBM with medications were evaluated by descriptive analysis. None of the treatment-related adverse event was reported. Up to date, PBM appears to have an effect on pain reduction and life quality improvement in pBMS patients. However, more evidence is still required to warrant its efficacy and safety in treating pBMS.





Similar content being viewed by others
References
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38(1):1–211
Treede RD, Rief W, Barke A et al (2019) Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International Classification of Diseases (ICD-11). Pain 160(1):19–27
Coculescu EC, Tovaru S, Coculescu BI (2014) Epidemiological and etiological aspects of burning mouth syndrome. J Med Life 7(3):305–309
Klasser GD, Fischer DJ, Epstein JB (2008) Burning mouth syndrome: recognition, understanding, and management. Oral Maxillofac Surg Clin North Am 20(2):255–271 vii
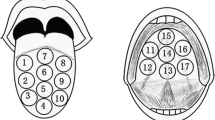
Grushka M (1987) Clinical features of burning mouth syndrome. Oral Surg Oral Med Oral Pathol 63(1):30–36
Ariyawardana A, Chmieliauskaite M, Farag AM et al (2019) World workshop on oral medicine VII: burning mouth syndrome: a systematic review of disease definitions and diagnostic criteria utilized in randomized clinical trials. Oral Dis null:141–156
Ducasse D, Courtet P, Olie E (2013) Burning mouth syndrome: current clinical, physiopathologic, and therapeutic data. Reg Anesth Pain Med 38(5):380–390
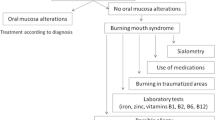
Moghadam-Kia S, Fazel N (2017) A diagnostic and therapeutic approach to primary burning mouth syndrome. Clin Dermatol 35(5):453–460
Coluzzi DJ, Parker S (2017) Lasers in dentistry-current concepts. Springer, New York
Hamblin MR, De Sousa MVP, Agrawal T (2016) Handbook of low level laser therapy. Pan-Stanford Publishing, Singapore
Cronshaw M, Parker S, Arany P (2019) Feeling the heat: evolutionary and microbial basis for the analgesic mechanisms of photobiomodulation therapy. Photobiomodul Photomed Laser Surg 37(9):517–526
Kato IT, Pellegrini VD, Prates RA, Ribeiro MS, Wetter NU, Sugaya NN (2010) Low-level laser therapy in burning mouth syndrome patients: a pilot study. Photomed Laser Surg 28(6):835–839
Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM (2009) Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet 374(9705):1897–1908
Huang Z, Ma J, Chen J, Shen B, Pei F, Kraus VB (2015) The effectiveness of low-level laser therapy for nonspecific chronic low back pain: a systematic review and meta-analysis. Arthritis Res Ther 17:360
Zadik Y, Arany PR, Fregnani ER et al (2019) Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 27:3969–3983
Aras MH, Güngörmüş M (2009) The effect of low-level laser therapy on trismus and facial swelling following surgical extraction of a lower third molar. Photomed Laser Surg 27(1):21–24
Salmos-Brito JA, de Menezes RF, Teixeira CE, Gonzaga RK, Rodrigues BH, Braz R (2013) Evaluation of low-level laser therapy in patients with acute and chronic temporomandibular disorders. Lasers Med Sci 28(1):57–64
Doshi-Mehta G, Bhad-Patil WA (2012) Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofac Orthop 141(3):289–297
Akram Z, Abduljabbar T, Vohra F, Javed F (2018) Efficacy of low-level laser therapy compared to steroid therapy in the treatment of oral lichen planus: a systematic review. J Oral Pathol Med 47(1):11–17
Pozza DH, Fregapani PW, Weber JB et al (2008) Analgesic action of laser therapy (LLLT) in an animal model. Med Oral Patol Oral Cir Bucal 13(10):E648–E652
Pezelj-Ribarić S, Kqiku L, Brumini G et al (2013) Proinflammatory cytokine levels in saliva in patients with burning mouth syndrome before and after treatment with low-level laser therapy. Lasers Med Sci 28(1):297–301
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Spanemberg JC, Segura-Egea JJ, Rodríguez-de Rivera-Campillo E et al (2019) Low-level laser therapy in patients with burning mouth syndrome: a double-blind, randomized, controlled clinical trial. J Clin Exp Dent 11(2):e162–e169
Bardellini E, Amadori F, Conti G, Majorana A (2019) Efficacy of the photobiomodulation therapy in the treatment of the burning mouth syndrome. Med Oral Patol Oral Cir Bucal 24(6):e787–e791
Sikora M, Včev A, Siber S, Vučićević Boras V, Rotim Ž, Matijević M (2018) The efficacy of low-level laser therapy in burning mouth syndrome-a pilot study. Acta Clin Croat 57(2):312–315
Valenzuela S, Lopez-Jornet P (2017) Effects of low-level laser therapy on burning mouth syndrome. J Oral Rehabil 44(2):125–132
Sugaya NN, Silva ÉF, Kato IT, Prates R, Gallo CB, Pellegrini VD (2016) Low intensity laser therapy in patients with burning mouth syndrome: a randomized, placebo-controlled study. Braz Oral Res 30(1):e108
Spanemberg JC, López López J, de Figueiredo MA, Cherubini K, Salum FG (2015) Efficacy of low-level laser therapy for the treatment of burning mouth syndrome: a randomized, controlled trial. J Biomed Opt 20(9):098001
Arbabi-Kalati F, Bakhshani NM, Rasti M (2015) Evaluation of the efficacy of low-level laser in improving the symptoms of burning mouth syndrome. J Clin Exp Dent 7(4):e524–e527
Cui D, Zhang Y (2017) Efficacy of low-level laser therapy in the treatment of burning mouth syndrome. Chinese Journal of Practical Stomatology 10(3):158–162
Arduino PG, Cafaro A, Garrone M et al (2016) A randomized pilot study to assess the safety and the value of low-level laser therapy versus clonazepam in patients with burning mouth syndrome. Lasers Med Sci 31(4):811–816
Barbosa NG, Gonzaga AKG, de Sena Fernandes LL et al (2018) Evaluation of laser therapy and alpha-lipoic acid for the treatment of burning mouth syndrome: a randomized clinical trial. Lasers Med Sci 33(6):1255–1262
Yang JG, Sun P, Liu ZX (2018) Efficacy of ND:YAG laser and mecobalamin in the treatment of burning mouth syndrome. General Journal Of Stomatology 5(36):1–2,8
McKenzie AL, Carruth JA (1984) Lasers in surgery and medicine. Phys Med Biol 29(6):619–641
Périer JM, Boucher Y (2019) History of burning mouth syndrome (1800-1950): a review. Oral Dis 25(2):425–438
Kate RJ, Rubatt S, Enwemeka CS, Huddleston WE (2018) Optimal laser phototherapy parameters for pain relief. Photomed Laser Surg 36(7):354–362
Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR (2012) The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng 40(2):516–533
Carroll JD, Milward MR, Cooper PR, Hadis M, Palin WM (2014) Developments in low level light therapy (LLLT) for dentistry. Dent Mater 30(5):465–475
Acknowledgments
We would like to acknowledge Dr. Cibele Nasri-Heir from Rutgers School of Dental Medicine for her kind help.
Funding
This work was financially supported by the National Natural Science Foundation of China (No. 81570985).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable for this review.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, W., Hu, L., Zhao, W. et al. Effectiveness of photobiomodulation in the treatment of primary burning mouth syndrome–a systematic review and meta-analysis. Lasers Med Sci 36, 239–248 (2021). https://doi.org/10.1007/s10103-020-03109-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03109-9