Abstract
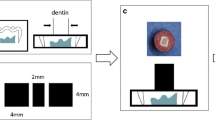
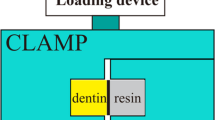
The purpose of this study was to explore the influence of Er:YAG laser irradiation with different pulse durations on the organic matrix, micromorphology of the hybrid layer (HL), and bond strength over time. Sixty caries-free human molars were cut to obtain flat dentin surfaces which were randomly divided into 4 groups: control (not irradiated–G1) and laser groups (80 mJ/2 Hz) with pulse duration ranging between 50 (G2), 300 (G3), and 600 μs (G4). A self-etch adhesive system (Universal 3M ESPE) was applied on pre-treated dentin surfaces and cylinders of resin composite were built up and stressed in a universal testing machine (μSBS) at 24 h and after12 months (n = 12). In addition, 3 other dentin-bonded specimens were prepared as previously described for each group with the adhesive doped with 0.1 wt% Rhodamine B to analyze hybrid layer morphology under Confocal Laser Microscope Scanning (CLMS). Organic matrix and collagen fibrils were analyzed by second harmonic generation (SGH). Two-way ANOVA and Tukey’s test detected significantly higher μSBS values for the control group, whereas the lower values were observed in all laser groups at 24 h (p < 0.05). Storage in artificial saliva did not reduce μSBS in all groups. The low signal emitted by SHG images below the irradiated area demonstrated thermal damage of the collagen matrix. CLMS images of laser groups exhibited thicker and irregular resin-dentin interfaces than the control group. Regardless of the pulse duration, Er:YAG laser pre-treatment altered the organic matrix and HL formation which resulted in low μSBS values at 24 h. The alterations on dentin’s organic structure did not jeopardize the μSBS after 1 year of saliva storage.

Similar content being viewed by others
References
Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P et al (2003) Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent 28:215–235
Karadas M, Çağlar İ (2017) The effect of Er:YAG laser irradiation on the bond stability of self-etch adhesives at diferente dentin depths. Lasers Med Sci 32(5):967–974. https://doi.org/10.1007/s10103-017-2194-x
Gordon LM, Cohen MJ, MacRenaris KW, Pasteris JD, Seda T, Joester D (2015) Dental materials. Amorphous intergranular phases control the properties of rodent tooth enamel. Science 13(347):746–750
Agee KA, Prakki A, Abu-Haimed T, Naguib GH, Nawareg MA, Tezvergil-Mutluay A, Scheffel DL, Chen C, Jang SS, Hwang H, Brackett M, Grégoire G, Tay FR, Breschi L, Pashley DH (2015) Water distribution in dentin matrices: bound vs. unbound water. Dent Mater 31(3):205–116
Li B, Zhu X, Ma L, Wang F, Liu X, Yang X, Zhou J, Tan J, Pashley DH, Tay FR (2016) Selective demineralisation of dentine extrafibrillar minerals-a potential method to eliminate water-wet bonding in the etch-and-rinse technique. J Dent 52:55–62
Frassetto A, Breschi L, Turco G, Marchesi G, Di Lenarda R, Tay FR, Pashley DH, Cadenaro M (2016) Mechanisms of degradation of the hybrid layer in adhesive dentistry and therapeutic agents to improve bond durability –a literature review. Dent Mater 32(2):e41–e53. https://doi.org/10.1016/j.dental.2015.11.007
Carrilho MR, Carvalho RM, De Goes MF, Di Hipolito V, Geraldeli S, Tay FR et al (2007) Chlorhexidine preserves dentinbond in vitro. J Dent Res 86:90–94
Van Meerbeek B, Yoshihara K, Yoshida Y, Mine A, De Munck J, Van Landuyt KL (2011) State of the art of self-etch adhesives. Dent Mater 27:17–28
Tsujimoto A, Barkmeier WW, Takamizawa T, Watanabe H, Johnson WW, Latta MA, Miyazaki M (2017) Comparison between universal adhesives and twostep self-etch adhesives in terms of dentin bond fatigue durability in selfetch mode. Eur J Oral Sci 125:215–222
De Munck J, Van Meerbeek B, Vargas M et al (2005) One day bonding effectiveness of new self-etch adhesives to bur-cut enamel and dentin. Oper Dent 30:39–49
Hanabusa M, Mine A, Kuboki T, Momoi Y, Van Ende A, Van Meerbeek B et al (2012) Bonding effectiveness of a new ‘multi- mode’ adhesive to enamel and dentine. J Dent 40:475–484
Chen C, Niu LN, Xie H, Zhang ZY, Zhou LQ, Jiao K, Chen JH, Pashley DH, Tay FR (2015) Bonding of universal adhesives to dentine--old wine in new bottles? J Dent 43(5):525–536. https://doi.org/10.1016/j.jdent.2015.03.004
Camerlingo C, Lepore M, Gaeta GM, Riccio R, Riccio C, De Rosa A, De Rosa M (2004) Er:YAG laser treatments on dentine surface: micro-Raman spectroscopy and SEM analysis. J Dent 32(5):399–405
Trevelin LT, Marques MM, Aranha AC, Arana-Chavez VE, Matos AB (2015 Jun) Effect of super short pulse Er:YAG laser on human dentin-scanning eléctron microscopy analysis. Microsc Res Tech 78(6):472–478. https://doi.org/10.1002/jemt.22496
Hibst R, Keller U (1989) Experimental studies of the application of the Er: YAG laser on dental hard substances: I. Measurement of the ablation rate. Lasers Surg Med 9(4):338–344
Burkes Junior EJ, Hoke J, Gomes E, Wolbarsht M (1992) Wet versus dry enamel ablation by Er: YAG laser. J Prosthet Dent 67(6):847–851
Eberhard J, Eisenbeiss AK, Braun A, Hedderich J, Jepsen S (2005) Evaluation of selective caries removal by a fluorescence feedback- controlled Er:YAG laser in vitro. Caries Res 39(6):496–504
Kilinc E, Roshkind DM, Antonson SA, Antonson DE, Hardigan PC, Siegel SC, Thomas JW (2009) Thermal safety of Er:YAG and Er, Cr:YSGG lasers in hard tissue removal. Photomed Laser Surg 27(4):565–570
Aranha AC, De Paula EC, Gutknecht N, Marques MM, Ramalho KM, Apel C (2007) Analysis of the interfacial micromorphology of adhesive systems in cavities prepared with Er,Cr:YSGG, Er:YAG laser and bur. Microsc Res Tech 70(8):745–751
Ceballos L, Toledano M, Osorio R, Tay FR, Marshall GW (2002 Feb) Bonding to Er-YAG- laser-treated dentin. J Dent Res 81(2):119–122
Jiang Q, Chen M, Ding J (2013) Comparison of tensile bond strengths of four one-bottle self-etching adhesive systems with Er: YAG laser irradiated dentin. Mol Biol Rep 40:7053–7059
Guven Y, Aktoren O (2015) Shear bond strength and ultrastructural interface analysis of different adhesive systems to Er:YAG laser-prepared dentin. Lasers Med Sci 30:769–778
Brandao CB, Contente MM, De Lima FA et al (2012) Thermal alteration and morphological changes of sound and demineralized primary dentin after Er:YAG laser ablation. Microsc Res Tech 75:126–132
Lukac M, Marko M, Ladislav G (2004) Super VSP Er:YAG pulses for fast and precise cavity preparation. J Oral laser Applic 4:171–173. Medicine 9(4):338–344
Grgurevic J, Grgurevic L, Miletic I, Karlovic Z, Jukic Krmek S, Anic I (2005) In vitro study of the variable square pulse Er: YAG laser cutting efficacy for apicectomy. Lasers Surg Med 5:347–350
Baraba A, Kqiku L, Gabrić D, Verzak Ž, Hanscho K, Miletić I (2018) Efficacy of removal of cariogenic bacteria and carious dentin by ablation using different modes of Er:YAG lasers. Braz J Med Biol Res 51(3):e6872. https://doi.org/10.1590/1414-431X20176872.
Terrer E, Panayotov IV, Slimani A, Tardivo D, Gillet D, Levallois B, Fejerskov O, Gergely C, Cuisinier FJ, Tassery H, Cloitre T (2016) Laboratory studies of nonlinear optical signals for caries detection. J Dent Res 95(5):574–579. https://doi.org/10.1177/0022034516629400
Oelgiesser D, Blasbalg J, Ben-Amar A (2003) Cavity preparation by Er–YAG laser on pulpal temperature rise. Am J Dent 16:96–98
Hossain M, Nakamura Y, Yamada Y, Kimura Y, Nakamura G, Matsumoto K (1999) Ablation depths and morphological changes in human enamel and dentin after Er: YAG laser irradiation with or without water mist. J Clin Laser Med Surg 17(3):105–109
Majaron B, Lukac M, Sustercic D, Funduk N, Skaleric U (1996) Threshold and efficiency analysis in Er:YAG ablation of hard dental tissue. Proc SPIE 2922:233–242
Krmek SJ, Miletic I, Simeon P, Mehicić GP, Anić I, Radisić B (2009) The temperature changes in the pulp chamber during cavity preparation with the Er:YAG laser using a very short pulse. Photomed Laser Surg 27:351–355
Trevelin LT, Silva BT, Arana-Chavez VE, Matos AB (2018) Impact of Er:YAG laser pulse duration on ultrastructure of dentin collagen fibrils.2018. Lasers Dental Sci 15:1–7. https://doi.org/10.1007/s41547-017-0020-1
Firat E, Gurgan S, Gutknecht N (2012) Microtensile bond strength of an etch-and-rinse adhesive to enamel and dentin after Er:YAG laser pretreatment with different pulse durations. Lasers Med Sci 27(1):15–21
He Z, Chen L, Hu X, Shimada Y, Otsuki M, Tagami J, Ruan S (2017) Mechanical properties and molecular structure analysis of subsurface dentin after Er:YAG laser irradiation. J Mech Behav Biomed Mater 74:274–282. https://doi.org/10.1016/j.jmbbm.2017.05.036
Ramos AC, Esteves-Oliveira M, Arana-Chavez VE, de PaulaEduardo C (2010) Adhesives bonded to erbium:yttrium–aluminum– garnet laser-irradiated dentin: transmission electron microscopy, scanning electron microscopy and tensile bond strength analyses. Lasers Med Sci 25(2):181–189
Ferreira LS, Apel C, Francci C, Simoes A, Eduardo CP, Gutknecht N (2010) Influence of etching time on bond strength in dentin irradiated with erbium lasers. Lasers Med Sci 25(6):849–854
Arhun N, Arman A, Sesen C, Karabulut E, Korkmaz Y, Gokalp S (2006) Shear bond strength of orthodontic brackets with 3 self-etch adhesives. Am J Orthod Dentofac Orthop 129:547–550
Nakabayashi N, Pashley DH (1998) Hybridization of dental hard tissues, 1st edn. Quintessence, Tokyo
Bedran-Russo A, Leme-Kraus AA, Vidal CMP, Teixeira EC (2017) An overview of dental adhesives systems and the dynamics tooth-adhesive interface. Dent Clin N Am 61(4):713–731. https://doi.org/10.1016/j.cden.2017.06.001 Review
Yoshida Y, Yoshihara K, Nagaoka N, Hayakawa S, Torii Y, Ogawa T et al (2012) Self-assembled nano-layering at the adhesive interface. J Dent Res 91:376–381
Feitosa VP, Sauro S, Ogliari FA, Ogliari AO, Yoshihara K, Zanchi CH, Correr-Sobrinho L, Sinhoreti MA, Correr AB, Watson TF, Van Meerbeek B (2014 Dec) Impact of hydrophilicity and length of spacer chains on the bonding of functional monomers. Dent Mater 30(12):e317–e323. https://doi.org/10.1016/j.dental.2014.06.006
Tsuchiya K, Takamizawa T, Barkmeier WW, Tsubota K, Tsujimoto A, Berry TP, Erickson RL, Latta MA, Miyazaki M (2016) Effect of a functional monomer (MDP) on the enamel bond durability of single-step self-etch adhesives. Eur J Oral Sci 124(1):96–102
Erhardt MC, Rodrigues JA, Valentino TA, Ritter AV, Pimenta LA (2008a) In vitro microTBS of one-bottle adhesive systems: sound versus artificially-created caries- affected dentin. J Biomed Mater Res B Appl Biomater 86(1):181–187
Akin GE, Herguner-Siso S, Ozcan M, Ozel-Bektas O, Akin H (2012) Bond strengths of one-step self-etch adhesives to laser-irradiated and bur-cut dentin after water storage and thermocycling. Photomed Laser Surg 30(4):214–221
Acknowledgments
The authors would like to thank the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) for the financial support given for the purchase of the laser equipment (Fidelis III-Fotona), Grant # 2015/12651-1.
Funding
This study was funded by FAPESP (2015/12651-1 and 2015/13571-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Human third molars used in this in vitro study followed the approval of the Human Research Ethics Committee of the School of Dentistry of the University of São Paulo, Brazil (Protocol n. 124143/2015).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Trevelin, L.T., da Silva, B.T.F., de Freitas, P.M. et al. Influence of Er:YAG laser pulse duration on the long-term stability of organic matrix and resin-dentin interface. Lasers Med Sci 34, 1391–1399 (2019). https://doi.org/10.1007/s10103-019-02739-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-019-02739-y