Abstract
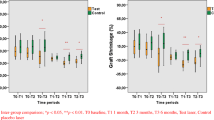
The aim of this clinical study was to compare dimensional changes of the transplanted grafts when the recipient area was prepared with either erbium:yttrium, aluminum, and garnet (Er:YAG) laser or scalpel in free gingival grafts (FGGs). In the first and second groups of ten patients, the recipient area was prepared with an Er:YAG laser and a scalpel, respectively. All grafts were harvested from the palate at standard dimensions (horizontal, 14 mm; vertical, 8 mm). Probing depth, clinical attachment level, and keratinized tissue width were measured before surgery. FGG dimensions (width, length, and area) were measured using the University of North Carolina-15 manual probe (N15) (Nordent Manufacturing, Inc., IL, USA) during surgery and at 10, 21, and 90 days postoperatively. Differences between the two groups were statistically analyzed. In both groups, there was a statistically significant reduction in vertical and horizontal dimensions (p < 0.05) and graft area (p < 0.05) at all time points compared to the baseline measurements. There were no significant differences between the two groups with respect to vertical and horizontal dimensions and graft area at day 90 (p > 0.05). The Er:YAG laser may be used with similar effectiveness as the scalpel in the preparation of the recipient site for free gingival grafts.




Similar content being viewed by others
References
Orban B (1948) Clinical and histologic study of the surface characteristics of the gingiva. Oral Surgery 1:827–841
Gartrell JR, Mathews DP (1976) Gingival recession, the condition, process and treatment. Dent Clin N Am 20:199–213
Schmid MO (1976) The subperiosteal vestibule extension. Literature review, rationale and technique. J West Soc Periodontol 24:89–99
Wennström J, Lindhe J (1983) Role of attached gingiva for maintenance of periodontal health. Healing following excisional and grafting procedures in dogs. J Clin Periodontol 10:206–221
Camargo PM, Melnick PR (2000) Kenney EB (2001) The use of free gingival grafts for aesthetic purposes. Periodontol 27:72–96
Müller HP, Eger T, Schorb A (1998) Gingival dimensions after root coverage with free connective tissue grafts. J Clin Periodontol 25:424–430
Lang NP, Löe H (1972) The relationship between the width of keratinized gingiva and gingival health. J Periodontol 43:623–627
Rossmann JA (2002) Lasers in periodontics. A position paper by the American Academy of Periodontology. J Periodontol 73:1231–1239
Cobb CM (2006) Lasers in periodontics: a review of the literature. J Periodontol 77:545–564
Romeo U, Palaia G, Del Vecchio A, Tenore G, Gambarini G, Gutknecht N, De Luca M (2010) Effects of KTP laser on oral soft tissues. An in vitro study. Lasers Med Sci 25(4):539–543
Badran Z, Boutigny H, Struillou X, Weiss P, Laboux O, Soueidan A (2012) Clinical outcomes after nonsurgical periodontal therapy with an Er:YAG laser device: a randomized controlled pilot study. Photomed Laser Surg 30(7):347–353
Wigdor H, Walsh J, Featherstone JDB et al (1995) Lasers in dentistry. Lasers Surg Med 16:103–133
Bader H (2000) Use of lasers in periodontics. Dent Clin N Am 44:779–792
Israel M (1994) Use of the CO2 laser in soft tissue and periodontal surgery. Pract Periodontics Aesthet Dent 6(6):57–64
Romanos GE (1994) Clinical applications of the Nd:YAG laser in oral soft tissue surgery and periodontology. J Clin Laser Med Surg 12(2):103–108
Zharikov EV, Zhekov VI, Kulevskii LA, Murina TM, Osiko VV, Prokhorov AM, Savel'ev AD, Smirnov VV, Starikov BP, Timoshechkin MI (1975) Stimulated emission from Er3+ ionsin yttrium aluminum garnet crystal at L = 2.94 μ. Sov J Quantum Electron 4(8):1039–1040
Stojan T (2010) 5. 510(k) Summary. http://www.accessdata.fda.gov/cdrh_docs/pdf10/K101817.pdf. Accessed 23 Nov 2012
Spencer P, Cobb CM, Wieliczka DM, Glaros AG, Morris PJ (1998) Change in temperature of subjacent bone during soft tissue laser ablation. J Periodontol 69:1278–1282
Williams TM, Cobb CM, Rapley JW, Killoy WJ (1995) Histologic evaluation of alveolar bone following CO2 laser removal of connective tissue from periodontal defects. Int J Periodontics Restor Dent 15:497–506
Krause LS, Cobb CM, Rapley JW, Killoy WJ (1997) Laser irradiation of bone: an in vitro study concerning the effects of the CO2 laser on oral mucosa and subjacent bone. J Periodontol 68:872–880
Yamaguchi H, Kobayashi K, Reiko O et al (1997) Effects of irradiation of an erbium:YAG laser on root surfaces. J Periodontol 68:1151–1155
Israel M, Cobb CM, Rossmann JA, Spencer P (1997) The effects of the CO2, Nd:YAG and Er:YAG lasers with and without surface coolant on the tooth root surfaces: an in vitro study. J Clin Periodontol 24:595–602
Aoki A, Ando Y, Watanebe H, Ishikawa I (1994) In vitro studies on laser scaling of subgingival calculus with an erbium:YAG laser. J Periodontol 65:1097–1106
Pennel BM, Tabor JC, King KO, Towner JD, Fritz BD, Higgason JD (1969) Free masticatory mucosa graft. J Periodontol 40:162–166
Donoff RB (1976) Biological basis for vestibuloplasty procedures. J Oral Surg 34:890–896
Hatipoğlu H, Keçeli HG, Güncü GN, Şengün D, Tözüm TF (2007) Vertical and horizontal dimensional evaluation of free gingival grafts in the anterior mandible: a case report series. Clin Oral Invest 11:107–113
Silva CO, Ribeiro EP, Sallum AW, Tatakis DN (2010) Free gingival grafts: graft shrinkage and donor-site healing in smokers and non-smokers. J Periodontol 81:692–701
Mörmann W, Schaer F, Firestone AR (1981) The relationship between success of free gingival grafts and transplant thickness. Revascularization and shrinkage—a one year clinical study. J Periodontol 52:74–80
Orsini M, Orsini G, Benlloch D, Aranda JJ, Lazaro P, Sanz M (2004) Esthetic and dimensional evaluation of free connective tissue grafts in prosthetically treated patients: a 1-year clinical study. J Periodontol 75:470–477
Gordon HP, Sullivan HC, Atkins JH (1968) Free autogenous gingival grafts. II. Supplemental findings: histology of the graft site. Periodontics 6:130–133
Sullivan HC, Atkins JH (1968) Free autogenous gingival grafts. III. Utilization of grafts in the treatment of gingival recession. Periodontics 6:152–160
Maynard JG (1977) Coronally positioning of a previously placed autogenous gingival graft. J Periodontol 48:151–155
Visser H, Mausberg R (1996) Free gingival grafts using a CO2 laser: results of a clinical study. J Clin Laser Med Surg 14:85–88
Finkbeiner RL (1995) Free autogenous soft tissue graft with the argon laser. J Clin Laser Med Surg 13:1–5
James WC, McFall WT Jr (1978) Placement of free gingival grafts on denuded alveolar bone. Part I: clinical evaluations. J Periodontol 49:283–290
Dreeskamp M, de Jacoby LF (1973) Breadth of the gingiva propria in vestibuloplasty following gingiva transplantation (in German). Dtsch Zahnarztl Z 28:192–197
Barbosa FI, Corrêa DS, Zenóbio EG, Costa FO, Shibli JA (2009) Dimensional changes between free gingival grafts fixed with ethyl cyanoacrylate and silk sutures. J Int Acad Periodontol 11:170–176
Acknowledgments
The authors thank Gregory T. Sullivan of the School of Foreign Languages at the Ondokuz Mayis University in Samsun, Turkey, for his proofreading.
Conflict of interest
The authors report no conflict of interest related to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Türer, Ç.C., Ipek, H., Kirtiloğlu, T. et al. Dimensional changes in free gingival grafts: scalpel versus Er:YAG laser—a preliminary study. Lasers Med Sci 30, 543–548 (2015). https://doi.org/10.1007/s10103-013-1349-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-013-1349-7