Abstract
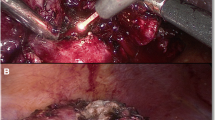
Warm ischemia (WI) and bleeding during laparoscopic partial nephrectomy (LPN) place technical constraints on surgeons. Our aim was to develop a safe and effective laser-assisted LPN-technique without the need for WI. In this study, a diode laser-emitting light at a wavelength of 1,318 nm at output powers between 45 and 70 W in continuous-wave mode was used. Light was coupled into a flexible 600-μm bare fiber to be transported to the tissues. After dry lab experience, 13 patients (six males, seven females) underwent five open and eight laparoscopic/retroperitoneoscopic partial nephrectomies. Postoperative renal function and serum C-reactive protein (CRP) were monitored and coagulation depth and effects on resection margins (RR) were evaluated. Demographic, clinical, and follow-up data are presented. Mean operative time was 116.5 min (range 60–175 min) with mean blood loss of 238 ml (range 50–600 ml). Laser light application took a maximum of 17 min. All patients had a favorable outcome. The locations of the treated tumors (eight left and five right) were central (two), upper pole (two), lower pole (three) and middle kidney parenchyma (six anterior, two posterior, and five peripheral). Mean tumor size was 3.3 cm (range 1.8–5 cm). Two WI (19 and 24 min) were needed. Immediate postoperative serum creatinine and CRP were elevated within 0.1 to 0.6 mg/dl (mean 0.18) and 2.1–10 mg/dl (mean 6.24), respectively. Coagulation depth ranged from <1 to 2 mm without an effect on histopathological evaluation of tumors or RR. One patient had positive RR. During follow-up (2–6 months), one patient developed an A-V fistula that needed embolization. This prospective in-vivo feasibility study showed that the diode laser is a safe and promising device for LPN. Its advantages are minimal gas formation, good hemostasis, and minimal parenchymal damage. Oncological safety appears to be warranted by the use of a diode laser.



Similar content being viewed by others
References
Pantuck AJ, Zisman A, Belldegrun AS (2001) The changing natural history of renal cell carcinoma. J Urol 52:447–450
Chow WH, Devesa SS, Warren JL, Fraumeni JF Jr (1999) Rising incidence of renal cell cancer in the United States. JAMA 281:1628–1631
Lane BR, Gill IS (2007) 5-year outcomes of laparoscopic partial nephrectomy. J Urol 177:70–74
Federico VF, Rolle A, Anile M, Martucci N, Bis B, Rocco G (2010) Techniques used in lung metastasectomy. J Thorac Oncol 5(6) Suppl 2:S145–S150
Rolle A, Pereszlenyi A, Koch R, Bis B, Baier B (2006) Laser resection technique and results of multiple lung metastasectomies using a new 1,318-nm Nd:YAG laser system. Lasers Surg Med 38:26–32
Rolle A, Pereszlenyi A, Koch R, Richard M, Baier B (2006) Is surgery for multiple lung metastases reasonable? A total of 328 consecutive patients with multiple-laser metastasectomies with a new 1,318-nm Nd:YAG laser. J Thorac Cardiovasc Surg 131:1236–1242
Wieliczka DM, Weng S, Querry MR (1989) Wedge-shaped cell for highly absorbent liquids: infrared optical constants of water. Appl Opt 28:1714–1719
Takatani S, Graham MD (1987) Theoretical analysis of diffuse reflectance from a two-layer tissue model. IEEE Trans Biomed Eng BME-26:656–664
Sroka R, Rösler P, Janda P, Grevers G, Leunig A (2000) Endonasal laser surgery with a new laser fibre guidance instrument. Laryngoscope 110:332–334
Campbell SC, Novick AC (2006) Expanding the indications for elective partial nephrectomy: is this advisable? Eur Urol 49:952–954
Porpiglia F, Volpe A, Billia M, Scarpa RM (2008) Laparoscopic versus open partial nephrectomy: analysis of the current literature. Eur Urol 53:732–743
Godoy G, Ramanathan V, Kanofsky JAO, Malley RL, Tareen BU, Taneja SS, Stifelman MD (2009) Effect of warm ischemia time during laparoscopic partial nephrectomy on early postoperative glomerular filtration rate. J Urol 181(6):2438–2443
Abukora F, Nambirajan T, Albqami N, Leeb K, Jeschke S, Gschwendtner M, Janetschek G (2005) Laparoscopic nephron sparing surgery: evolution in a decade. Eur Urol 47:488–493
Gill I, Novick A, Soble J et al (1998) Laparoscopic renal cryoablation: initial clinical series. Urology 52:543–551
Hsu T, Fidler M, Gill I (2000) Radiofrequency ablation of the kidney: acute and chronic histology in porcine model. Urology 56:872–875
Rendon R, Kachura J, Sweet J et al (2002) The uncertainty of radiofrequency treatment of renal cell carcinoma: findings at immediate and delayed nephrectomy. J Urol 167:1587–1592
Desai M, Gill I (2002) Current status of cryoablation and radiofrequency ablation in the management of renal tumors. Curr Opin Urol 12:387–393
Sewell PE, Howard JC, Shingleton WB et al (2003) Interventional magnetic resonance image-guided percutaneous cryoablation of renal tumors. South Med J 96:708–710
Eret V, Hora M, Sykora R, Hes O, Urge T, Klecka J, Matejovic M (2009) GreenLight (532 nm) laser partial nephrectomy followed by suturing of collecting system without renal hilar clamping in porcine model. Urology 73:1115–1118
Bui MH, Breda A, Gui D, Said J, Schulam P (2007) Less and minimal tissue carbonization using a thulium laser for laparoscopic partial nephrectomy without hilar clamping in a porcine model. J Endourol 21:1107–1111
Gruschwitz T, Stein R, Schubert J, Wunderlich H (2008) Laser-supported partial nephrectomy for renal cell carcinoma. Urology 71:334–336
Mattioli S, Muñoz R, Recasens R, Berbegal C, Teichmann H (2008) What does Revolix laser contribute to partial nephrectomy. Arch Esp Urol 61:1126–1129
Gill IS, Matin SF, Desai MM et al (2003) Comparative analysis of laparoscopic versus open partial nephrectomy for renal tumors in 200 patients. J Urol 170:64–68
Gill IS, Kavoussi LR, Lane BR et al (2007) Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. J Urol 178:41–46
Porpiglia F, Volpe A, Billia M, Scarpa RM (2008) Laparoscopic versus open nephrectomy: analysis of the current literature. Eur Urol 53:732–742
Breda A, Stepanian SV, Liao J et al (2007) Positive margins in laparoscopic partial nephrectomy in 855 cases: a multiinstitutional survey from the United States and Europe. J Urol 178:47–50
Frank I, Colombo JR Jr, Rubinstein M, Desai M, Kaouk J, Gill IS (2006) Laparoscopic partial nephrectomy for centrally located renal tumors. J Urol 175:849–852
Seitz M, Reich O, Gratzke C, Schlenker B, Karl A, Bader M, Khoder W, Fischer F, Stief C, Sroka R (2009) High-power diode laser at 980 nm for the treatment of benign prostatic hyperplasia: ex vivo investigations on porcine kidneys and human cadaver prostates. Lasers Med Sci 24:172–178
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Wael Y. Khoder and Ronald Sroka contributed equally to this investigation and manuscript.
Rights and permissions
About this article
Cite this article
Khoder, W.Y., Sroka, R., Hennig, G. et al. The 1,318-nm diode laser supported partial nephrectomy in laparoscopic and open surgery: preliminary results of a prospective feasibility study. Lasers Med Sci 26, 689–697 (2011). https://doi.org/10.1007/s10103-011-0897-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-011-0897-y