Abstract
Objectives
Fusobacterium necrophorum is a common cause of pharyngotonsillitis. However, no guidelines exist on when to diagnose or treat it. We aimed to investigate associations between clinical criteria and F. necrophorum-positivity in pharyngotonsillitis and assess the predictive potential of a simple scoring system.
Methods
Pharyngotonsillitis patients who were tested for F. necrophorum (PCR) and presented to hospitals in the Skåne Region, Sweden, between 2013–2020 were eligible. Data were retrieved from electronic chart reviews and registries. By logistic regression we investigated associations between F. necrophorum-positivity and pre-specified criteria: age 13–30 years, symptom duration ≤ 3 days, absence of viral symptoms (e.g. cough, coryza), fever, tonsillar swelling/exudate, lymphadenopathy and CRP ≥ 50 mg/L. In secondary analyses, associated variables were weighted by strength of association into a score and its predictive accuracy of F. necrophorum was assessed.
Results
Among 561 cases included, 184 (33%) had F. necrophorum, which was associated with the following criteria: age 13–30, symptom duration ≤ 3 days, absence of viral symptoms, tonsillar swelling/exudate and CRP ≥ 50 mg/L. Age 13–30 had the strongest association (OR5.7 95%CI 3.7–8.8). After weighting, these five variables had a sensitivity and specificity of 68% and 71% respectively to predict F. necrophorum-positivity at the proposed cut-off.
Conclusion
Our results suggest that F. necrophorum cases presenting to hospitals might be better distinguished from other pharyngotonsillitis cases by a simple scoring system presented, with age 13–30 being the strongest predictor for F. necrophorum. Prospective studies, involving primary care settings, are needed to evaluate generalisability of findings beyond cases presenting to hospitals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fusobacterium necrophorum is a common pharyngotonsillitis pathogen, found in 21% of pharyngotonsillitis cases overall [1], and in up to 48% of non-streptococcal cases in a study selecting patients aged 18–32 years [2]. Furthermore, a recent study highlighted similar complication rates when F. necrophorum or group A streptococci (GAS) were identified [3] and F. necrophorum is the most frequent cause of peritonsillar abscesses [4]. While the incidence of invasive F. necrophorum disease remains low, including severe manifestations such as Lemierre´s syndrome, it is increasing [5,6,7,8].
In a nationwide study in Sweden, a majority of cases presenting with Lemierre’s syndrome or other severe F. necrophorum infections had a prior medical visit, which rarely resulted in effective antibiotic therapy [6]. Consequently, it could be argued that current guidelines [9,10,11] for testing in tonsillitis may need to be revised, as they barely mention F. necrophorum. However, as of yet, antibiotic efficacy in F. necrophorum pharyngotonsillitis has not been evaluated. In addition, tonsillar carriage rates of F. necrophorum have varied between 0–21% [2, 12,13,14,15,16,17,18] in studies including adolescents and young adults, complicating the interpretation of a positive finding. Nevertheless, the tonsillar carriage rate of GAS (by PCR) in similar age groups have been found to be 9% [12].
When pharyngotonsillitis is suspected, current Swedish practice [9] recommend using the presence of three or more Centor criteria [19] to guide testing with a Rapid antigen detection test (RADT) for GAS. These criteria include a history of fever, tonsillar exudate, cervical lymphadenopathy, and absence of cough [9, 19]. Another common score, the FeverPAIN-score [20], includes fever in the last 24 h, tonsillar exudate, symptom duration ≤ 3 days, severely inflamed tonsils, and absence of cough and coryza, with suggested antibiotic treatment for patients fulfilling four or more criteria [21]. Unsurprisingly, since they were developed to detect beta-haemolytic streptococci [19,20,21], they have been found to have inferior accuracy to detect F. necrophorum [13, 14, 16]. No score has been developed with the purpose to detect F. necrophorum.
The primary aim of this study was to investigate the association of clinically easily available variables with F. necrophorum-positivity among patients with pharyngotonsillitis presenting to hospital. The secondary aim was to investigate the predictive ability of these pre-specified criteria of F. necrophorum-positivity. Their accuracy to predict F. necrophorum were expected to outperform previous criteria developed for beta-haemolytic streptococci in pharyngotonsillitis, e.g., Centor [19] and FeverPAIN-scores [20, 21]. This expectation was partly based on the assumption that among patients referred to hospitals, severe presentations yet with negative RADT, or cases with severe, yet atypical presentations, would be overrepresented, making established criteria less specific.
Method
Study design and setting
In this retrospective study, all pharyngotonsillitis cases tested for F. necrophorum with available medical records in the Skåne Region, Sweden were investigated, limiting cases to those presenting to hospitals due to data availability. All nine hospitals in the region were included in the study, and the population was 1.4 million (2021). The study period ranged from June 2013 until December 2020, encompassing the full period during which F. necrophorum-PCR and registry data were available in this region. Electronic chart reviews were performed in addition to data collection from registries on antibiotic prescriptions, diagnoses and microbiological findings. The study was approved by the local Ethical Review Board in Lund, Sweden (number 2017/971).
Participants
Patients diagnosed with acute pharyngotonsillitis (ICD-10-code J02-03) in any hospital (emergency or outpatient department) and tested with PCR for F. necrophorum were eligible for the study. Patients were excluded if they had a previous (0–30 days) diagnosis of peritonsillar or other pharyngeal abscesses, sinusitis, otitis, chronic pharyngotonsillitis, sepsis or septic complication (ICD-codes in Appendix 1). They were also excluded if they had received antibiotics active against F. necrophorum 1–30 days prior to the visit, defined as beta-lactam antibiotics, metronidazole, or clindamycin, or if misclassification of diagnosis was discovered upon chart review. The follow up period for each patient was 30 days from the index visit. The same person could be included again if at least 30 days had followed since the previous inclusion. All PCR-positive cases for F. necrophorum were defined as F. necrophorum regardless of the presence of a co-infection.
Variables and statistical analysis
The following criteria were pre-specified and associations with F. necrophorum were investigated:
-
Age 13–30 years (0/1)
-
Symptom duration ≤ 3 days (0/1)
-
Absence of common cold symptoms (e.g. cough, coryza, conjunctivitis) (0/1)
-
Fever ≥ 38° C (including anamnestic fever) (0/1)
-
Tonsillar swelling or exudate (0/1)
-
Cervical lymphadenopathy (0/1)
-
CRP ≥ 50 mg/L (0/1)
Variables were chosen a priori, based on literature reviews of known clinical characteristics of patients with bacterial pharyngotonsillitis, including F. necrophorum, and expert opinion [5,6,7, 14, 19, 20, 22]. Information about patient characteristics, symptoms, comorbidities, and microbiological findings were collected from the chart. When defining variables of the Centor and FeverPAIN-scores, absence of cough was equalled to absence of viral symptoms, fever was defined as either measured temperature ≥ 38° or anamnestic fever, and severely inflamed tonsils were defined as tonsillar swelling or exudate. Continuous variables were described as median with interquartile range provided. Dichotomous variables were described as counts and percentages.
As part of the study design, a pilot study including 25 patients was performed to evaluate data quality and data missingness after pre-specifying criteria. Handling of missing data was pre-defined. Clinical signs and symptoms were considered as absent if not described in the chart review. If < 5% were missing for any of the pre-specified criteria, complete case analysis was performed. If ≥ 5% of data were missing (only CRP), multiple imputation (25 iterations) with predictive mean matching (5 nearest neighbours) was performed with a continuous output. Pre-specified variables and F. necrophorum-PCR were used as independent variables. Data were considered missing at random, with similar rates missing in patients regardless of F. necrophorum PCR-positivity. Sensitivity analyses using complete case analysis as comparison were performed. Following multiple imputation of CRP as a continuous variable, estimates from the 25 iterations were dichotomized (≥ 50 mg/L (0/1)) and then pooled.
For the primary analysis, logistic regression analyses were performed to evaluate associations between F. necrophorum-positivity and pre-specified variables, with the reference category being cases with a negative F. necrophorum-PCR. Crude and adjusted odds ratios (OR) were presented. A sensitivity analysis was performed to compare cases with monomicrobial F. necrophorum infection with those with co-infection.
All eligible cases during the period with available data were included, determining the sample size. With seven dichotomous variables (7 degrees of freedom), we expected a sample size with > 15 events per variable included, lowering the risk of overfitting. Statistical analyses were performed using Stata: Release 17.
Secondary analysis
In the secondary analysis, the variables associated with F. necrophorum in the crude analysis were weighted according to strength of association, creating a weighted predictive model, with a simple scoring system. At each point score of this model, its sensitivity, specificity and positive predictive value were tabulated. The predictive model was then assessed against existing scores previously developed to identify beta-haemolytic streptococci, i.e., the Centor [19] and FeverPAIN-scores [20, 21]. The ability of these three predictive models to detect F. necrophorum or any bacterial infection was visualized by ROC-curves and tabulated with suggested cut-offs.
Results
Of a total of 11,748 tests for F. necrophorum performed from throat swabs in the Skåne Region during the study period, 1193 were eligible for the study, since they were performed in pharyngotonsillitis cases who presented to hospitals. 561 were included, with 632 fulfilling exclusion criteria (Fig. 1). 184 (33%) tested positive for F. necrophorum, 95 (17%) tested positive for GAS either by culture or RADT and 88 (16%) tested positive for group C or G streptococci (GCS or GGS). 244 (43%) had no bacterial findings, in 9 of these cases (2% of the total study population), no culture for beta-haemolytic streptococci was performed (Table 1). Of the eligible cases, less than 5% had missing data on symptom duration or throat status and were excluded. CRP levels were missing in 21% and were imputed, dichotomized (≥ 50 mg/L (0/1)), and then pooled.
Flowchart showing the selection process of inclusion of eligible patients by case definition and exclusion criteria for this study, with the microbial findings (F. necrophorum, Group A streptococci (GAS), Group C/G streptococci (GCS/GGS) or no bacterial findings) presented. If more than one finding was made, the case is represented in more than one box. 1 9 cases had missing medical charts, 27 cases had no documented symptom duration, 3 cases had no documented throat status and in 1 case the F. necrophorum sample had not been analysed. 215 cases lacked tonsils (previous tonsillectomy), 4 cases had lingual tonsillitis, 37 cases had a symptom duration of > 14 days
Baseline characteristics
The median age of the patients with F. necrophorum was 21 years. A vast majority was 13–30 years. The age distribution in the GCS/GGS group was similar, while less than half of the patients with GAS were between 13–30 years. A slight majority of the F. necrophorum-positive patients were female and regardless of microbial findings, comorbidities were rare (Table 1).
Primary analysis results
Of the seven pre-specified variables investigated, age 13–30 years (OR 5.7 (95% confidence interval (CI) 3.7–8.8)), symptom duration ≤ 3 days (OR 1.8 (95% CI 1.3–2.7)), absence of viral symptoms (OR 2.2 (95% CI 1.3–3.8)), tonsillar swelling or exudate (OR 3.3 (95% CI 1.8–6.3)) and CRP ≥ 50 mg/L (OR 2.2 (95% CI 1.3–3.6)) were associated with F. necrophorum-positivity in the crude analysis, with age having the strongest association. Lymphadenopathy (OR 1.0 (95% CI 0.7–1.4)) and fever (OR1.3 (95% CI 0.8–1.9)) were not associated with F. necrophorum-positivity. In the multivariate analysis, all associations remained similar (Table 2), and sensitivity analyses had similar results (Appendix 2, Tables 1, 2, 3, 4).
Secondary analyses
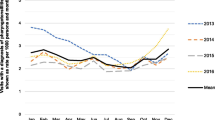
For the scoring system, variables associated with F. necrophorum were weighted by strength of association. Age 13–30 years was assigned 3 points, while symptom duration ≤ 3 days, absence of viral symptoms, tonsillar swelling or exudate and CRP ≥ 50 mg/L were assigned one point each with a maximum of seven points (Table 2). Sensitivity and specificity to detect F. necrophorum were calculated at each point-score. At a cut-off level of six points in this cohort, the F. necrophorum-prevalence (positive predictive value) was 53% above and 18% below. As expected, lower positive predictive values were seen for Centor criteria and FeverPAIN-score (Table 3), which performed worse at identifying both F. necrophorum or any bacterial infection (Fig. 2).
Discussion
We investigated signs and symptoms in hospital cases with F. necrophorum-pharyngotonsillitis to describe how their presentation may distinguish them from patients with other causes of pharyngotonsillitis. Of seven pre-specified variables, five were associated with F. necrophorum-PCR-positivity, i.e., age 13–30 years, symptom duration of ≤ 3 days, absence of viral symptoms, tonsillar swelling or exudate and CRP ≥ 50 mg/L. After weighting criteria by strengths of associations, a predictive model was evaluated and at a cut-off of six or more of seven points, every second patient with pharyngotonsillitis had a positive F. necrophorum-PCR.
The variables investigated were inspired by previous studies [1, 14] and scores used in pharyngotonsillitis, yet varied slightly from the Centor [19] and FeverPAIN-scores [20, 21] suggesting that F. necrophorum could be distinguished from other causes of pharyngotonsillitis. Most importantly, the age criterion was the strongest predictor of F. necrophorum, suggesting that focusing on adolescents and young adults is advisable in future guidelines on F. necrophorum-pharyngotonsillitis, specifically in RADT-negative cases presenting to hospital. No randomized controlled trial has investigated antibiotic therapy in F. necrophorum-pharyngotonsillitis. Yet, a Cochrane meta-analysis on antibiotic treatment in pharyngotonsillitis patients with negative cultures for beta-haemolytic streptococci have shown symptom reduction following exposure to antibiotics [24]. It is conceivable that this could also apply to F. necrophorum, although studies are needed.
No previous criteria have been developed to predict F. necrophorum. However, the performance of the Centor criteria in predicting F. necrophorum pharyngotonsillitis has previously been summarized in a meta-analysis by Klug et al [1], focused on three prospective studies with low risk of bias performed in a primary care setting [13, 14, 16]. Based on data from this meta-analysis, a cut-off of three or more Centor criteria would only identify 30% of patients with F. necrophorum. Conversely, in the large data set presented in our study, 80% of patients with F. necrophorum had three or more Centor criteria. Presumably, among the patients referred to hospital in this study, many likely had high Centor criteria, negative RADT, yet severe or atypical presentations. Consequently, regardless of microbiological findings, most patients enrolled in our study had Centor criteria of three or more (72%). Hence, in our cohort of hospital cases the Centor criteria had a low positive predictive value due to low specificity (Table 3). First, this highlight that our data represent a severely ill pharyngotonsillitis cohort, most with high Centor scores. Second, given the retrospective nature of data, selection bias is likely to occur since current practice in Sweden [9] (focused on Centor criteria) will likely select cases with high Centor criteria or severely ill cases for further testing despite a negative RADT. The previously cited meta-analysis [1] highlights that Centor criteria perform worse in detecting F. necrophorum efficiently when compared to GAS in the primary health care setting. Our study shows that the Centor and FeverPAIN scores have worse performance to predict F. necrophorum among hospital cases compared to our proposed criteria, yet we can draw no firm conclusions on their performance in the primary care setting. As neither were developed to predict F. necrophorum, this is expected, yet indicates the need for a different tool to decide whom to test for F. necrophorum. The findings of this paper should encourage the validation of our score, which shows promise among cases presenting to hospital. However, its sensitivity and specificity of 68 and 71% highlights room for improvement. Meanwhile, meta-analyses of validation studies on criteria used to identify GAS in pharyngotonsillitis have similarly shown moderate accuracy in both primary care [25] and hospitals [26]. Nevertheless, these criteria remain useful. Importantly, due to the known asymptomatic tonsillar carriage of F. necrophorum and GAS [12, 18], the aim of clinical criteria in pharyngotonsillitis should not be to identify all cases positive for F. necrophorum or GAS, but preferably target cases most likely to benefit from treatment.
There are several limitations to this study. As stated, it suffers from selection bias since it only includes patients presenting to hospital. In Swedish practice pharyngotonsillitis patients with three or more Centor criteria are recommended to be tested with a RADT for GAS [9]. Extensive diagnostics for other beta-haemolytic streptococci or F. necrophorum is mentioned in severely ill patients or patients with persistent or worsening symptoms after three days. Hence, the patients in this study are both selected since they present to hospital and since the case definition requires testing. In addition, most patients testing positive for GAS using RADT would likely not have been tested any further, decreasing the number of GAS-patients included. Thus, generalizability of the findings is limited to severe and mainly RADT-negative pharyngotonsillitis cases presenting to hospital. Nonetheless, these are the patients where current practice recommendations [9] mention extended diagnostics beyond an RADT. Important to note, the reference category in regression analyses is defined by a negative F. necrophorum-PCR, and not negative results for any bacteria, since the aim was to distinguish F. necrophorum-pharyngotonsillitis from all other causes, including beta-haemolytic streptococci. By highlighting distinctive features of F. necrophorum pharyngotonsillitis in a large number of severely ill cases with pharyngotonsillitis, future guidelines are aided to provide better guidance, with the main predictor being age 13–30 years. Guidelines on management of pharyngotonsillitis might need revision following evidence during the last ten years establishing F. necrophorum as an important cause of pharyngotonsillitis [1, 3], peritonsillar abscess [4, 27] and with increasing incidence of invasive infections in adolescents and young adults [6].
Future prospective studies are needed to investigate associations of these and other clinically easily available variables to predict F. necrophorum-positivity. Preferably, studies should be performed in a primary care population, where most cases of pharyngotonsillitis present. It is likely that the sensitivity of the predictive model here discussed will decrease considerably if used in a less severely ill population and would likely require lower cut-offs or potentially investigate other variables. Nevertheless, in the sub-group of patients with severe pharyngotonsillitis and negative RADT for GAS, signs and symptoms presented here could help guide physicians on whom to test for F. necrophorum. Investigating whether treatment leads to reduced symptoms and complications remains necessary, as do the development of more easily available tests for F. necrophorum, preferably an RADT.
Given the increased acknowledgement and importance of F. necrophorum in pharyngotonsillitis in high-income countries, guidance on whom and when to test for it is needed. In a large but selected cohort of severe cases of pharyngotonsillitis presenting to hospital, age between 13–30 was identified as the strongest predictor of F. necrophorum-positivity, followed by tonsillar swelling or exudate, CRP ≥ 50 mg/L, absence of viral symptoms and symptom duration ≤ 3 days. When used to predict presence of F. necrophorum, these easily available clinical characteristics outperformed previous established criteria, but need to be investigated and likely finetuned in primary health care populations prior to clinical use.
Data availability
According to the ethical approval by the Ethical Review Board in Lund, Sweden (number 2017/971) data is not allowed to be shared publicly. For specific questions regarding the data, please contact the authors.
Code availability
Not applicable.
References
Klug TE, Rusan M, Fuursted K, Ovesen T, Jorgensen AW (2016) A systematic review of Fusobacterium necrophorum-positive acute tonsillitis: prevalence, methods of detection, patient characteristics, and the usefulness of the Centor score. Eur J Clin Microbiol Infect Dis 35(12):1903–1912. https://doi.org/10.1007/s10096-016-2757-y
Jensen A, HagelskjaerKristensen L, Prag J (2007) Detection of Fusobacterium necrophorum subsp. funduliforme in tonsillitis in young adults by real-time PCR. Clin Microbiol Infect. 13(7):695–701. https://doi.org/10.1111/j.1469-0691.2007.01719.x
Nygren D, Wasserstrom L, Holm K, Torisson G (2023) Associations Between Findings of Fusobacterium necrophorum or β-Hemolytic Streptococci and Complications in Pharyngotonsillitis-A Registry-Based Study in Southern Sweden. Clin Infect Dis 76(3):e1428–e1435. https://doi.org/10.1093/cid/ciac736
Klug TE, Rusan M, Fuursted K, Ovesen T (2009) Fusobacterium necrophorum: most prevalent pathogen in peritonsillar abscess in Denmark. Clin Infect Dis 49(10):1467–1472. https://doi.org/10.1086/644616
Brazier JS, Hall V, Yusuf E, Duerden BI (2002) Fusobacterium necrophorum infections in England and Wales 1990–2000. J Med Microbiol 51(3):269–272. https://doi.org/10.1099/0022-1317-51-3-269
Nygren D, Holm K (2020) Invasive infections with Fusobacterium necrophorum including Lemierre’s syndrome: an 8-year Swedish nationwide retrospective study. Clin Microbiol Infect. 26(8):1089.e7-.e12. https://doi.org/10.1016/j.cmi.2019.12.002
HagelskjaerKristensen L, Prag J (2008) Lemierre’s syndrome and other disseminated Fusobacterium necrophorum infections in Denmark: a prospective epidemiological and clinical survey. Eur J Clin Microbiol Infect Dis 27(9):779–789. https://doi.org/10.1007/s10096-008-0496-4
Riordan T (2007) Human infection with Fusobacterium necrophorum (Necrobacillosis), with a focus on Lemierre’s syndrome. Clin Microbiol Rev 20(4):622–659. https://doi.org/10.1128/cmr.00011-07
(2012) Handläggning av faryngotonsilliter i öppenvård – ny rekommendation. Information från Läkemedelsverket 23(6):18–25. Available at www.lakemedelsverket.se, document in Swedish
Pelucchi C, Grigoryan L, Galeone C, Esposito S, Huovinen P, Little P et al (2012) Guideline for the management of acute sore throat. Clin Microbiol Infect 18(Suppl 1):1–28. https://doi.org/10.1111/j.1469-0691.2012.03766.x
Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G et al (2012) Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis 55(10):e86-102. https://doi.org/10.1093/cid/cis629
Agerhäll M, Henrikson M, Johansson Söderberg J, Sellin M, Tano K, Gylfe Å et al (2021) High prevalence of pharyngeal bacterial pathogens among healthy adolescents and young adults. APMIS 129(12):711–716. https://doi.org/10.1111/apm.13179
Centor RM, Atkinson TP, Ratliff AE, Xiao L, Crabb DM, Estrada CA et al (2015) The clinical presentation of Fusobacterium-positive and streptococcal-positive pharyngitis in a university health clinic: a cross-sectional study. Ann Intern Med 162(4):241–247. https://doi.org/10.7326/m14-1305
Hedin K, Bieber L, Lindh M, Sundqvist M (2015) The aetiology of pharyngotonsillitis in adolescents and adults - Fusobacterium necrophorum is commonly found. Clin Microbiol Infect 21(3):263.e1–7. https://doi.org/10.1016/j.cmi.2014.08.020
Jensen A, Hansen TM, Bank S, Kristensen LH, Prag J (2015) Fusobacterium necrophorum tonsillitis: an important cause of tonsillitis in adolescents and young adults. Clin Microbiol Infect 21(3):266.e1–3. https://doi.org/10.1016/j.cmi.2014.09.020
Kjærulff AM, Thomsen MK, Ovesen T, Klug TE (2015) Clinical and biochemical characteristics of patients with Fusobacterium necrophorum-positive acute tonsillitis. Eur Arch Otorhinolaryngol 272(6):1457–1463. https://doi.org/10.1007/s00405-015-3535-7
Ludlam H, Howard J, Kingston B, Donachie L, Foulkes J, Guha S et al (2009) Epidemiology of pharyngeal carriage of Fusobacterium necrophorum. J Med Microbiol 58(Pt 9):1264–1265. https://doi.org/10.1099/jmm.0.006718-0
Nygren D, Brorson E, Musonda M, Wasserstrom L, Johansson Å, Holm K (2021) Geographical differences in tonsillar carriage rates of Fusobacterium necrophorum - A cross-sectional study in Sweden and Zambia. Anaerobe 69:102360. https://doi.org/10.1016/j.anaerobe.2021.102360
Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K (1981) The diagnosis of strep throat in adults in the emergency room. Med Decis Making 1(3):239–246. https://doi.org/10.1177/0272989x8100100304
Little P, Moore M, Hobbs FD, Mant D, McNulty C, Williamson I et al (2013) PRImary care Streptococcal Management (PRISM) study: identifying clinical variables associated with Lancefield group A β-haemolytic streptococci and Lancefield non-Group A streptococcal throat infections from two cohorts of patients presenting with an acute sore throat. BMJ Open 3(10):e003943. https://doi.org/10.1136/bmjopen-2013-003943
Little P, Hobbs FD, Moore M, Mant D, Williamson I, McNulty C et al (2013) Clinical score and rapid antigen detection test to guide antibiotic use for sore throats: randomised controlled trial of PRISM (primary care streptococcal management). BMJ 347:f5806. https://doi.org/10.1136/bmj.f5806
Bank S, Jensen A, Nielsen HM, Kristensen LH, Voldstedlund M, Prag J (2016) Fusobacterium necrophorum findings in Denmark from 2010 to 2014 using data from the Danish microbiology database. APMIS 124(12):1087–1092. https://doi.org/10.1111/apm.12606
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Spinks A, Glasziou PP, Del Mar CB (2021) Antibiotics for treatment of sore throat in children and adults. Cochrane Database Syst Rev 12(12):Cd000023. https://doi.org/10.1002/14651858.CD000023.pub5
Willis BH, Coomar D, Baragilly M (2020) Comparison of Centor and McIsaac scores in primary care: a meta-analysis over multiple thresholds. Br J Gen Pract 70(693):e245–e254. https://doi.org/10.3399/bjgp20X708833
Kanagasabai A, Evans C, Jones HE, Hay AD, Dawson S, Savović J et al (2024) Systematic review and meta-analysis of the accuracy of McIsaac and Centor score in patients presenting to secondary care with pharyngitis. Clin Microbiol Infect 30(4):445–452. https://doi.org/10.1016/j.cmi.2023.12.025
Klug TE, Greve T, Caulley L, Hillerup S (2023) The impact of social restrictions on the incidence and microbiology of peritonsillar abscess: a retrospective cohort study. Clin Microbiol Infect. https://doi.org/10.1016/j.cmi.2023.08.003
Acknowledgements
We are grateful to Lena Hyllebusk at the Department of Clinical Microbiology, Infection Control and Prevention, Skåne University Hospital, Lund for assistance in data retrieval. We are also grateful to Jon Pallon at the Department of Research and Development, Region Kronoberg, Växjö for valuable discussions during the conduct of this study.
Funding
Open access funding provided by Lund University. This work was supported by the Swedish Government Funds for Clinical Research (ALF) and Region Skåne.
Author information
Authors and Affiliations
Contributions
Contributions to the paper are described as following: Writing – Original Draft: Josefina Pagels and David Nygren; Writing – Review & Editing: Josefina Pagels, David Nygren, Gustav Torisson, Karin Holm, Lisa Wasserstrom and Katarina Hedin; Conceptualization: David Nygren, Gustav Torisson and Karin Holm; Investigation: Josefina Pagels, David Nygren and Karin Holm; Methodology: David Nygren and Gustav Torisson; Formal Analysis: Josefina Pagels and David Nygren; Project Administration: Karin Holm and David Nygren; Funding Acquisition: Karin Holm and David Nygren.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the local Ethical Review Board in Lund, Sweden (number 2017/971).
Consent to participate
The requirement of consent to participate was waived by the ethical review board (number 2017/971).
Consent to publish
The requirement of consent to publish was waived by the ethical review board (number 2017/971).
Conflicts of interest
None of the authors have conflicting interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Preliminary results from the study were presented at the ESCMID conference in Copenhagen, Denmark on the 15th of April 2023.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pagels, J., Torisson, G., Wasserstrom, L. et al. Symptoms predictive of Fusobacterium necrophorum pharyngotonsillitis – an observational study of cases presenting to hospitals in Southern Sweden. Eur J Clin Microbiol Infect Dis (2024). https://doi.org/10.1007/s10096-024-04827-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10096-024-04827-6