Abstract
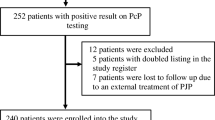
In the non-AIDS group, several underlying conditions and immune defects could lead to different PCP presentations. This study compared PCP presentation and outcome according to the underlying disease. A secondary analysis of a previously published prospective observational study including 544 PCP patients was done. Only non-AIDS patients were included. Underlying disease was defined as chronic lymphocytic leukemia (CLL), organ transplantation, solid cancer, allogeneic hematopoietic stem cell transplant (AHSCT), other hematological diseases, and immunosuppressive treatment. Clinical characteristics and outcomes were compared between groups. Multiple correspondent analyses compared clinical characteristics at diagnosis. Day 30 mortality was analyzed. Three hundred and twenty-one patients were included in the study. The underlying diseases were hematological malignancy (n = 75), AHSCT (n = 14), CLL (n = 19), solid organ transplant (n = 94), solid tumor (n = 39), and immunosuppressive treatment (n = 57). Compared with other underlying diseases, PCP related to CLL was closer to PCP related to AIDS presentation (long duration of symptoms before diagnosis, high level of dyspnea, and low oxygen saturation at diagnosis). Day 30 mortality was associated with underlying disease, oxygen flow, and shock at ICU admission. PCP presentations may vary according to the underlying reason for immunosuppression. Response to treatment and adjuvant steroid therapy should be analyzed regarding this result.


Similar content being viewed by others
Data availability
Data are available on reasonable request required because of observational study.
References
Bollée G, Sarfati C, Thiéry G, Bergeron A, de Miranda S, Menotti J et al (2007) Clinical picture of Pneumocystis jiroveci pneumonia in cancer patients. Chest 132:1305–1310
Gonzalez Santiago TM, Wetter DA, Kalaaji AN, Limper AH, Lehman JS (2016) Pneumocystis jiroveci pneumonia in patients treated with systemic immunosuppressive agents for dermatologic conditions: a systematic review with recommendations for prophylaxis. Int J Dermatol 55:823–830
Matsumoto T, Fujita M, Hirano R, Sasaki T, Watanabe K (2019) Risk factors for pneumocystis pneumonia onset in HIV-negative patients treated with high-dose systemic corticosteroids. Infect Dis (Lond) 51:305–307
Park SY, Jung JH, Kwon H, Shin S, Kim YH, Chong Y et al (2020) Epidemiology and risk factors associated with Pneumocystis jirovecii pneumonia in kidney transplant recipients after 6-month trimethoprim-sulfamethoxazole prophylaxis: a case-control study. Transpl Infect Dis 22(2):e13245
Watanabe H, Kitahara Y, Murakami Y, Nihashi F, Matsushima S, Eifuku T et al (2020) Pneumocystis jirovecii pneumonia in a patient with breast cancer receiving neoadjuvant dose-dense chemotherapy. Intern Med 59:987–990
Roux A, Canet E, Valade S, Gangneux-Robert F, Hamane S, Lafabrie A et al (2014)Pneumocystis jirovecii pneumonia in patients with or without AIDS, France. Emerg Infect Dis 20:1490–1497
Monnet X, Vidal-Petiot E, Osman D, Hamzaoui O, Durrbach A, Goujard C et al (2008) Critical care management and outcome of severe Pneumocystis pneumonia in patients with and without HIV infection. Crit Care 12:R28
Festic E, Gajic O, Limper AH, Aksamit TR (2005) Acute respiratory failure due to pneumocystis pneumonia in patients without human immunodeficiency virus infection: outcome and associated features. Chest 128:573–579
Gassner FJ, Weiss L, Geisberger R, Hofbauer JP, Egle A, Hartmann TN et al (2011) Fludarabine modulates composition and function of the T cell pool in patients with chronic lymphocytic leukaemia. Cancer Immunol Immunother 60:75–85
Thomas CF, Limper AH (2007) Current insights into the biology and pathogenesis of Pneumocystis pneumonia. Nat Rev Microbiol 5:298–308
Werbel WA, Ison MG, Angarone MP, Yang A, Stosor V (2018) Lymphopenia is associated with late onset Pneumocystis jirovecii pneumonia in solid organ transplantation. Transpl Infect Dis 20:e12876
Pagano L, Fianchi L, Leone G (2006) Fungal pneumonia due to molds in patients with hematological malignancies. J Chemother 18:339–352
Tasaka S, Tokuda H (2012) Pneumocystis jirovecii pneumonia in non-HIV-infected patients in the era of novel immunosuppressive therapies. J Infect Chemother 18:793–806
Gaborit BJ, Tessoulin B, Lavergne R-A, Morio F, Sagan C, Canet E et al (2019) Outcome and prognostic factors of Pneumocystis jirovecii pneumonia in immunocompromised adults: a prospective observational study. Ann Intensive Care 9:131
Thomas CF, Limper AH (2004) Pneumocystis pneumonia. N Engl J Med 350:2487–2498
Nandakumar V, Hebrink D, Jenson P, Kottom T, Limper AH (2017) Differential macrophage polarization from Pneumocystis in immunocompetent and immunosuppressed hosts: potential adjunctive therapy during pneumonia. Infect Immun 85(3):e00939-16
Moon SM, Kim T, Sung H, Kim M-N, Kim S-H, Choi S-H et al (2011) Outcomes of moderate-to-severe Pneumocystis pneumonia treated with adjunctive steroid in non-HIV-infected patients. Antimicrob Agents Chemother 55:4613–4618
Wieruszewski PM, Barreto JN, Frazee E, Daniels CE, Tosh PK, Dierkhising RA et al (2018) Early corticosteroids for Pneumocystis pneumonia in adults without HIV are not associated with better outcome. Chest 154:636–644
Borcoman E, Dupont A, Mariotte E, Doucet L, Joseph A, Chermak A et al (2020) One-year survival in patients with solid tumours discharged alive from the intensive care unit after unplanned admission: a retrospective study. J Crit Care 57:36–41
Fishman JA, Gans H (2019) AST Infectious Diseases Community of Practice. Pneumocystis jiroveci in solid organ transplantation: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transpl 33:e13587
Funding
The initial cohort was supported by a grant from the French ministry of health.
Author information
Authors and Affiliations
Contributions
GB, LB, EA, and VL designed the study, performed analysis, and wrote the manuscript. AR, SV, FRG, SH, DM, AD, SLG, FD, ML, DT, CP, APB, JB, AB, XI, IDJ, DM, DP, CH, and EM included patients, and reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The appropriate ethics committee approved the first study.
Consent to participate
Non-applicable
Consent to publish
Non-applicable
Informed consent
It was not required because of observational study.
Competing interests
Antoine Roux, MD,; Sandrine Valade, MD; Florence Gangneux-Robert, PharmD, PhD; Samia Hamane, MD; Daniele Maubon, MD, PhD; Anne Debourgogne, PhD, MPH; Solène Le Gal, DVM, PhD; Frederic Dalle, PharmD, PhD; Marion Leterrier, PharmD; Dominique Toubas, MD, PhD; Christelle Pomares, MD, PhD; Anne Pauline Bellanger, PharmD, PhD; Julie Bonhomme, MD, PhD; Xavier Iriart, PhD; Isabelle Durand-Joly, PhD; Denis Magne, PhD; Denis Pons, Pharmacien Biologiste; and Eric Maury, MD, PhD, have disclosed no relevant financial relationships. Christophe Hennequin, MD, PhD, has disclosed the following relevant financial relationships: served as an advisor or consultant for Gilead Sciences, Inc., Merck Sharp & Dohme Corp; Pfizer Inc. Elie Azoulay, MD, PhD, has disclosed the following relevant financial relationships: Gilead Sciences, Pfizer, Astellas, Alexion, Fisher-Paykel. Dr. Lemiale has disclosed being memeber of a research group which received grant from Pfizer, Fisher-Paykel, Gilead, Alexion, Astellas.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 33 kb)
Rights and permissions
About this article
Cite this article
Burghi, G., Biard, L., Roux, A. et al. Characteristics and outcome according to underlying disease in non-AIDS patients with acute respiratory failure due to Pneumocystis pneumonia. Eur J Clin Microbiol Infect Dis 40, 1191–1198 (2021). https://doi.org/10.1007/s10096-020-04118-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-020-04118-w