Abstract
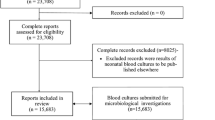
We investigated the clinical implications of the practice in our emergency department (ED) of discharging patients with pending blood cultures. We reviewed the medical records of adults discharged with positive blood cultures from the ED of a 330-bed university hospital during a five-year period. Clinical characteristics, laboratory data, and antibiotic treatment prescribed in the ED and at discharge were accessed. Antimicrobial susceptibility profiles were used to determine whether antibiotic treatment was adequate. The outcomes assessed for 90 days following discharge were return to the ED, hospitalization, modified diagnosis, and death. Of 220,681 visits to the ED, 1362 showed positive blood cultures; of these, 307 (22.5%) were from discharged patients. More than half the isolates (56.3%) were considered contaminants. Of 124 visits with true bacteremia, Enterobacteriaceae were the most common pathogens (67.0%). This is concordant with urinary tract infection (UTI) being the most common diagnosis (52.4%). With antibiotic treatment, 69.4% had been discharged with antibiotic treatment, which was adequate in two-thirds of them. Among the 77 who returned to the ED, 27.5% had persistent bacteremia. The diagnosis was changed in 44.2% of them, mostly with brucellosis or bone and joint infections, and 84.4% were subsequently hospitalized. Within three months, 5.6% of bacteremic patients died, all after hospitalization. Bacteremia in discharged patients occurred mainly in association with UTI. Outcomes were generally favorable, although only about half received appropriate antibiotic treatment. Diagnoses were changed in a relatively high proportion of patients following culture results.


Similar content being viewed by others
Abbreviations
- CT:
-
computer tomography
- ED:
-
emergency department
- WBC:
-
white blood count.
References
Brown JD, Chapman S, Ferguson PE (2017) Blood cultures and bacteraemia in an Australian emergency department: evaluating a predictive rule to guide collection and their clinical impact. Emerg Med Australas 29:56–62. https://doi.org/10.1111/1742-6723.12696
CDC (2019) Bloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-central Line Associated Bloodstream Infection). https://www.cdc.gov/nhsn/pdfs/pscmanual/4psc_clabscurrent.pdf
Chan J, Wong J, Saginur R, Forster AJ, van Walraven C (2015) Epidemiology and outcomes of bloodstream infections in patients discharged from the emergency department. Cjem 17:27–37. https://doi.org/10.2310/8000.2013.131349
CLSI (2017) M100: performance standards for antimicrobial susceptibility testing. http://www.facm.ucl.ac.be/intranet/CLSI/CLSI-2017-M100-S27.pdf
Coburn B, Morris AM, Tomlinson G, Detsky AS (2012) Does this adult patient with suspected bacteremia require blood cultures? Jama 308:502–511. https://doi.org/10.1001/jama.2012.8262
Dempsey C, Skoglund E, Muldrew KL, Garey KW (2019) Economic health care costs of blood culture contamination: a systematic review. Am J Infect Control. https://doi.org/10.1016/j.ajic.2018.12.020
Epstein D, Raveh D, Schlesinger Y, Rudensky B, Gottehrer NP, Yinnon AM (2001) Adult patients with occult bacteremia discharged from the emergency department: epidemiological and clinical characteristics. Clin Infect Dis 32:559–565. https://doi.org/10.1086/318699
Fu CM, Tseng WP, Chiang WC, Lai MS, Chie WC, Chou HC, Hsueh PR, Ma MH, Fang CC, Chen SC, Chen WJ, Chen SY (2012) Occult staphylococcus aureus bacteremia in adult emergency department patients: rare but important. Clin Infect Dis 54:1536–1544. https://doi.org/10.1093/cid/cis214
Gonzalez-Del Vecchio M, Bunsow E, Sanchez-Carrillo C, Garcia Leoni E, Rodriguez-Creixems M, Bouza E (2014) Occult bloodstream infections in adults: a "benign" entity. Am J Emerg Med 32:966–971. https://doi.org/10.1016/j.ajem.2014.05.007
Jessen MK, Mackenhauer J, Hvass AM, Ellermann-Eriksen S, Skibsted S, Kirkegaard H, Schonheyder HC, Shapiro NI (2016) Prediction of bacteremia in the emergency department: an external validation of a clinical decision rule. Eur J Emerg Med 23:44–49. https://doi.org/10.1097/mej.0000000000000203
Kamin Y, Steinberg JM, Kafka M, Hussein A, Srugo I (2003) Is there a need for taking blood cultures from febrile adults discharged from the emergency department? In: J infect, vol 46. Vol 1. England, pp 72-73
Lin CT, Lu JJ, Chen YC, Kok VC, Horng JT (2017) Diagnostic value of serum procalcitonin, lactate, and high-sensitivity C-reactive protein for predicting bacteremia in adult patients in the emergency department. PeerJ 5:e4094. https://doi.org/10.7717/peerj.4094
Long B, Koyfman A (2016) Best clinical practice: blood culture utility in the emergency department. J Emerg Med 51:529–539. https://doi.org/10.1016/j.jemermed.2016.07.003
Mountain D, Bailey PM, O'Brien D, Jelinek GA (2006) Blood cultures ordered in the adult emergency department are rarely useful. Eur J Emerg Med 13:76–79. https://doi.org/10.1097/01.mej.0000188231.45109.ec
Ramos JM, Masia M, Elia M, Gutierrez F, Royo G, Bonilla F, Padilla S, Martin-Hidalgo A (2004) Epidemiological and clinical characteristics of occult bacteremia in an adult emergency department in Spain: influence of blood culture results on changes in initial diagnosis and empiric antibiotic treatment. Eur J Clin Microbiol Infect Dis 23:881–887. https://doi.org/10.1007/s10096-004-1235-0
Stalnikowicz R, Block C (2001) The yield of blood cultures in a department of emergency medicine. Eur J Emerg Med 8:93–97
Sturmann KM, Bopp J, Molinari D, Akhtar S, Murphy J (1996) Blood cultures in adult patients released from an urban emergency department: a 15-month experience. Acad Emerg Med 3:768–775
Takeshima T, Yamamoto Y, Noguchi Y, Maki N, Gibo K, Tsugihashi Y, Doi A, Fukuma S, Yamazaki S, Kajii E, Fukuhara S (2016) Identifying patients with bacteremia in community-hospital emergency rooms: a retrospective cohort study. PLoS One 11:e0148078. https://doi.org/10.1371/journal.pone.0148078
Zafar Iqbal-Mirza S, Serrano Romero de Avila V, Estevez-Gonzalez R, Rodriguez-Gonzalez D, Heredero-Galvez E, Julian-Jimenez A (2019) Ability of procalcitonin to differentiate true bacteraemia from contaminated blood cultures in an emergency department. Enferm Infecc Microbiol Clin. https://doi.org/10.1016/j.eimc.2019.01.012
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the local Institutional Review Board.
Informed consent
The requirement for informed consent was waived since the study was based on anonymized data collected retrospectively.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meetings
The work was presented as an oral presentation at the ECCMID (European Congress of Clinical Microbiology & Infectious Diseases) in Amsterdam, Netherlands, on April 16th 2019. It was also presented as an oral presentation at the annual meeting of the Israel Emergency Medicine Society in Tel Aviv, Israel, March 2019; and was awarded the best poster at the annual meeting of the Israel Infectious Diseases Society in Kfar Blum, Israel, May 2019. It was presented as well as an oral presentation at the MEMC19 (Mediterranean Emergency Medicine Congress) in Dubrovnik, Croatia, September 2019.
Electronic supplementary material
ESM 1
(DOCX 26 kb)
Rights and permissions
About this article
Cite this article
Kenig, A., Salameh, S., Gershinsky, Y. et al. Blood cultures of adult patients discharged from the emergency department—is the safety net reliable?. Eur J Clin Microbiol Infect Dis 39, 1261–1269 (2020). https://doi.org/10.1007/s10096-020-03838-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-020-03838-3