Abstract
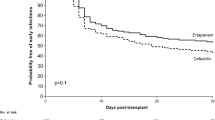
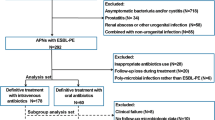
Kidney transplant recipients are at risk for infections due to carbapenem-resistant Enterobacteriaceae (CRE). Polymyxin-resistant CRE (PR-CRE) infections are especially difficult to treat. The aim of this study was to characterize PR-CRE infections among kidney transplant recipients and identify risk factors for treatment failure. This retrospective cohort study involved all kidney transplant recipients with PR-CRE infection between 2013 and 2017 at our center. Minimal inhibitory concentrations for polymyxin B were determined by broth microdilution. Carbapenem-resistant genes (blaKPC, blaNDM, and blaOXA-48), aminoglycoside-resistance genes, and polymyxin-resistant gene mcr-1 were identified by polymerase chain reaction. All but one of the 47PR-CRE infections identified were due to Klebsiella pneumoniae. The most common type of infection (in 54.3%) was urinary tract infection (UTI). Monotherapy was used in 10 cases. Combined treatment regimens included double-carbapenem therapy in 19 cases, oral fosfomycin in 19, and amikacin in 13. Treatment failure occurred in 21 cases (45.7%). Clinical success was achieved 78.9% of patients who used aminoglycosides versus 37.0% of those who not used this drug (p = 0.007). Multivariate analysis showed diabetes mellitus to be a risk factor for treatment failure; amikacin use and UTI were found to be protective. Nine strains were RmtB producers. Although aminoglycosides constitute an important therapeutic option for PR-CRE infection, the emergence of aminoglycoside resistance could have a major impact on the management of CRE infection.



Similar content being viewed by others
References
Aguado JM, Silva JT, Fernández-Ruiz M, Cordero E, Fortún J, Gudiol C, Martínez-Martínez L, Vidal E, Almenar L, Almirante B, Cantón R, Carratalá J, Caston JJ, Cercenado E, Cervera C, Cisneros JM, Crespo-Leiro MG, Cuervas-Mons V, Elizalde-Fernández J, Fariñas MC, Gavaldà J, Goyanes MJ, Gutiérrez-Gutiérrez B, Hernández D, Len O, López-Andujar R, López-Medrano F, Martín-Dávila P, Montejo M, Moreno A, Oliver A, Pascual A, Pérez-Nadales E, Román-Broto A, San-Juan R, Serón D, Solé-Jover A, Valerio M, Muñoz P, Torre-Cisneros J (2018) Management of multidrug resistant gram-negative bacilli infections in solid organ transplant recipients: SET/GESITRA-SEIMC/REIPI recommendations. Transplant Rev 32:36–57
Gutiérrez-Gutiérrez B, Salamanca E, de Cueto M, Hsueh PR, Viale P, Paño-Pardo JR, Venditti M, Tumbarello M, Daikos G, Cantón R, Doi Y, Tuon FF, Karaiskos I, Pérez-Nadales E, Schwaber MJ, Azap ÖK, Souli M, Roilides E, Pournaras S, Akova M, Pérez F, Bermejo J, Oliver A, Almela M, Lowman W, Almirante B, Bonomo RA, Carmeli Y, Paterson DL, Pascual A, Rodríguez-Baño J (2017) Effect of appropriate combination therapy on mortality of patients with bloodstream infections due to carbapenemase-producing Enterobacteriaceae (INCREMENT): a retrospective cohort study. Lancet Infect Dis 3099:1–9
Freire MP, Abdala E, Moura ML, de Paula FJ, Spadão F, Caiaffa-Filho HH, David-Neto E, Nahas WC, Pierrotti LC (2015) Risk factors and outcome of infections with Klebsiella pneumoniae carbapenemase-producing K. pneumoniae in kidney transplant recipients. Infection 43:315–323
Simkins J, Muggia V, Cohen HW, Minamoto GY (2014) Carbapenem-resistant Klebsiella pneumoniae infections in kidney transplant recipients: a case-control study. Transpl Infect Dis 16:775–782
Varotti G, Dodi F, Terulla A, Santori G, Bertocchi M, Marchese A, Fontana I, Unit KT (2017) Impact of carbapenem-resistant Klebsiella pneumoniae (CR-KP) infections in kidney transplantation. Transpl Infect Dis 19:e12757
Nabarro LEB, Veeraraghavan B (2015) Combination therapy for carbapenem-resistant Enterobacteriaceae: increasing evidence, unanswered questions, potential solutions. Eur J Clin Microbiol Infect Dis 34:2307–2311
Jeannot K, Bolard A, Plésiat P (2017) Resistance to polymyxins in gram-negative organisms. Int J Antimicrob Agents
Sampaio JLM, Gales AC (2016) Antimicrobial resistance in Enterobacteriaceae in Brazil: focus on β-lactams and polymyxins. Brazilian J Microbiol 47:31–37
2017. CDC/NHSN surveillance definitions for specific types of infections
EUCAST. 2017. European Committee on Antimicrobial Susceptibility Testing (EUCAST). Breakpoints tables for interpretation of MICs and zone diameters. Version 7.0
CLSI. 2017. Performance standards for antimicrobial susceptibility testing. 27th ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standards Institute
Poirel L, Walsh TR, Cuvillier V, Nordmann P (2011) Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis 70:119–123
Bueno MFC, Francisco GR, O’Hara JA, De Oliveira Garcia D, Doi Y (2013) Coproduction of 16S rRNA methyltransferase RmtD or RmtG with KPC-2 and CTX-M group extended-spectrum βlactamases in Klebsiella pneumoniae. Antimicrob Agents Chemother 57:2397–2400
Doi Y, Arakawa Y (2007) 16S ribosomal RNA methylation: emerging resistance mechanism against aminoglycosides. Clin Infect Dis 45:88–94
Gautom RK. 1997. Rapid pulsed-field gel electrophoresis protocol for typing of Escherichia coli O157: H7 and other gram-negative organisms in 1 day 35:2977–2980
Seroy JT, Grim SA, Reid GE, Wellington T, Clark NM (2016) Treatment of MDR urinary tract infections with oral fosfomycin: a retrospective analysis. J Antimicrob Chemother 71:2563–2568
Mouloudi E, Massa E, Piperidou M, Papadopoulos S, Iosifidis E, Roilides I, Theodoridou T, Kydona C, Fouzas I, Imvrios G, Papanikolaou V, Gritsi-Gerogianni N (2014) Tigecycline for treatment of carbapenem-resistant Klebsiella pneumoniae infections after liver transplantation in the intensive care unit: a 3-year study. Transplant Proc 46:3219–3221
Freire MP, Oshiro ICVS, Pierrotti LC, Bonazzi PR, De Oliveira LM, Song ATW, Camargo CH, Van Der Heijden IM, Rossi F, Costa SF, D’Albuquerque LAC, Abdala E (2017) Carbapenem-resistant Enterobacteriaceae acquired before liver transplantation: impact on recipient outcomes. Transplantation 101
Giannella M, Bartoletti M, Morelli MC, Tedeschi S, Cristini F, Tumietto F, Pasqualini E, Danese I, Campoli C, Di Lauria N, Faenza S, Ercolani G, Lewis R, Pinna AD, Viale P (2015) Risk factors for infection with carbapenem-resistant Klebsiella pneumoniae after liver transplantation: the importance of pre- and posttransplant colonization. Am J Transplant 15:1708–1715
Tumbarello M, Trecarichi EM, De Rosa FG, Giannella M, Giacobbe DR, Bassetti M, Losito AR, Bartoletti M, Del Bono V, Corcione S, Maiuro G, Tedeschi S, Celani L, Cardellino CS, Spanu T, Marchese A, Ambretti S, Cauda R, Viscoli C, Viale P (2015) Infections caused by KPC-producing Klebsiella pneumoniae: differences in therapy and mortality in a multicentre study. J Antimicrob Chemother 70:2133–2143
Sastry S, Clarke LG, Alrowais H, Querry AM, Shutt KA, Doi Y (2015) Clinical appraisal of fosfomycin in the era of antimicrobial resistance. Antimicrob Agents Chemother 59:7355–7361
Endimiani A, Patel G, Hujer KM, Swaminathan M, Perez F, Rice LB, Jacobs MR, Bonomo RA (2010) In vitro activity of Fosfomycin against blaKPC-containing Klebsiella pneumoniae isolates, including those nonsusceptible to tigecycline and/or colistin. Antimicrob Agents Chemother 54:526–529
Rosa R, Rudin SD, Rojas LJ, Hujer AM, Perez-Cardona A, Perez F, Bonomo RA, Martinez O, Abbo LM, Camargo JF (2018) “Double carbapenem” and oral fosfomycin for the treatment of complicated urinary tract infections caused by bla NDM -harboring Enterobacteriaceae in kidney transplantation. Transpl Infect Dis 20:e12795
Tängdén T, Hickman RA, Forsberg P, Lagerbäck P, Giske CG, Cars O (2014) Evaluation of double- and triple-antibiotic combinations for VIM- and NDM-producing Klebsiella pneumoniae by in vitro time-kill experiments. Antimicrob Agents Chemother 58:1757–1762
Loethen AA, Kerstenetzky L, Descourouez JL, Leverson GE, Smith JA, Jorgenson MR (2017) Fosfomycin for the treatment of cystitis in the abdominal solid organ transplant population. Pharmacotherapy 37:599–606
Souli M, Karaiskos I, Masgala A, Galani L, Barmpouti E, Giamarellou H (2017) Double-carbapenem combination as salvage therapy for untreatable infections by KPC-2-producing Klebsiella pneumoniae. Eur J Clin Microbiol Infect Dis 36:1305–1315
Neuner EA, Gallagher JC (2016) Pharmacodynamic and pharmacokinetic considerations in the treatment of critically ill patients infected with carbapenem-resistant Enterobacteriaceae. Virulence 0:1–13
Camargo JF, Simkins J, Beduschi T, Tekin A, Aragon L, Pérez-Cardona A, Prado CE, Morris MI, Abbo LM, Cantón R (2015) Successful treatment of carbapenemase-producing pandrug-resistant Klebsiella pneumoniae bacteremia. Antimicrob Agents Chemother 59:5903–5908
Oliva A, Mascellino MT, Cipolla A, Abramo AD, De Rosa A, Savinelli S, Rosa M, Mastroianni CM (2015) Therapeutic strategy for pandrug-resistant Klebsiella pneumoniae severe infections: short-course treatment with colistin increases the in vivo and in vitro activity of double carbapenem regimen. Int J Infect Dis 33:132–134
De Pascale G, Martucci G, Montini L, Panarello G, Cutuli SL, Di Carlo D, Di Gravio V, Di Stefano R, Capitanio G, Vallecoccia MS, Polidori P, Spanu T, Arcadipane A, Antonelli M (2017) Double carbapenem as a rescue strategy for the treatment of severe carbapenemase-producing Klebsiella pneumoniae infections: a two-center, matched case-control study. Crit Care 21:1–10
Venugopalan V, Nogid B, Le TN, Rahman SM, Bias TE (2017) Double carbapenem therapy (DCT) for bacteremia due to carbapenem-resistant Klebsiella pneumoniae (CRKP): from test tube to clinical practice. Infect Dis (Auckl) 49:867–870
Cprek JB, Gallagher JC (2015) Ertapenem-containing double-carbapenem therapy for treatment of infections caused by carbapenem-resistant Klebsiella pneumoniae. Antimicrob Agents Chemother 60:669–673
Van Duin D, Lok JJ, Earley M, Cober E, Richter SS, Perez F, Salata RA, Kalayjian RC, Watkins RR, Doi Y, Kaye KS, Jr VGF, Paterson DL, Bonomo RA, Evans S (2017) Colistin versus ceftazidime-avibactam in the treatment of infections due to carbapenem-resistant Enterobacteriaceae. Clin Infect Dis 66:163–171
Shields RK, Nguyen MH, Chen L, Press EG, Potoski BA, Marini RV, Doi Y, Kreiswirth BN, Clancy CJ (2017) Ceftazidime-avibactam is superior to other treatment regimens against carbapenem-resistant Klebsiella pneumoniae bacteremia. Antimicrob Agents Chemother 61:1–7
Shields RK, Clancy CJ, Press EG, Hong M. 2016. Aminoglycosides for treatment of bacteremia due to carbapenem-resistant Klebsiella pneumoniae 60:3187–3192
Abboud CS, Bergamasco MD, De Sousa EE, De Cássia Zandonadi E, Cortez D (2013) Successful use of gentamycin as an antibiotic prophylaxis regimen to reduce the rate of healthcare-associated infections after renal transplantation. Brazilian J Infect Dis 17:254–255
Gonzalez-Padilla M, Torre-Cisneros J, Rivera-Espinar F, Pontes-Moreno A, López-Cerero L, Pascual A, Natera C, Rodríguez M, Salcedo I, Rodríguez-López F, Rivero A, Rodríguez-Baño J (2015) Gentamicin therapy for sepsis due to carbapenem-resistant and colistin-resistant Klebsiella pneumoniae. J Antimicrob Chemother 70:905–913
Doi Y, Wachino J, Arakawa Y (2016) Aminoglycoside resistance. Infect Dis Clin N Am 30:523–537
Galani I, Souli M, Panagea T, Poulakou G, Kanellakopoulou K, Giamarellou H (2012) Prevalence of 16S rRNA methylase genes in Enterobacteriaceae isolates from a Greek university hospital. Clin Microbiol Infect 18:E52–E54
Zhou Y, Yu H, Guo Q, Xu X, Ye X, Wu S, Guo Y, Wang M (2010) Distribution of 16S rRNA methylases among different species of gram-negative bacilli with high-level resistance to aminoglycosides. Eur J Clin Microbiol Infect Dis 29:1349–1353
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by our Institutional Review Board and due to its retrospective study design, patient informed consent was waived.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Freire, M.P., de Oliveira Garcia, D., Cury, A.P. et al. The role of therapy with aminoglycoside in the outcomes of kidney transplant recipients infected with polymyxin- and carbapenem-resistant Enterobacteriaceae. Eur J Clin Microbiol Infect Dis 38, 755–765 (2019). https://doi.org/10.1007/s10096-019-03468-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-019-03468-4