Abstract
Staphylococcus aureus is an infrequent cause of community-associated (CA-SA) pneumonia in children. The aim of this study was to evaluate the clinical, epidemiological, microbiological, and molecular characteristics of CA-SA pneumonia among children hospitalized in two large tertiary care referral centers during an 8-year period. Cases of CA-SA pneumonia admitted between 2007 and 2014 were retrospectively examined through medical record review. Molecular investigation was performed for available strains; mecA, Panton–Valentine leukocidin (PVL) (lukS-lukF-PV), and fibronectin binding protein A (fnbA) genes were detected by polymerase chain reaction (PCR). Clones were assigned by agr groups, pulsed-field gel electrophoresis (PFGE), SCCmec, and multilocus sequencing typing (MLST). In total, 41 cases were recorded (boys, 61 %), with a median age of 4.3 months (range, 1–175). Methicillin-resistant S. aureus (MRSA) accounted for 31 cases (75.6 %). Complications included empyema (25/41, 61 %), pneumatoceles (7/41, 17 %), and lung abscess (1/41, 2.5 %). Intensive care unit (ICU) admission was required in 58.5 %. Two deaths occurred (4.9 %). Definitive therapy was based on vancomycin with or without other antibiotics (55.9 %), followed by clindamycin and linezolid (26.5 % each). All isolates were susceptible to vancomycin (MIC90 2 mg/L, range 1–2), teicoplanin, and linezolid, whereas 26.8 % were resistant to clindamycin. Among the 25 studied strains, 20 were mecA-positive (MRSA), carrying also the fnbA gene. Of these, 90 % belonged to the ST80-IV/agr3/PVL-positive clone. Methicillin-susceptible S. aureus (MSSA) strains showed polyclonality, 3/5 were PVL-positive, and 3/5 were fnbA-positive. MRSA and particularly the ST80-IV clone predominated among staphylococcal pneumonia cases in children. Treatment provided was effective in all but two patients, despite the relatively high minimum inhibitory concentration (MIC) of vancomycin and a high resistance to clindamycin.
Similar content being viewed by others
Introduction
Staphylococcus aureus is a major pathogen responsible for a wide spectrum of infections, pneumonia being one of the most serious and life-threatening. It is estimated to cause 1–10 % of community-associated pneumonia (CAP) and 20–50 % of nosocomial pneumonia [1]. Community-associated methicillin-resistant S. aureus (CA-MRSA) has become a well-established pathogen during the last two decades, in both outpatient and healthcare settings. Community-associated S. aureus (CA-SA) pneumonia remains a fairly rare but serious condition both in children and adults. Panton–Valentine leukocidin (PVL) is a well-known virulence factor, implicated in staphylococcal pneumonia [2, 3]. The initial adherence of S. aureus to the respiratory epithelium is mediated through a group of surface adhesins called MSCRAMMS (microbial surface components recognizing adhesive matrix molecules). Among them, fibronectin binding protein A (FnBP) encoded by the fnbA gene plays an important role [4, 5]. In the USA, there has been an increase in staphylococcal pneumonia cases over the past decade among previously healthy children, particularly presenting as necrotizing pneumonia with empyema [6, 7]. The MRSA ST8-USA300 clone is predominant among these cases. Meanwhile, MRSA strains in Europe have evolved far more heterogeneously and genetically diverse, with the so-called European ST80 clone being predominant [8, 9]. Little is known about the current epidemiology of pediatric staphylococcal pneumonia in Europe, especially in Greece, with a burden of MRSA-associated invasive disease estimated at 40 % of all cases attributed to S. aureus [10].
We retrospectively investigated the clinical and microbiologic characteristics of CA-SA pneumonia among children hospitalized in the two large tertiary care referral centers in Athens over an 8-year period.
Materials and methods
Study design and population
The “P. & A. Aglaia Kyriakou” Children’s Hospital (Institution 1) and the “Aghia Sophia” Children’s Hospital (Institution 2) in Athens are two tertiary care referral centers accommodating 400 and 700 beds, respectively. Institution 1 receives 25,000–27,000 admissions, whereas Institution 2 receives 51,000–53,000 admission per year. They both serve the population of the greater Athens area comprising about 4.25 million people (2014 census), as well as other parts of central Greece. Children hospitalized with the diagnosis of primary CA-SA pneumonia in both hospitals from January 1st, 2007 to December 31st, 2014 were included in this retrospective study. Cases were identified from the microbiology laboratory database in each hospital. The demographic, clinical, and radiologic characteristics, as well as laboratory and microbiological findings, were recorded after review of medical records. Moreover, empiric and definitive treatment, complications, surgical interventions, and outcome were also recorded for each case.
Definitions
Staphylococcus aureus pneumonia was defined by isolation of the organism from pleural fluid, blood, or lung tissue from children with clinical and radiologic findings of pneumonia, with or without parapneumonic effusion. Cases with clinical signs and radiographic findings of pneumonia in which Gram stain of bronchial aspirates showed Gram-positive cocci and the organism was grown in pure culture were also included. A community-associated infection was defined according to the Centers for Disease Control and Prevention (CDC) criteria [11]. Pleural empyema was defined as pleural effusion with macroscopic presence of pus or a positive Gram stain, or culture demonstrating the presence of bacteria in the pleural space [12]. Lung abscess was considered when there was a cavitary lung lesion containing an air–fluid level on radiograph or computed tomography (CT) [13]. Viral co-infection was the detection of a viral pathogen from respiratory secretions (nasal swab/wash or tracheal aspirate).
Microbiological methods
Bacterial cultures were performed according to standard microbiological methods. Blood and pleural fluid cultures were carried out using BD BACTEC Peds Plus/F® vials in the BACTEC system (Becton, Dickinson and Company, Sparks, MD, USA). Staphylococcus aureus was identified by Gram stain, catalase, and coagulase production (Pastorex™ Staph-Plus, Bio-Rad, Marnes-la-Coquette, France) and the VITEK 2 Advanced Expert System (bioMérieux, Marcy l’Etoile, France). Antimicrobial susceptibility testing to cefoxitin, gentamicin, rifampicin, kanamycin, erythromycin, clindamycin, tetracycline, ciprofloxacin, and sulfamethoxazole–trimethoprim was performed by the disk diffusion method according to the Clinical and Laboratory Standards Institute (CLSI) guidelines, whereas for fusidic acid, the European Committee for Antimicrobial Susceptibility Testing (EUCAST) breakpoints were used. The minimum inhibitory concentrations (MICs) of vancomycin, teicoplanin, and linezolid were determined with a gradient method (Etest, bioMérieux, Marcy l’Etoile, France). MRSA were defined as those cases with cefoxitin-resistant isolates by the disk diffusion method.
Investigation for viral pathogens from nasal swabs/washes or tracheal aspirates was carried out upon admission in 12 patients in whom epidemiological and clinical data indicated a possible viral infection. Samples were examined by reverse transcription polymerase chain reaction (RT-PCR) for influenza A and B and cytomegalovirus (CMV) viruses (Cobas AmpliPrep/Cobas TaqMan CMV Test, Roche Diagnostics, Penzberg, Germany) and by direct immunofluorescence for respiratory syncytial virus (RSV), parainfluenza virus types (PIV) 1, 2 and 3 (PathoDx™ Respiratory Virus Panel, Remel Europe Ltd., Dartford, UK).
Molecular methods
Molecular investigation was performed for 25 available S. aureus strains, as follows.
Toxin genes and adhesion factors detection
Genes encoding PVL (lukS-lukF-PV) and fnbA were investigated by PCR [14]. PCR products were analyzed by electrophoresis onto agarose 1 % w/v gels. Staphylococcus aureus strains ATCC49775 (PVL-positive, agr3), Fri 913 (agr1), Fri 137 (agr2), and HT 20000195 (agr4) were used as positive controls for the PCR assays [14].
Molecular typing
DNA extraction was performed into agarose disks, whereas pulsed-field gel electrophoresis (PFGE) of SmaI DNA digests in a CHEF-DR III apparatus (Bio-Rad Laboratories, Richmond, CA, USA) was as previously described [15]. Visual interpretation of the PFGE banding patterns and the assignments of types (pulsotypes) were performed according to the criteria of Tenover et al. PFGE types were named using capital letters. agr groups and SCCmec types were defined by PCR [14, 16]. Multilocus sequencing typing (MLST) was performed for 20 selected representative isolates according to agr groups, PFGE types, SCCmec types, gene profiles, and antibiotic resistance patterns (http://www.mlst.net). Clones were defined according to ST-SCCmec types.
Measurement of serum vancomycin levels
Trough levels of vancomycin in patients’ serum were measured with fluorescence polarization immunoassay (Abbott AxSYM, Abbott Laboratories, Irving, TX, USA).
Statistics
Counts and percentages were reported for categorical variables, and median and interquartile range (IQR: 25th−75th percentile) for continuous variables with non-symmetric distribution, unless otherwise noted. Statistical significance of observed associations was evaluated using the χ2 or Fisher’s exact test for categorical variables and Mann–Whitney U-test or Kruskal–Wallis test for continuous variables, as appropriate. Time trends were examined using the Mann–Kendall test. All tests were two-tailed and α = 0.05 was considered as the level of significance. Statistical analysis was performed using SPSS for Windows, version 18 (SPSS, Chicago, IL, USA).
Results
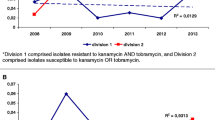
In total, 132 cases of documented bacterial CAP were recorded during the study period after review of the microbiology laboratory records. Among them, 90 (68.94 %) were due to Streptococcus pneumoniae and 41 (31.06 %) to S. aureus; MRSA accounted for 31 of the latter (75.6 %). There was an increasing trend in the number of admitted CA-SA cases per year, but the difference was not statistically significant (p = 0.09).
Demographics
The demographic characteristics of the patients are shown in Table 1. The median age of the cohort was 4.3 months (range, 1–175 months). Four children (9.75 %) had an underlying condition and for two of them, both younger than 2 months of age, methicillin-susceptible S. aureus (MSSA) pneumonia was the first manifestation of cystic fibrosis and severe combined immunodeficiency (SCID), respectively. A 19-month-old child had congenital heart disease, whereas another patient with MRSA infection had a history of central nervous system (CNS) glioma while being off chemotherapy. There was no difference in the demographic characteristics among patients infected with MRSA or MSSA strains; however, those with underlying illness were more commonly affected by MSSA (p = 0.012). No other difference was noted between MRSA and MSSA cases with regard to their demographic characteristics.
Radiologic, laboratory, and clinical characteristics
The radiologic and laboratory findings of patients admitted with staphylococcal pneumonia are shown in Table 2. A chest X-ray was obtained in all patients and a chest ultrasound in 24/41 (58.5 %) of cases. In six (14.6 %) children, a chest CT scan was performed. No significant difference was evident with regard to radiologic findings in relation to methicillin resistance, although all seven cases with pneumatoceles were caused by MRSA. Similarly, there was no significant difference between the two groups when white blood cell (WBC) counts were compared. However, it is remarkable that, from all six patients with leukopenia, MRSA was recovered. Patients with MRSA infection had significantly higher C-reactive protein (CRP) levels (222 vs. 110 mg/L, normal values <5 mg/L, p = 0.012).
Two patients (4 months and 10 years of age, respectively) with MRSA infection had pulmonary involvement during hospitalization for osteomyelitis. The first had osteomyelitis of the tibia and developed bacteremia, deep venous thrombosis (DVT), and pulmonary septic emboli with bilateral pleural fluid, while the second had acute femoral osteomyelitis and bilateral consolidation. Viral co-infections were identified in five (H1N1, PIV1, PIV3, CMV, and RSV) out of 12 tested children; however, investigation for viral infection was not systematically performed in all patients.
Microbiological and molecular analyses
Staphylococcus aureus was isolated from pleural fluid in 29 cases (70.7 %), blood in eight (19.5 %), bronchial aspirate in two (4.9 %), and from both pleural fluid and blood in another two patients (4.9 %). The percentage of concurrent bacteremia was similar between the MRSA and MSSA groups (25.8 vs. 30 %) (p = 0.68).
Among all isolates, MRSA (cefoxitin-resistant) accounted for 31 cases (75.6 %). All MRSA strains were resistant to fusidic acid, tetracycline, and kanamycin. None was resistant to gentamicin, rifampicin, sulfamethoxazole–trimethoprim, and ciprofloxacin. Regarding MSSA isolates, 90 % were resistant to penicillin and 20 % to sulfamethoxazole–trimethoprim. Overall, 13 (31.7 %) strains were resistant to erythromycin, 40 % among MSSA and 29 % in MRSA (p = 0.51). Interestingly, the overall rate of resistance to clindamycin was high (11/41, 26.8 %), higher among MRSA (9/31, 29 %) as compared to MSSA (2/10, 20 %, p = 0.57). Among them, 9/11(81.8 %) showed inducible resistance to clindamycin. The ΜIC50 of vancomycin was 1.5 mg/L, teicoplanin 1 mg/L, and linezolid 0.75 mg/L. The MIC90 of vancomycin was 2 mg/L (range, 1–2 mg/L), teicoplanin 1.5 mg/L (range, 0.5–2), and linezolid 1 mg/L (range, 0.25–2 mg/L). All strains were susceptible to linezolid.
Twenty-five strains were available for molecular analysis (five MSSA and 20 MRSA). All MRSA strains were mecA-positive, none carried mecC. Eighteen MRSA strains were PVL-positive and belonged to the ST80-IV/agr3 clone. Moreover, one PVL-positive strain belonged to ST80-IV/agr1 and one PVL-negative strain belonged to ST30-IV/agr1 clones. All were positive for fnbA. MSSA strains showed polyclonality. Three out of five MSSA were PVL-positive and another three positive for fnbA (Table 3).
Staphylococcus aureus nasal colonization was investigated in 30 (73.2 %) children and, among them, 18 (60 %) were found positive; in each patient, the colonizing strain had a phenotypically identical antimicrobial susceptibility pattern with the strain causing pneumonia.
Management and outcome
Data regarding antimicrobial treatment and type of management are shown in Table 4.
Empirical therapy consisted of beta-lactam with or without other antibiotics for 31 among 37 recorded cases (83.8 %), whereas clindamycin was used alone or as part of therapy in 15 (40.5 %) cases. Vancomycin was given as part of therapy in 17 (45.9 %) cases.
Definitive therapy solely with vancomycin was administered to eight (21.6 %) patients, all with MRSA pneumonia, for 15–25 days. The vancomycin MIC was 2 mg/L for four of these cases; nevertheless, the final outcome was favorable. Clindamycin alone or in combination with other antibiotics was used in ten children (27 %) and linezolid in 12 (32.4 %), among which ten with MRSA pneumonia. For MSSA cases, antistaphylococcal penicillin was used as standard of care in seven children and linezolid was used for two children who were admitted in the pediatric intensive care unit (PICU). Trough levels for vancomycin were measured only in four (25 %) of the vancomycin-treated cases and they were below 15 μg/L in two and between 15–20 μg/L in the other two cases.
Two deaths occurred, both due to MRSA. A 5-month-old boy with a preceding influenza-like illness who was positive for PIV1 developed necrotizing pneumonia and acute respiratory distress syndrome requiring mechanical ventilation and died on the third hospitalization day in the ICU. The second patient was a 14-year-old girl with post-H1N1 staphylococcal pneumonia. Both had leukopenia on admission (WBC counts of 900/μL and 1000/μL, respectively). Patients with MSSA infection had a significantly longer duration of hospitalization (26.5 vs. 21 days, p = 0.04). However, this difference did not reach significance when the two patients who deceased soon after their admission (on the first and third days of hospitalization, respectively) were excluded from the analysis (26.5 vs. 22 days, p = 0.06).
There was no statistically significant difference on disease severity, procedural intervention, and the outcome of pneumonia between patients with PVL-negative and PVL-positive strains, whereas children with underlying disease were prone to having pneumonia caused by a PVL-negative strain (p = 0.012).
Discussion
In pediatric CAP, S. pneumoniae and S. aureus were the most commonly isolated bacterial pathogens for our population; this is in accordance with a similar study from India where S. aureus was found to be an important pathogen [17]. Our study focused on the investigation of factors predisposing to S. aureus pneumonia in children and correlated them to virulence factors of the bacterium. We retrospectively reviewed a considerable cohort of community-associated S. aureus pneumonia cases hospitalized in the two largest pediatric hospitals in Greece, a country with a heavy burden of MRSA-associated disease [10].
To the best of our knowledge, this is a unique series of pediatric pneumonia cases in Europe. Although there are a few reports concerning pediatric community-acquired S. aureus pneumonia from the USA, relevant data from Europe are scarce and only a few case reports have been published [18–20].
Most of our patients were boys and young infants, with a median age of 4.3 months, in accordance with the first documentation from Chartrand and McCracken in 1982, who reported a median age of 6 months among patients with staphylococcal pneumonia [21]. Thus, S. aureus pneumonia remains predominantly a disease of young infants. No significant difference according to age and race was found regarding the status of methicillin resistance. Similar results were observed regarding distinct radiologic entities and complications, including multilobular infiltrates, pneumatoceles, empyema, abscess, and evolution to necrotizing pneumonia.
Α predominance of MRSA was noted as the cause of staphylococcal pneumonia in our cohort, in which most children had no underlying illness. This is in accordance with recent data from the USA [6], where the prevalence of MRSA was 74 % among 117 staphylococcal pneumonia cases. According to recent data from Institution 1, the rate of MRSA strains involved in pneumonia was higher as compared to other types of invasive staphylococcal disease (72 vs. 44.4 %).
Staphylococcus aureus can invade the lung parenchyma directly through the tracheobronchial tree or through the hematogenous route. In this report, there were two cases of pulmonary involvement concurrently with osteoarticular infection, both due to MRSA. No evidence of endocarditis was found in these patients. Pulmonary involvement in children with staphylococcal osteomyelitis is not uncommon, especially in MRSA-associated disease [7].
From previously published data covering a 15-year period, it is evident that the European ST80-mecA-PVL-positive clone is predominant in Greece and accounts for the vast majority of MRSA infections [9, 22]. PVL leukocidin forms pores in the cell membrane, causing lysis of the host’s neutrophils, monocytes, and macrophages, inducing a significant release of inflammation mediators. This clone is characterized by resistance to fusidic acid, kanamycin, and tetracycline [9, 23], and was predominant in the present cohort of pediatric pneumonia cases among MRSA strains. It is generally accepted that PVL-positive S. aureus strains exhibit a tropism for the lower respiratory tract [3]. However, it seems that PVL is a virulence factor for severe staphylococcal pneumonia, regardless of methicillin resistance. We did not observe any significant difference in the duration of hospital stay, rate of admission to the PICU, and requirement for surgical intervention in association with methicillin resistance. Remarkably, all MRSA isolates except for one and 3/5 MSSA strains causing pneumonia in the present study were PVL-positive. Thomas et al. reported a case series where community-acquired PVL-producing MSSA strains caused pneumonia with complications, such as pneumatoceles, recurrent bilateral multilobar infiltrates, pneumothoraces, empyema, lung abscess, and diaphragmatic paralysis [24]. Diep et al., in 2010, found a striking epidemiological association of PVL with serious staphylococcal infections, using a rabbit model of necrotizing pneumonia [25].
All but two of the examined staphylococcal strains in this study were positive for the fnbA gene encoding fibronectin binding proteins (FnBPs). Microbial adherence to cells and matrix components promotes colonization and infection. Mongodin et al. have shown that S. aureus prefers mainly undifferentiated human airway epithelial cells (HAECs) for adhesion through FnBPs, whereas protein A (SpA) and clumping factor (ClfA) do not play a role in this process. Fibronectin acts as a bridging molecule between cellular a5b1-integrins and staphylococcal FnBPs, inducing, thus, the adherence of the microbe to epithelial cells, fibroblasts, and subsequent internalization of the pathogen [4]. In the same study, among 32 S. aureus strains from cystic fibrosis lungs and nosocomial pneumonia, 97 % possessed the fnbA and fnbB genes.
Necrotizing pneumonia is an uncommon complication of CAP in children. Although it can also be caused by S. pneumoniae, it is most commonly associated with PVL-positive staphylococcal infection. In a recent study from France, a bacterial agent was identified in 21/41 patients of necrotizing pneumonia and S. aureus accounted for 13/21 cases. Twelve of these 13 cases were caused by MSSA PVL-positive strains and one by MRSA [20].
The mortality rate in the present study was low (4.9 %) as compared to 39 %, a rate reported in a series of 133 community-associated PVL-positive staphylococcal pneumonia cases from France between 1986 and 2010, which included children and adults with a median age of 22 years. In the same study, mortality was not related to methicillin resistance but to the presence of erythroderma, airway bleeding, and leukopenia [26]. In a recent study from Texas, USA that included 119 children with staphylococcal pneumonia, the mortality was 0.85 % [6]. In a series of 14 PICU-admitted children with MRSA pneumonia or pulmonary involvement from Tunisia over a 9-year period, the observed mortality was 14.3 % [27]. Lethal cases of necrotizing MRSA pneumonia have been linked to antecedent viral respiratory infection, with influenza being the prototype infection [28, 29]. Influenza infection was documented in one of the two lethal cases in our series.
Of note, it has been recently suggested that low leukocyte count is a marker of poor prognosis, allowing early identification of severe cases and appropriate management. In a French case series of 148 cases of childhood and adulthood necrotizing pneumonia due to PVL-positive S. aureus, the mortality rate was 75.8 % for the 62 cases with leukocyte count below 3000/μL [30]. The same is suggested by our findings as mortality was high among patients with leukopenia (2/6, 33.3 %), and both patients who died had leukopenia.
The majority of our cases required an invasive procedure to drain the pleural exudate or, in addition, decortication to excise the fibrinous pleural peel for the resolution of complicated pneumonia. Conservative management only with antibiotics is not adequate and prolongs hospitalization [31].
Our study shows a high resistance rate of pneumonia-causing strains to clindamycin (26.8 %) in comparison with the average resistance rate (15.6 %) of all MRSA clinical isolates (n = 1083) in institution 1 for the period 2007–2013 (unpublished data). Although clindamycin is recommended as an option for empiric therapy among children with possible staphylococcal pneumonia, the disproportionately high resistance rate observed indicates that this antibiotic should not be used empirically as monotherapy in these settings.
There is growing evidence that antimicrobial agents which inhibit the microbial ribosome system, such as the protein synthesis inhibitors clindamycin and linezolid, suppress the synthesis of bacterial toxins. In addition to alpha-hemolysin (Hla) and protein A (SpA), which are well-known mediators of staphylococcal disease, PVL is a toxin almost ubiquitously present in CA-MRSA strains causing pneumonia, bone, and skin and soft tissue disease. Otto et al. have recently shown that clindamycin suppresses PVL, Hla, and SpA mRNA levels, and subinhibitory concentrations of clindamycin decreased the levels of the three mRNAs studied [32]. Linezolid reduced the mRNA and protein expression of PVL and SpA, though to a lesser extent than clindamycin. Exposure to subinhibitory concentrations of vancomycin had no significant effect on PVL, Hla, and spA mRNAs. It is, therefore, suggested that clindamycin and linezolid can suppress staphylococcal virulence factors in serious infections. However, there are no clinical studies to document an improved outcome over vancomycin with the inclusion of these antibiotics in the therapeutic regimen against MRSA CAP. Furthermore, linezolid has not been endorsed as a first-line treatment and is considered as an alternative agent by the Infectious Diseases Society of America (IDSA) guidelines for the treatment of MRSA-associated CAP in infants and children older than 3 months of age [33]. The choice of linezolid over vancomycin in MRSA CAP is still inconclusive, since data from clinical trials comparing different antibiotics for this form of pneumonia are not available [34].
A limitation of our study is that it was conducted retrospectively, compromising the uniform access to all medical information. Moreover, testing for respiratory viruses was not routinely sought for every single case and the point outcome was “discharged alive” and long-term follow-up was not available.
In conclusion, the European ST80-IV-PVL-positive MRSA clone predominates among community-associated S. aureus pneumonia cases in our settings, although the overall staphylococcal pneumonia prevalence is not high. Clinicians should be aware that PVL-positive staphylococcal pneumonia can be lethal, even among previously healthy children. Optimal treatment includes prompt pleural drainage, together with proper antibiotic therapy. Treatment provided was effective in all but two patients, despite the relatively high MIC of vancomycin (≥1 mg/L) in all cases. The knowledge of high local resistance rate to clindamycin warrants broad coverage when treatment is empirically initiated. Appropriate modification can be applied as definitive treatment, after the antimicrobial susceptibility testing is available to the clinician.
References
Howard LS, Sillis M, Pasteur MC, Kamath AV, Harrison BD (2005) Microbiological profile of community-acquired pneumonia in adults over the last 20 years. J Infect 50(2):107–113
Lina G, Piémont Y, Godail-Gamot F, Bes M, Peter MO, Gauduchon V, Vandenesch F, Etienne J (1999) Involvement of Panton–Valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin Infect Dis 29(5):1128–1132
Gillet Y, Issartel B, Vanhems P, Fournet JC, Lina G, Bes M, Vandenesch F, Piémont Y, Brousse N, Floret D, Etienne J (2002) Association between Staphylococcus aureus strains carrying gene for Panton–Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet 359(9308):753–759
Mongodin E, Bajolet O, Cutrona J, Bonnet N, Dupuit F, Puchelle E, de Bentzmann S (2002) Fibronectin-binding proteins of Staphylococcus aureus are involved in adherence to human airway epithelium. Infect Immun 70(2):620–630
Foster TJ, Höök M (1998) Surface protein adhesins of Staphylococcus aureus. Trends Microbiol 6:484–488
Carrillo-Marquez MA, Hulten KG, Hammerman W, Lamberth L, Mason EO, Kaplan SL (2011) Staphylococcus aureus pneumonia in children in the era of community-acquired methicillin-resistance at Texas children’s hospital. Pediatr Infect Dis J 30(7):545–550. doi:10.1097/INF.0b013e31821618be
Gonzalez BE, Hulten KG, Dishop MK, Lamberth LB, Hammerman WA, Mason EO Jr, Kaplan SL (2005) Pulmonary manifestations in children with invasive community-acquired Staphylococcus aureus infection. Clin Infect Dis 41(5):583–590
Otter JA, French GL (2010) Molecular epidemiology of community-associated meticillin-resistant Staphylococcus aureus in Europe. Lancet Infect Dis 10:227–239
Drougka E, Foka A, Liakopoulos A, Doudoulakakis A, Jelastopulu E, Chini V, Spiliopoulou A, Levidiotou S, Panagea T, Vogiatzi A, Lebessi E, Petinaki E, Spiliopoulou I (2014) A 12-year survey of methicillin-resistant Staphylococcus aureus infections in Greece: ST80-IV epidemic? Clin Microbiol Infect 20(11):O796–O803. doi:10.1111/1469-0691.12624
European Centre for Disease Prevention and Control (ECDC) (2013) Antimicrobial resistance surveillance in Europe 2012. Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net). ECDC, Stockholm
Morrison MA, Hageman JC, Klevens RMJ (2006) Case definition for community-associated methicillin-resistant Staphylococcus aureus. Hosp Infect 62(2):241
Light RW (1994) Chapter 228: Disorders of the pleura, mediastinum and diaphragm. In: Isselbacher KJ, Braunwald W, Wilson JD, Martin JB, Fauci AS, Kasper DL (eds) Harrison’s principles of internal medicine, 13th edn, McGraw-Hill, New York, pp 1231–1232
Lakser O (2004) Chapter 392: Pulmonary abscess. In: Behrman RE, Kliegman RM, Jenson HB (eds) Nelson textbook of pediatrics, 17th edn. Saunders, Philadelphia, p 1437
Jarraud S, Mougel C, Thioulouse J, Lina G, Meugnier H, Forey F, Nesme X, Etienne J, Vandenesch F (2002) Relationships between Staphylococcus aureus genetic background, virulence factors, agr groups (alleles), and human disease. Infect Immun 70(2):631–641
Tenover FC, Arbeit RD, Goering RV, Mickelsen PA, Murray BE, Persing DH, Swaminathan B (1995) Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol 33(9):2233–2239
Oliveira DC, de Lencastre H (2002) Multiplex PCR strategy for rapid identification of structural types and variants of the mec element in methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 46:2155–2161
Mathew JL, Singhi S, Ray P, Hagel E, Saghafian-Hedengren S, Bansal A, Ygberg S, Sodhi KS, Kumar BV, Nilsson A (2015) Etiology of community acquired pneumonia among children in India: prospective, cohort study. J Glob Health 5(2):050418. doi:10.7189/jogh.05.020418
Haider S, Wright D (2013) Panton–Valentine leukocidin Staphylococcus causing fatal necrotising pneumonia in a young boy. BMJ Case Rep 2013. pii: bcr2012007655. doi:10.1136/bcr-2012-007655
Trieu TV, Gaudelus J, Lefevre S, Teychene AM, Poilane I, Colignon A, Etienne J, de Pontual L (2009) Sudden death caused by Staphylococcus aureus carrying Panton–Valentine leukocidin gene in a young girl. BMJ Case Rep 2009. pii: bcr02.2009.1542. doi:10.1136/bcr.02.2009.1542
Lemaître C, Angoulvant F, Gabor F, Makhoul J, Bonacorsi S, Naudin J, Alison M, Faye A, Bingen E, Lorrot M (2013) Necrotizing pneumonia in children: report of 41 cases between 2006 and 2011 in a French tertiary care center. Pediatr Infect Dis J 32(10):1146–1149. doi:10.1097/INF.0b013e31829be1bb
Chartrand SA, McCracken GH Jr (1982) Staphylococcal pneumonia in infants and children. Pediatr Infect Dis 1:19–23
Niniou I, Vourli S, Lebessi E, Foustoukou M, Vatopoulos A, Pasparakis DG, Kafetzis DA, Tsolia MN (2008) Clinical and molecular epidemiology of community-acquired, methicillin-resistant Staphylococcus aureus infections in children in central Greece. Eur J Clin Microbiol Infect Dis 27(9):831–837. doi:10.1007/s10096-008-0513-7
Chini V, Petinaki E, Foka A, Paratiras S, Dimitracopoulos G, Spiliopoulou I (2006) Spread of Staphylococcus aureus clinical isolates carrying Panton–Valentine leukocidin genes during a 3-year period in Greece. Clin Microbiol Infect 12(1):29–34
Thomas B, Pugalenthi A, Chilvers M (2009) Pleuropulmonary complications of PVL-positive Staphylococcus aureus infection in children. Acta Paediatr 98:1372–1375
Diep BA, Chan L, Tattevin P, Kajikawa O, Martin TR, Basuino L, Mai TT, Marbach H, Braughton KR, Whitney AR, Gardner DJ, Fan X, Tseng CW, Liu GY, Badiou C, Etienne J, Lina G, Matthay MA, DeLeo FR, Chambers HF (2010) Polymorphonuclear leukocytes mediate Staphylococcus aureus Panton–Valentine leukocidin-induced lung inflammation and injury. Proc Natl Acad Sci U S A 107(12):5587–5592. doi:10.1073/pnas.0912403107
Sicot N, Khanafer N, Meyssonnier V, Dumitrescu O, Tristan A, Bes M, Lina G, Vandenesch F, Vanhems P, Etienne J, Gillet Y (2013) Methicillin resistance is not a predictor of severity in community-acquired Staphylococcus aureus necrotizing pneumonia—results of a prospective observational study. Clin Microbiol Infect 19(3):E142–E148. doi:10.1111/1469-0691.12022
Menif K, Bouziri A, Khaldi A, Hamdi A, Belhadj S, Borgi A, Fitouri Z, Ben Jaballah N (2011) Community-associated methicillin-resistant Staphylococcus aureus infections in a pediatric intensive care unit. J Infect Dev Ctries 5(8):587–591
Kallen AJ, Brunkard J, Moore Z, Budge P, Arnold KE, Fosheim G, Finelli L, Beekmann SE, Polgreen PM, Gorwitz R, Hageman J (2009) Staphylococcus aureus community-acquired pneumonia during the 2006 to 2007 influenza season. Ann Emerg Med 53(3):358–365. doi:10.1016/j.annemergmed.2008.04.027
Hageman JC, Uyeki TM, Francis JS, Jernigan DB, Wheeler JG, Bridges CB, Barenkamp SJ, Sievert DM, Srinivasan A, Doherty MC, McDougal LK, Killgore GE, Lopatin UA, Coffman R, MacDonald JK, McAllister SK, Fosheim GE, Patel JB, McDonald LC (2006) Severe community-acquired pneumonia due to Staphylococcus aureus, 2003–04 influenza season. Emerg Infect Dis 12(6):894–899
Khanafer N, Sicot N, Vanhems P, Dumitrescu O, Meyssonier V, Tristan A, Bès M, Lina G, Vandenesch F, Gillet Y, Etienne J (2013) Severe leukopenia in Staphylococcus aureus-necrotizing, community-acquired pneumonia: risk factors and impact on survival. BMC Infect Dis 13:359. doi:10.1186/1471-2334-13-359
Chibuk T, Cohen E, Robinson J, Mahant S, Hartfield D (2011) Paediatric complicated pneumonia: diagnosis and management of empyema. Paediatr Child Health 16(7):425–429
Otto MP, Martin E, Badiou C, Lebrun S, Bes M, Vandenesch F, Etienne J, Lina G, Dumitrescu O (2013) Effects of subinhibitory concentrations of antibiotics on virulence factor expression by community-acquired methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother 68(7):1524–1532. doi:10.1093/jac/dkt073
Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, Harrison C, Kaplan SL, Mace SE, McCracken GH Jr, Moore MR, St Peter SD, Stockwell JA, Swanson JT, Pediatric Infectious Diseases Society and the Infectious Diseases Society of America (2011) The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis 53(7):e25–e76. doi:10.1093/cid/cir531
Peyrani P, Ramirez J (2015) What is the best therapeutic approach to methicillin-resistant Staphylococcus aureus pneumonia? Curr Opin Infect Dis 28(2):164–170. doi:10.1097/QCO.0000000000000149
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Molecular analysis of strains was performed at the National Staphylococcal Reference Laboratory, Greece, under the scientific responsibility of I.S., funded by the Hellenic Centre for Disease Control and Prevention (HCDCP/KEELPNO, grant C954).
Conflict of interest
E. Drougka has received funding from the National Staphylococcal Reference Laboratory.
M. Tsolia has received investigator-initiated grants from Pfizer and GSK. She has also received honoraria for participation in Advisory Boards of GSK, Pfizer, and Novartis, and for presentations in sponsored symposia by GSK, Pfizer, and Sanofi Pasteur.
For the remaining authors, no conflicts of interest were declared.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Doudoulakakis, A.G., Bouras, D., Drougka, E. et al. Community-associated Staphylococcus aureus pneumonia among Greek children: epidemiology, molecular characteristics, treatment, and outcome. Eur J Clin Microbiol Infect Dis 35, 1177–1185 (2016). https://doi.org/10.1007/s10096-016-2651-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2651-7