Abstract
The present study reports the evolution of the demographic characteristics and the molecular epidemiology of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) in Belgium from 2005 to 2009. Four hundred and ten CA-MRSA isolates were prospectively collected and screened for the presence of Panton–Valentin leucocidin (PVL) and toxic shock syndrome toxin 1 (TSST-1) encoding genes, while clinical information were recorded. PVL- and TSST-1-positive isolates were genotyped by pulsed-field gel electrophoresis (PFGE). Staphylococcal cassette chromosome mec (SCCmec) type, spa type and multilocus sequence type (MLST) were determined on representative isolates. One hundred and fifty-nine (39 %) isolates were PVL-positive. PVL-positive isolates were significantly more frequently isolated from skin or soft tissue than PVL-negative isolates, causing mainly subcutaneous abscesses and furuncles. Patients with PVL-positive CA-MRSA were significantly younger than patients with PVL-negative CA-MRSA. Eighty-seven percent of the PVL-positive isolates belonged to a limited number (n = 7) of PFGE types belonging to sequence types (ST) ST80, ST8, ST30, ST5, ST152, ST338 and a new ST, a single-locus variant of ST1. A temporal evolution of the distribution of these PFGE types was observed, characterised by (1) the dissemination of the ST8-SCCmecIV arcA-positive (USA300) genotype and (2) a genetic diversification. Forty-seven (11 %) strains were TSST-1-positive, of which 65 % clustered into four PFGE types, all belonging to ST5. The epidemiology of CA-MRSA in Belgium is changing, as the rapid diffusion of the USA300 clone seems to occur, together with a clonal diversification.
Similar content being viewed by others
Introduction
The first methicillin-resistant Staphylococcus aureus (MRSA) emerged in the early 1960s, 2 years after methicillin was introduced in medical practice. Since then, MRSA strains have spread globally and caused countless nosocomial outbreaks, making MRSA one of the most common causes of nosocomial infections. Besides these healthcare-associated MRSA (HA-MRSA), MRSA infections now also occur in the community (community-acquired methicillin-resistant S. aureus, CA-MRSA). CA-MRSA infections usually occur in young and healthy patients without any healthcare-associated risks factors for MRSA acquisition. These CA-MRSA strains generally cause mild skin and soft tissue infections, but can also cause life-threatening infections, distinct from those caused by HA-MRSA strains, such as necrotising osteomyelitis and necrotising pneumonia [1]. Classically, CA-MRSA strains possess several distinctive characteristics as compared with HA-MRSA strains: (i) they are often producing the leucocidin of Panton–Valentine (PVL), (ii) they belong to genetic backgrounds unrelated to those of pandemic HA-MRSA clones and (iii) they harbour a staphylococcal cassette chromosome mec (SCCmec) type IV or V [2].
The prevalence of CA-MRSA infections varies widely from one country to another [3]. For example, many differences exist between the epidemiology of CA-MRSA in the USA and in Europe. In the USA, CA-MRSA is one of the most common cause of skin and soft tissue infections in patients from emergency departments and one clone, the USA300 clone (ST8-SCCmec IV), is largely predominant [4]. This clone harbours the arginine catabolic mobile element (ACME), which is thought to enhance its colonising capacities [1]. In Europe, the prevalence of CA-MRSA is much lower but is increasing, especially in countries where the incidence of HA-MRSA is low, such as Denmark or the Netherlands [5]. Many different CA-MRSA clones are found, of which the ST80-SCCmec IV European clone is the most widely disseminated [5]. Recently, however, several European countries have been confronted with the rise of the prevalence of USA300 strains [3, 6].
In Belgium, the first PVL-positive MRSA were reported in 2002–2004 [7]. At that time, infections due to PVL-positive MRSA seemed to be sporadic cases and strains belonged to four major lineages (ST80, ST8, ST30 and ST88) [7]. The majority of strains had a genetic background that was distinct from those of Belgian HA-MRSA epidemic clones, and several cases were imported. The objectives of the present study were to update these data by following the demographic characteristics and molecular epidemiology of PVL-positive CA-MRSA colonisation and infection cases in Belgium from 2005 to 2009.
Materials and methods
Bacterial isolates, clinical and demographic information
Since 2002, all Belgian microbiology laboratories (n ~ 250) are invited by the Reference Laboratory for Staphylococcus aureus (BRLS) to refer for detection of exotoxin genes all CA-MRSA strains defined as strains isolated from ambulatory patients or during the first 48 h of hospitalisation. Each isolate has to be sent with a case report form describing the demographics and clinical mandatory information: sex and age of the patient, clinical site and date of sampling. Additional optional information fields include history of hospitalisation or travel during the year preceding the sampling and if the case is sporadic or part of a cluster.
Identification and susceptibility testing
All isolates sent from January 2005 to December 2009 were confirmed to be MRSA both phenotypically (coagulase test with human plasma and oxacillin susceptibility test using cefoxitin 30-μg discs) [8] and genotypically [detection of 16S rRNA, mecA and nuc genes by multiplex polymerase chain reaction (PCR) assay] [9].
Additionally, isolates collected between January 2005 and February 2008 were tested by disc diffusion for susceptibility to 12 antimicrobial agents (erythromycin, clindamycin, ciprofloxacin, gentamicin, kanamycin, tobramycin, fusidic acid, tetracycline, doxycycline, linezolid, trimethoprim/sulfamethoxazole, mupirocin). Isolates collected from March 2008 to December 2009 were tested by the Vitek 2 automated system (bioMérieux) using the AST-P549 card for the same antimicrobials, except for kanamycin and doxycycline, which are not present on the card, that were tested by disc diffusion, as described above. Clinical and Laboratory Standards Institute (CLSI) breakpoints were used for interpretation [10], except for fusidic acid and mupirocin, for which the Committee for Antimicrobial Testing of the French Society of Microbiology [11] and the British Society for Antimicrobial Chemotherapy (BSAC) [12] criteria were used, respectively.
Exotoxin genes detection
All MRSA isolates were screened for the presence of the PVL, toxic shock syndrome toxin 1 (TSST-1), and exfoliatin A and B encoding genes by PCR [13].
Molecular typing and characterisation
All exotoxin-positive isolates were genotyped by SmaI restriction of genomic DNA resolved by pulsed-field gel electrophoresis (PFGE) and classified as previously described [14]. The NARSA NRS384 strain was used for the USA300 reference profile.
For PVL- and TSST-1 positive isolates, SCCmec type and spa type were determined as previously described [15, 16] on randomly selected representative isolates (one per PFGE type per year). Multilocus sequence typing (MLST) was performed on one isolate per PFGE type randomly selected within the latter subset [17].
All PVL-positive isolates were further screened by PCR for the presence of the arginine deiminase gene (arcA, carried on the ACME) and the exfoliatin D encoding gene (etd), which are recognised as good markers for the USA300 and the European clones, respectively [18], and for the presence of enterotoxin genes (sea, seb, sec, sed, see, seg, seh, sei, sej, sek, sem, sen, seo, sep, seq, ser) [19]. Additionally, the presence of the antibiotic resistance genes aph(3′)-IIIa, ant(4′)-Ia, aac(6′)-Ie + aph(2″), erm (A, B and C) and msrA, tetK and tetM was searched by PCR on all kanamycin-, tobramycin-, gentamicin-, erythromycin- and tetracycline-resistant PVL-positive isolates, respectively [20–22].
Results
Participation and bacterial isolates
From January 2005 to December 2009, the BRLS received from 74 laboratories a total of 410 non-duplicated MRSA: nine laboratories of the Brussels-Capital region (that accounts for 10 % of the total Belgian population) sent 109 isolates (27 %), 44 laboratories located in the Flanders region (58 % of the Belgian population) sent 199 isolates (49 %) and 21 laboratories located in Wallonia (32 % of the population) sent 102 isolates (25 %). The relative proportion of isolates sent per region remained stable over the 5 years, except in 2009, where up to 45 % of the isolates received were from the Brussels-Capital region.
One hundred and fifty-nine isolates harboured the PVL-encoding genes, 47 the tst gene and two the eta gene. The number of PVL-positive isolates received per year increased progressively from 18 in 2005 to 48 in 2009, representing, every year, about 40 % (range 32 to 45 %) of the total number of isolates received (Fig. 1).
Demographic and clinical data
Three hundred and eighty case report forms (150 from PVL-positive and 230 from PVL-negative isolates) were available for analysis (Table 1). Patients with PVL-positive CA-MRSA had a Gaussian age distribution with a median of 23 years, which was significantly younger than the median observed among patients with PVL-negative CA-MRSA. The male/female ratio was 1.4. PVL-positive isolates were significantly more frequently isolated from skin or soft tissue (77 %) than PVL-negative isolates (37 %), causing significantly more subcutaneous abscesses and furuncles (Table 1). TSST-1-positive isolates were also observed more often in younger patients (median 20 years) compared to the other PVL-negative isolates and were significantly more frequently isolated from ear, nose and throat (ENT) specimens (8 out of the 40 evaluable forms reported an ear specimen).
Additional optional information was only available for about half of the isolates (see Table 1). When reported, hospitalisation or chronic pathology with frequent contacts with hospital were more frequently associated with PVL-negative isolates (85 cases), while travel within the preceding year was more frequently associated with PVL-positive isolates (22 cases). Few clusters were reported, three involving PVL-negative isolates (n = 11) and five involving PVL-positive isolates (n = 14). Four out of the five clusters involving PVL-positive isolates were related to travel abroad (Egypt, USA, Turkey and India).
Molecular typing results
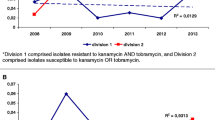
Eighty-seven percent of the 159 PVL-positive isolates belonged to seven genotypes: PFGE X1-spa t044-ST80-SCCmec IV (n = 76), A24-spa t008-ST8-SCCmec IV (n = 34), J4-spa t019-ST30-SCCmec IV (n = 12), XX1-spa t345-New ST (SLV of ST1)-SCCmec V (n = 6), W1-spa t437–ST338-SCCmec V (n = 4), U1–spa t355-ST152-SCCmec V (n = 4) and C3-spa t002-ST5-SCCmec V (n = 3) (Fig. 1, Table 2). All A24-spa t008-ST8-SCCmec IV strains carried the arcA gene.
A temporal evolution of the distribution of these different genotypes was observed (Fig. 1) and was mainly characterised by (1) the rising of the A24-spa t008-ST8-SCCmec IV genotype (from 0 % in 2005 to 33 % in 2009) and (2) a genetic diversification from six different PFGE types (belonging to three different MLST CCs) in 2005 to 14 PFGE types (belonging to nine CCs) in 2009. We found no significant association between clusters or travel abroad and a particular genotype, but the samples sizes were small. The four travel-related clusters were due to four distinct genotypes: X1-spa t044-ST80-SCCmec IV (Egypt), A24-t008-ST8-SCCmec IV (USA), J4-t019-ST30-SCCmec IV (Turkey) and XX1-t345-New ST (SLV of ST1)-SCCmec V (India).
Twenty-eight (65 %) of the 47 TSST-1-positive strains belonged to four PFGE types: C3 (n = 12), C4 (n = 11), C6 (n = 3) and G10 (n = 5), all belonging to ST5 by MLST and harbouring spa t002 or related spa types, but distinct SCCmec types. C3 and C4 strains were SCCmec I, C6 strains were SCCmec I (n = 1) or non-typable (NT, n = 2), and G10 strains were SCCmec II. The two eta-positive isolates harboured unrelated PFGE types.
Susceptibility and resistance genes profiles
The majority of PVL-positive CA-MRSA isolates was kanamycin- and tetracycline-resistant (74 and 57 %, respectively), which was significantly more than among PVL-negative isolates (Table 3). Up to 41 % of strains were resistant to fusidic acid, which was not significantly more than that observed among PVL-negative isolates (Table 3). Thirty-seven percent of strains were erythromycin resistant. Resistance to gentamicin (4 %), trimethoprim/sulfamethoxazole (3 %) and doxycycline (7 %) was low, as well as resistance rates to tobramycin (6 %), clindamycin (2 %) and ciprofloxacin (15 %), which were significantly lower than for PVL-negative isolates (Table 3).
Resistance profiles, strongly linked to genotypes, followed the epidemiological changes over time (Table 3). This led to an increase in the proportion of erythromycin- and ciprofloxacin-resistant PVL-positive MRSA strains (due to the dissemination of the USA300 arcA-positive A24-ST8-SCCmec IV clone) and a decrease in the proportion of tetracycline- and fusidic acid-resistant PVL-positive MRSA strains (characteristic of the European X1-ST80-SCCmec IV clone). Of note, TSST-1-positive major clones also differed by their resistance profiles, and all C3, C4 and C6 ST5-SCCmec I isolates were fusidic acid-resistant as opposed to G10 ST5-SCCmec II isolates.
Among PVL-positive isolates, tetracycline resistance was mainly mediated by the tetK gene (96 %). The most prevalent aminoglycoside resistance gene was aph(3′)-IIIa, present in 94 % of the 126 kanamycin non-susceptible isolates (mostly belonging to X1-ST80-SCCmec IV and A24-ST8-SCCmec IV clones). aac(6′)-Ie + aph(2″) was found in the seven isolates combining kanamycin, tobramycin and gentamicin resistance (mainly U1-ST152-SCCmec V and C3-ST5-SCCmec V), while ant(4′)-Ia was rarely observed (Table 3). Macrolides resistance was mediated by msrA in a majority of erythromycin-resistant isolates (61 %), which belonged mostly to the A24-ST8-SCCmec IV clone. By contrast, ermC, which was less frequent (34 %), was the gene harboured by the erythromycin-resistant X1-ST80-SCCmec IV isolates (Table 3).
Toxin genes profiles
The distribution of toxin genes was also strongly linked to the PFGE type. The X1-ST80-SCCmec IV type was associated with the carriage of etD and the lack of enterotoxin genes, while the A24 and A23 (ST8-SCCmec IV) isolates harboured the sek and seq enterotoxin genes. sek and seq were also present in W1-ST338-SCCmec V isolates, together with seb. The egc complex (seg-sei-sem-sen-seo) was present in L1-ST22-SCCmec IV and ZA3-ST5-SCCmec IV isolates, in XX1-New ST (single-locus variant of ST1)-SCCmec V isolates (in association with sea) and in C3-ST5-SCCmecV isolates (in association with sed-sej-sel). U1-ST152-SCCmec V isolates lacked any toxin gene targeted (Table 2).
Discussion
In Belgium, the first PVL-positive CA-MRSA isolate was reported in 2002, leading the BSRL to issue alert messages to microbiology laboratories about the need to refer CA-MRSA for the detection of exotoxin genes. At that time, infections due to PVL-positive CA-MRSA seemed to be sporadic cases and isolates belonged to four major lineages, the large majority belonging to the ST80-SCCmec IV European clone [7]. The present study updates these data by following the epidemiology of CA-MRSA cases from 2005 to 2009.
Our survey bears the obvious limitation of being voluntary based, which has the likely consequence of underestimating the true occurrence of CA-MRSA infections. Another drawback is the lack of answers in about half of the report forms concerning important epidemiological information such as healthcare-associated risk factors or travel abroad. However, it presents the advantage to be prospective, nationwide and to cover a 5-year period.
The number of CA-MRSA isolates received per year progressively increased from 48 in 2005 to 130 in 2009. As our survey is voluntary based, the reasons for this increase are difficult to ascertain. It could reflect a true increase in the CA-MRSA incidence, simply be due to an “artefactual” increase of sampling and/or sending due to a progressively growing awareness of laboratories and field practitioners regarding the CA-MRSA threat, or be the result of a mix of these two phenomenons. The majority of isolates received (about 60 % in each year) were PVL negative. PVL-negative isolates affected older patients than PVL-positive isolates, and about up to 30 % of them were recovered from admission screening samples. A recent study conducted in Belgian hospitals has demonstrated that previous healthcare exposure remains the main risk factor for MRSA carriage on admission [23]. However, when answered, the absence of previous hospitalisation or chronic pathology with frequent contacts with hospital was reported in 40 % of our PVL-negative CA-MRSA cases. In Belgium, the dissemination of HA-MRSA strains to long-term care facilities, serving as a reservoir of carriers, is a well-known phenomenon [24] that might account for part of these PVL-negative cases that could be considered as ‘healthcare-associated CA-MRSA’ (hCA-MRSA).
PVL-positive CA-MRSA received per year also tripled from 2005 to 2009, causing predominantly skin and soft tissue infections in young adults. Recent travel abroad was reported for a few cases. As compared to 2002–2004, the number of X1-ST80-SCCmec IV isolates remained stable (about 15/year), making the European clone the predominant PVL-positive CA-MRSA clone in Belgium. Similarly, the less frequent J4-ST30-SCCmec IV South West Pacific clone has remained stable since 2002–2004. On the other hand, the number of USA300 A24-ST8-SCCmec IV isolates has progressively increased and the USA300 clone became, in 2009, as frequently reported as the European clone, with apparently no association with travel abroad. Interestingly, and despite the fact that—our survey being voluntary based—no firm conclusion can be drawn regarding the exact incidence of each genotype, this USA300 progressive increase, together with a growing number of several other recent but less diffused genotypes, seem to add themselves to the stable burden caused by the European clone instead of replacing it.
The large majority of PVL-positive CA-MRSA isolates belonged to genetic backgrounds that are distinct from those of nosocomial MRSA strains from Belgian hospitals, except for A23/A24-spa t008-ST8-SCCmec IV and C3-spa t002-ST5-SCCmec V, which appear related to the widely disseminated hospital A20/A21 t008-ST8-SCCmec IV and C3 t002-ST5-SCCmec IV MRSA clones, respectively. However, ST8 and ST5 CA-MRSA differ from ST8 and ST5 HA-MRSA by their mobile genes content: A21/A20-ST8-SCCmec IV HA-MRSA isolates harbour the sea gene, lack PVL genes and carry ant(4′) and ermA resistance genes [25, 26], while A24-spa t008-ST8-SCCmec IV CA-MRSA harbour PVL genes, arcA, sek and seq, msrA and aph3′. Similarly, C3-spa t002-ST5 CA-MRSA and HA-MRSA differ by the SCCmec type they harbour, the PVL and aac-aph genes. These multiple differences suggest, rather, a divergent evolution (in hospitals and in the community) of strains belonging to a common genetic background than the ‘adaptation’ of local HA-MRSA clones to the community setting as the source of these PVL-positive CA-MRSA clones.
Eighteen percent of the PVL-negative isolates were found to be TSST-1-positive, and the majority of them (65 %) belonged to four genotypes: C3, C4 and C6-ST5-SCCmec I, and G10-ST5-SCCmec II. The exact genetic relatedness of TSST-1-positive C3 ST5-SCCmec I and G10 ST5-SCCmec II CA-MRSA with the closely related C3 t002-ST5-SCCmec IV and G10 t002-ST5-SCCmec II HA-MRSA clones has to be further studied. However, the majority of G10 HA-MRSA strains do possess the tst gene [25], suggesting that G10 HA-MRSA could be a likely origin for the G10 CA-MRSA observed here. On the contrary, C3 TSST-1-positive CA-MRSA do differ from C3 HA-MRSA by the SCCmec type they harbour, their resistance to fusidic acid and the tst gene. These C3 TSST-1-positive CA-MRSA could have been imported from France, where a similar TSST-1-positive ST5 SCCmec I CA-MRSA clone has recently been reported [27].
In conclusion, the epidemiology of CA-MRSA in Belgium is changing, as the rapid diffusion of the USA300 clone seems to occur, together with a clonal diversification. These epidemiological changes underline the importance of surveillance and typing data to monitor the CA-MRSA evolving epidemiology and control the spread of these organisms in the general population.
References
David MZ, Daum RS (2010) Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev 23(3):616–687
Rasigade JP, Laurent F, Lina G, Meugnier H, Bes M, Vandenesch F et al (2010) Global distribution and evolution of Panton–Valentine leukocidin-positive methicillin-susceptible Staphylococcus aureus, 1981–2007. J Infect Dis 201(10):1589–1597
Otter JA, French GL (2010) Molecular epidemiology of community-associated meticillin-resistant Staphylococcus aureus in Europe. Lancet Infect Dis 10(4):227–239
Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB et al (2006) Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med 355(7):666–674
Witte W (2009) Community-acquired methicillin-resistant Staphylococcus aureus: what do we need to know? Clin Microbiol Infect 15(Suppl 7):17–25
Blanco R, Tristan A, Ezpeleta G, Larsen AR, Bes M, Etienne J et al (2011) Molecular epidemiology of Panton–Valentine leukocidin-positive Staphylococcus aureus in Spain: emergence of the USA300 clone in an autochthonous population. J Clin Microbiol 49(1):433–436
Denis O, Deplano A, De Beenhouwer H, Hallin M, Huysmans G, Garrino MG et al (2005) Polyclonal emergence and importation of community-acquired methicillin-resistant Staphylococcus aureus strains harbouring Panton–Valentine leucocidin genes in Belgium. J Antimicrob Chemother 56(6):1103–1106
Roisin S, Nonhoff C, Denis O, Struelens MJ (2008) Evaluation of new Vitek 2 card and disk diffusion method for determining susceptibility of Staphylococcus aureus to oxacillin. J Clin Microbiol 46(8):2525–2528
Hallin M, Maes N, Byl B, Jacobs F, De Gheldre Y, Struelens MJ (2003) Clinical impact of a PCR assay for identification of Staphylococcus aureus and determination of methicillin resistance directly from blood cultures. J Clin Microbiol 41(8):3942–3944
Clinical and Laboratory Standard Institute (CLSI) (2006) Performance standards for antimicrobial disk susceptibility tests; Approved standard—ninth edition. CLSI document M2-A9. CLSI, Wayne
Comité de l’Antibiogramme de la Société française de Microbiologie (2008) Recommandations. http://www.sfm-microbiologie.org/pages/?page=746&id_page=182. January 2008
British Society for Antimicrobial Chemotherapy (BSAC) (2007) BSAC Methods for Antimicrobial Susceptibility Testing. Available online at: http://bsac.org.uk/wp-content/uploads/2012/02/version_6.1.pdf
Jarraud S, Mougel C, Thioulouse J, Lina G, Meugnier H, Forey F et al (2002) Relationships between Staphylococcus aureus genetic background, virulence factors, agr groups (alleles), and human disease. Infect Immun 70(2):631–641
Deplano A, Witte W, van Leeuwen WJ, Brun Y, Struelens MJ (2000) Clonal dissemination of epidemic methicillin-resistant Staphylococcus aureus in Belgium and neighboring countries. Clin Microbiol Infect 6(5):239–245
Kondo Y, Ito T, Ma XX, Watanabe S, Kreiswirth BN, Etienne J et al (2007) Combination of multiplex PCRs for staphylococcal cassette chromosome mec type assignment: rapid identification system for mec, ccr, and major differences in junkyard regions. Antimicrob Agents Chemother 51(1):264–274
Hallin M, Deplano A, Denis O, de Mendonça R, De Ryck R, Struelens MJ (2007) Validation of pulsed-field gel electrophoresis and spa typing for long-term, nationwide epidemiological surveillance studies of Staphylococcus aureus infections. J Clin Microbiol 45(1):127–133
Enright MC, Day NP, Davies CE, Peacock SJ, Spratt BG (2000) Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J Clin Microbiol 38(3):1008–1015
Strommenger B, Braulke C, Pasemann B, Schmidt C, Witte W (2008) Multiplex PCR for rapid detection of Staphylococcus aureus isolates suspected to represent community-acquired strains. J Clin Microbiol 46(2):582–587
Omoe K, Hu DL, Takahashi-Omoe H, Nakane A, Shinagawa K (2005) Comprehensive analysis of classical and newly described staphylococcal superantigenic toxin genes in Staphylococcus aureus isolates. FEMS Microbiol Lett 246(2):191–198
Lina G, Quaglia A, Reverdy ME, Leclercq R, Vandenesch F, Etienne J (1999) Distribution of genes encoding resistance to macrolides, lincosamides, and streptogramins among staphylococci. Antimicrob Agents Chemother 43(5):1062–1066
Ng LK, Martin I, Alfa M, Mulvey M (2001) Multiplex PCR for the detection of tetracycline resistant genes. Mol Cell Probes 15(4):209–215
Vanhoof R, Godard C, Content J, Nyssen HJ, Hannecart-Pokorni E (1994) Detection by polymerase chain reaction of genes encoding aminoglycoside-modifying enzymes in methicillin-resistant Staphylococcus aureus isolates of epidemic phage types. Belgian Study Group of Hospital Infections (GDEPIH/GOSPIZ). J Med Microbiol 41(4):282–290
Vandendriessche S, Hallin M, Catry B, Jans B, Deplano A, Nonhoff C et al (2012) Previous healthcare exposure is the main antecedent for methicillin-resistant Staphylococcus aureus carriage on hospital admission in Belgium. Eur J Clin Microbiol Infect Dis 31(9):2283–2292
Denis O, Jans B, Deplano A, Nonhoff C, De Ryck R, Suetens C et al (2009) Epidemiology of methicillin-resistant Staphylococcus aureus (MRSA) among residents of nursing homes in Belgium. J Antimicrob Chemother 64(6):1299–1306
Denis O, Deplano A, Nonhoff C, Hallin M, De Ryck R, Vanhoof R et al (2006) In vitro activities of ceftobiprole, tigecycline, daptomycin, and 19 other antimicrobials against methicillin-resistant Staphylococcus aureus strains from a national survey of Belgian hospitals. Antimicrob Agents Chemother 50(8):2680–2685
Hallin M, de Mendonça R, Denis O, Lefort A, El Garch F, Butaye P et al (2011) Diversity of accessory genome of human and livestock-associated ST398 methicillin resistant Staphylococcus aureus strains. Infect Genet Evol 11(2):290–299
Robert J, Tristan A, Cavalié L, Decousser JW, Bes M, Etienne J et al (2011) Panton–Valentine leukocidin-positive and toxic shock syndrome toxin 1-positive methicillin-resistant Staphylococcus aureus: a French multicenter prospective study in 2008. Antimicrob Agents Chemother 55(4):1734–1739
Acknowledgements
We thank all the participating microbiology laboratories for referring us their CA-MRSA strains.
We thank Sylvianne Rottiers, Emilie Vandaele and Karim El Kadaani for their skilled technical assistance.
Part of this work was presented at the 19th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID), Helsinki, Finland, May 2009.
Funding
The BRLS is supported by the Belgian Antibiotic Policy Coordination Committee (BAPCOC), Ministry of Public Health, Belgium.
Transparency declarations
None to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Brauner and M. Hallin contributed equally to this work.
Rights and permissions
About this article
Cite this article
Brauner, J., Hallin, M., Deplano, A. et al. Community-acquired methicillin-resistant Staphylococcus aureus clones circulating in Belgium from 2005 to 2009: changing epidemiology. Eur J Clin Microbiol Infect Dis 32, 613–620 (2013). https://doi.org/10.1007/s10096-012-1784-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1784-6