Abstract
The purpose of this paper is to determine the prevalence of the toxic shock toxin gene (tst) and to enumerate the circulating strains of methicillin-sensitive Staphylococcus aureus (MSSA) and methicillin-resistant S. aureus (MRSA) in Australian isolates collected over two decades. The aim was to subtype these strains using the binary genes pvl, cna, sdrE, pUB110 and pT181. Isolates were assayed using real-time polymerase chain reaction (PCR) for mecA, nuc, 16 S rRNA, eight single-nucleotide polymorphisms (SNPs) and for five binary genes. Two real-time PCR assays were developed for tst. The 90 MRSA isolates belonged to CC239 (39 in 1989, 38 in 1996 and ten in 2003), CC1 (two in 2003) and CC22 (one in 2003). The majority of the 210 MSSA isolates belonged to CC1 (26), CC5 (24) and CC78 (23). Only 18 isolates were tst-positive and only 15 were pvl-positive. Nine MSSA isolates belonged to five binary types of ST93, including two pvl-positive types. The proportion of tst-positive and pvl-positive isolates was low and no significant increase was demonstrated. Dominant MSSA clonal complexes were similar to those seen elsewhere, with the exception of CC78. CC239 MRSA (AUS-2/3) was the predominant MRSA but decreased significantly in prevalence, while CC22 (EMRSA-15) and CC1 (WA-1) emerged. Genetically diverse ST93 MSSA predated the emergence of ST93-MRSA (the Queensland clone).
Similar content being viewed by others
Introduction
The pathogenicity of Staphylococcus aureus can, in part, be attributed to the production of pyrogenic toxins such as toxic shock toxin-1 (TSST-1) [1]. TSST-1 is a 21.9-kDa protein that is encoded by the S. aureus toxic shock toxin (tst) gene [2]. The release of TSST-1 into the bloodstream may give rise to a variety of severe clinical conditions, such as toxic shock syndrome (TSS), sudden infant death syndrome, neonatal TSS-like exanthematous disease (NTED) and Kawasaki syndrome. The tst gene is present in up to 70% of the S. aureus strains isolated from patients with TSS. Without appropriate therapy, lethal shock may develop within 24 h after the onset of symptoms. Although most cases of TSS are associated with tampon use, an increasing number of cases are related to localised infections, surgical complications and insect bites [1–4].
There has been a worldwide increase in the frequency of clusters of TSS since the 1980s, but this has not been noted specifically in cases reported from Australia. In 1983, the Communicable Diseases Intelligence reported 11 cases of toxic shock in 1981, seven in 1982 and four in 1983 in Australia [5]. The Therapeutic Goods Administration stated that, between 1982 and 1994, there were 38 reports of TSS in Australia, of which three cases were fatal and ten were female non-menstrual cases [6]. In 1996, Robinson et al. reported the result of two surveys to identify TSS cases in the period 1990–1994. Their survey revealed 11 possible cases of TSS from intensive care units (ICUs) in Australia and New Zealand and 12 TSS cases from Victoria, Australia [7]. A search by Donovan et al. for possible fatal cases of TSS, by reviewing the records of females whose deaths were registered in 1978–1979, revealed that unrecognised TSS could not be excluded as the cause of one of the deaths [8]. A number of isolated case reports of TSS have been published, including TSS associated with newly diagnosed type I diabetes mellitus [9] and TSS in a male complicated by oliguric acute renal failure [10]. Reports of shock associated with S. aureus infection which resembled TSS but not reported as such include the death of 12 children after receiving a S. aureus-contaminated diphtheria toxin–antitoxin mixture and a case of late-onset warfarin necrosis [11, 12]. In 2005 a case of menstrual TSS was reported by MacIsaac et al., indicating that toxic shock Staphylococcus is still a problem [13].
TSST-1 has been frequently associated with MSSA, but, recently, community-acquired and hospital-acquired tst-positive methicillin-resistant S. aureus (MRSA) has been reported in Europe and Japan [14–18]. The paucity of ongoing reports on TSS and the absence of reports indicating an increase of TSS in Australia raises the question of whether the TSST-1 gene is common in S. aureus in Australia. It has been postulated that modifications to the host population, such that the fitness of organisms already carrying TSST-1 genes increases, could result in an increase in TSS [19].
TSS has been frequently associated with ST30-MSSA [14]. The prevalence of MSSA strains in Australia is not well described, as previous studies have focussed on MRSA and, even for MRSA molecular strain typing of large collections of clinical isolates, has only been available relatively recently. However, it is clear that ST239-MRSA-III (also known in Australia as EA-MRSA or AUS-2/3 MRSA) has been the dominant healthcare-associated strain of MRSA in Australia since the late 1970s, while more recently, ST22-MRSA-IV (EMRSA-15) has also become established in this niche [20–-22].
The aims of this study were to determine the prevalence of the tst gene and to enumerate the circulating strains of S. aureus, including methicillin-resistant S. aureus (MRSA), in a substantial Australian collection of isolates encompassing the period 1989–2003. The detection of a small set of other binary genes including potential virulence factors and integrated plasmids was also undertaken to confirm its utility as a method of subtyping. This set included pvl, which was of particular interest given the recent emergence of pvl-positive MRSA in the community in Australia.
Materials and methods
Selection of archival isolates
Three hundred S. aureus isolates collected at the Princess Alexandra Hospital as part of the Australian Group for Antimicrobial Resistance (AGAR) in the 1989, 1996 and 2003 national staphylococcal surveys were examined. AGAR studies have shown that the same MRSA strains are present throughout Australia, albeit in differing proportions [23, 24]. It is, therefore, likely that this collection is representative of circulating S. aureus in Australia. The same sampling methodology was used in all three year groups and there was no distinction made between community- and healthcare-associated isolates. The isolates were from specimens submitted for clinical diagnosis and not for infection control screening and duplicates were excluded [20].
After the isolates were retrieved from storage at −80°C, there were 91 pure S. aureus isolates from 1989, 104 from 1996 and 105 from 2003.
DNA extraction
Isolates were grown on horse blood agar in air at 37°C overnight. One microlitre loop of pure 24-h colonies were emulsified into 250 μL of water in a 1.5-mL simple prelabelled microtube and DNA extraction was performed using the MagNA Pure LC Total Nucleic Acid Isolation Kit on the Roche MagNA Pure instrument.
Amplification of the 16 S ribosomal DNA was used to confirm the quality of each DNA extract and the absence of polymerase chain reaction (PCR) inhibitors.
Detection of the tst gene
To determine the optimal primer set for the detection of the tst gene, two assays were developed, using the two primer sets previously described in the literature and aimed at different areas of the tst gene [1, 25]. Primer sets were supplied by Sigma Genosys. The tst gene was detected using real-time PCR with SYBR Green on a Rotor-Gene 3000 (Corbett Research, Mortlake, Australia).
The conditions of the assay were: 50°C for 2 min, 95°C for 2 min, 40 cycles of 95°C for 15 s, 56°C for 20 s, 72°C for 35 s; melt 72°C to 99°C at 1°C intervals.
The gene was considered to be detected if the cycle threshold (Ct) was crossed in a predetermined Ct interval within which all positive control strains were positive and all negative control strains were undetected.
Strain typing
Real-time PCR assays for mecA, nuc and 16 S rRNA genes were performed on all isolates to confirm the identity and methicillin resistance, based on publications by Barski et al. and Unal et al. [26, 27].
Real-time PCR typing of S. aureus is based on a previous publication by Huygens et al. [28], for single-nucleotide polymorphisms (SNPs) derived from the multi-locus sequence typing (MLST) database of seven housekeeping genes. The method involves eight PCRs for arcC210, tpi241 + tpi243, arcC162, gmk318, pta294, tpi36 (tpi36*C and tpi36*T) and pta383. It is able to distinguish between major clonal complexes (CCs) and is largely concordant with the population structure of S. aureus as determined by MLST. A single SNP-based PCR to detect aroE525G was added to confirm the identity of ST93 (the Queensland clone) when the appropriate seven-SNP profile (TGGTTCTA) was obtained. The binary genes interrogated were pvl, cna, sdrE, pUB110 and pT181 according to Huygens et al. [28]. The presence of the genes was detected using real-time PCR with SYBR Green on a Rotor-Gene 3000 (Corbett Research, Mortlake, Australia). The genes were considered to be detected if the threshold was crossed within the predetermined Ct.
Statistical analysis
Confidence interval calculations for proportions and Chi-square analysis for probability estimates were performed using the VassarStats web site (http://faculty.vassar.edu/lowry/VassarStats.html).
Results
Prevalence of clonal complexes of MRSA and MSSA
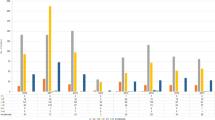
SNP profiles of the isolates correlated with 21 CCs or sequence types (STs): 91 with CC239, 28 with CC1, 24 with CC5, 23 with CC78, 22 with CC15 and 22 with CC45. CC239 was the major strain for 1989 (43/91), followed by CC45 (10/91) and CC15 (6/91). CC239 was, again, the major strain in 1996 (38/104), followed by CC1 (13/104) and CC78 (11/104). In 2003, CC5 was predominant with 15/105, followed by both CC1 and CC15 with 11/105, and both CC239 and CC78 with 10/105 (Table 1).
Ninety isolates were confirmed as MRSA and the SNP profiles of the isolates correlated with three CCs: 87 with CC239, two with CC1 (WA-1) and one with CC22 (EMRSA-15). There were 39 (42.9%; 95% confidence interval [CI] 33.2–53.1%) MRSA isolates in the 1989 collection and 38 (36.5; 95% CI 27.9–46.1%) in 1996, all CC239 (AUS-2/3). In 2003, there were only 13 (12.4%; 95% CI 7.4–20.0%) MRSA isolates (P < 0.0001), of which ten were CC239, two CC1 (WA-1) and one CC22 (EMRSA-15).
Of 210 MSSA isolates, 26 (12.4%) were CC1, 24 (11.4%) CC5, 23 (11.0%) CC78, 22 (10.5%) CC15, 22 (10.5%) CC45 and 17 (8.1%) CC30. The predominant strains for 1989 were CC45 (10/52) and CC15 (6/52), for 1996 CC1 (13/66) and CC78 (11/66), and for 2003 CC5 (15/92), CC15 (11/92), followed by CC78 (10/92). The yearly variation in the prevalence of major clones was not statistically significant. Nine MSSA isolates belonged to ST93: four were in 1989, two in 1996 and three in 2003. Five binary types of ST93 were described, including two in which pvl was present. Three of the five types including both pvl-positive types were seen in the isolates from 1989. Overall, five MSSA isolates were pvl-positive in each year. In 1989, 3/5 pvl-positive MSSA isolates belonged to ST93, 1/5 to CC1 and 1/5 to CC30; in 1996, 2/5 belonged to CC30, 2/5 to CC1 and 1/5 to ST93; and in 2003, 2/5 belonged to CC30, 1/5 to CC1, 1/5 to ST93 and 1/5 to CC25. No MRSA were pvl-positive.
Prevalence of tst-positive isolates
The tst gene was present in 18 isolates (6%; 95% CI 3.8–9.3%) overall. The annual prevalence did not vary significantly (P = 0.289) with three (3.3%; 95% CI 1.1–9.3%) isolates being positive in 1989, six (5.8%; 95% CI 2.7–12.0%) positive in 1996 and nine (8.6%; 95% CI 4.6–15.5%) positive in 2003. Based on the SNP type correlation, CC30 was predominant with 11 isolates, followed by two isolates correlating with CC45 and two with CC8, followed by the rest (Table 2).
CC30 was the predominant strain for tst-positive isolates in all three years, with 2/3 isolates being tst-positive in 1989 and the remaining tst-positive isolate for 1989 was the sole isolate with an SNP profile consistent with ST67, ST198, ST395, ST426, ST479, ST66, ST68 or ST520. In 1996, 4/6 CC30, 1/7 CC45 and 1/1 CC72 isolates were tst-positive and in 2003, 5/9 CC30, 2/6 CC8, 1/5 CC45 and 1/3 ST93 isolates were tst-positive.
tst-positive isolates were from a variety of sites, none were from the female genital tract and none of the patients were considered to have TSS. There were equal numbers of male and female patients with isolates positive for the tst gene. The ages of patients ranged from 14 to 86 years. None of the tst-positive isolates had the mecA or pvl gene detected. The binary gene results are summarised in Table 2.
Discussion
TSST-1 is a superantigenic toxin encoded by the tst gene in S. aureus and is associated with TSS amongst various clinical diseases. TSST-1 was the first of a number of toxins associated with TSS and is the major exotoxin aetiologically involved in staphylococcal TSS, especially in menstrual cases [29]. Methods based on the detection of the toxin depend on the concentration of toxin expressed and can be negatively influenced by various factors [29]. Detection of the tst gene by PCR can overcome these difficulties if a representative clinical isolate is available. In this study, we have shown that the prevalence of tst in a substantial collection of S. aureus is low and has not changed significantly over two decades. This provides a plausible explanation for the low reportage of staphylococcal TSS in Australia.
The genotyping data in this study provides a unique picture of prevalent S. aureus strains in Australia over two decades, as previous studies have been restricted to MRSA or to a short time-frame [21, 22]. Detection of the binary genes and integrated plasmids adds further discrimination and potentially significant information on the prevalence of toxins of clinical interest, such as tst and pvl.
Among the 90 MRSA isolates, CC239 MRSA (AUS-2/3) was the overall predominant strain and also the sole strain in 1989 and 1996. CC1 MRSA (WA-1) and CC22 MRSA (EMRSA-15) only appeared in 2003. However, the total number of MRSA isolates decreased significantly in that year due to a marked decrease in CC239. The presence of CC239 (which has previously been shown to be synonymous with ST239-MRSA-III) as the only MRSA clone in the 1989 and 1996 surveys is in keeping with previous studies [20, 21]. ST239-MRSA-III (also known in Australia as EA-MRSA or AUS-2/3 MRSA) has been the dominant healthcare-associated strain of MRSA in Australia since the late 1970s. However, to our knowledge, the molecular typing of MRSA in Queensland by a method referrable to MLST had not been undertaken on isolations made prior to 2000. Our results provide further evidence of the ubiquity of this international epidemic clone in eastern Australia in the late 20th century. The importation of other strains of MRSA, such as EMRSA-15, into Australia and the emergence of still more local strains, including WA-1, since 2000 has been described previously and is in keeping with our findings [20, 21]. Of 210 MSSA isolates, the major clones present were CC1, CC5, CC78, CC15, CC45 and CC30. Of these, all but CC5 and CC78 were major clones present in the Oxfordshire collection [30]. However, CC5 was also represented by a substantial number of isolates in that study, but was characterised as a minor group at that time. CC78, on the other hand, was not present at all. Australia has been the major source of STs (six of 18) belonging to this CC in the MLST database. Most of the registered isolates (22 of 28) have been MRSA [31].
MSSA isolates belonging to ST93 were detected in each survey year. This sequence type is a singleton apparently unique to Australia and distinct from other lineages [31, 32]. The MRSA clone of this sequence type was first described in Queensland in 2000 [33]. A subsequent clinical cohort study conducted in the same region in 2004 and 2005 identified five binary types among MSSA isolates and only one for ST93-MRSA (a pvl-positive clone) [22]. Similarly, five binary types of ST93-MSSA were detected in this study. Three of these five types, including two pvl-positive types, were present among the 1989 isolates, thus, demonstrating that a diverse population of ST93 was present in south-east Queensland prior to the emergence of the Queensland clone by acquisition of SCCmec type IV.
The number of pvl-positive isolates was surprisingly low: 15 MSSA overall (5%), with five in each year group. A clinical cohort study in 2004–2005 in the same region showed a pvl prevalence of 16% in 192 MSSA isolates [22]. In addition, the majority (55%) of non-multiresistant MRSA isolates in the same study were also pvl-positive, thus, suggesting that there has been an increase in the prevalence of pvl in circulating S. aureus. In the current study, most pvl-positive isolates belonged to CC30 (five) or ST93 (five), the same lineages as the major pvl-positive community-associated MRSA clones that have expanded over the last decade. Thirteen of 15 pvl-positive isolates were from skin and soft tissue specimens, and the other 2/15 from respiratory specimens. The majority (11/15) of the pvl-positive isolates were considered to be community-acquired, 1/15 was considered to be hospital-acquired and the acquisition of the remaining 3/15 was not known.
TSST-1 has been frequently associated with MSSA ST30, but, recently, community-acquired and hospital-acquired tst-positive MRSA belonging to ST5 and ST30 has been reported in Europe and Japan [14–18]. All of our tst-positive isolates were MSSA and, perhaps predictably, the majority of these (11/18) belonged to CC30. In addition, the majority (11/17) of all CC30 isolates were tst-positive.
The tst-positive isolates in this study were from a variety of sites, including superficial sites and deep sterile sites, in patients of widely varying age. While none of these patients had TSS, this is not surprising as the production and penetration of sufficient concentration of TSST-1 is required for the development of TSS [34] and only occurs in a subset of infections due to tst-positive strains.
There have been recent overseas publications drawing attention to infection due to TSST-1-positive S. aureus [14, 15, 35, 36]. For example, TSST-1 has been involved in an outbreak of neonatal toxic shock-like exanthematous disease in a neonatal intensive care unit in Japan [35]. The emergence of TSST-1-positive community-associated MRSA strains may lead to higher rates of TSS among the young, with attendant impact on infection control and empiric therapeutic strategies [14]. The recently reported tst-positive MRSA clones ST5 and ST30 have been associated with both hospital-acquired and community-acquired infections causing a variety of clinical syndromes, including TSS and suppurative infections. Recent studies have shown that tst-positive MSSA strains belonging to ST1, ST8 and ST30 are a potential source of tst-positive community-acquired MRSA and that the pulsotype of tst-positive MRSA clones have been found to differ from that of MSSA by a single band involving the SCCmec element. These findings suggest that the tst-positive MRSA clones may have emerged from their respective MSSA counterparts and have the same sequence type (ST5) of two pandemic nosocomial MRSA clones [15, 37]. These publications support the desirability for the ongoing surveillance of MRSA and MSSA harbouring the tst gene as an aid to targeted infection control.
References
Deurenberg RH, Nieuwenhuis RF, Driessen C, London N, Stassen FR, van Tiel FH, Stobberingh EE, Vink C (2005) The prevalence of the Staphylococcus aureus tst gene among community- and hospital-acquired strains and isolates from Wegener’s Granulomatosis patients. FEMS Microbiol Lett 245(1):185–189. doi:10.1016/j.femsle.2005.03.002
Fraser J, Arcus V, Kong P, Baker E, Proft T (2000) Superantigens—powerful modifiers of the immune system. Mol Med Today 6(3):125–132. doi:10.1016/S1357-4310(99)01657-3
Llewelyn M, Cohen J (2002) Superantigens: microbial agents that corrupt immunity. Lancet Infect Dis 2(3):156–162. doi:10.1016/S1473-3099(02)00222-0
Lowy FD (1998) Staphylococcus aureus infections. N Engl J Med 339(8):520–532. doi:10.1056/NEJM199808203390806
Department of Health Australian Capital Territory (1983) Toxic shock syndrome (TSS) update. Commun Dis Intell 83(15):2–6
[No authors listed] (1995) Toxic shock syndrome. Qld Nurse 14(5):17.
Robinson P, Peel M, Skowronski G, Rouch G (1996) Toxic shock syndromes in Australia and New Zealand 1990–1994. Commun Dis Intell 20(15):336–339
Donovan JW (1984) Search for possible fatal cases of toxic shock syndrome.Med J Aust 141(10):646–647
Couper JJ, Kallincos N, Pollard A, Honeyman M, Prager P, Harrison LC, Rischmueller M (2000) Toxic shock syndrome associated with newly diagnosed type I diabetes. J Paediatr Child Health 36(3):279–282. doi:10.1046/j.1440-1754.2000.00475.x
Raper RF, Ibels LS (1982) Toxic-shock syndrome in a male complicated by oliguric acute renal failure. Aust NZ J Med 12(1):60–62
Goodman JS (1980) Toxic-shock syndrome and the Bundaberg disaster. N Engl J Med 303(24):1417
Scarff CE, Baker C, Hill P, Foley P (2002) Late-onset warfarin necrosis. Australas J Dermatol 43(3):202–206. doi:10.1046/j.1440-0960.2002.00596.x
MacIsaac CM, Page MA, Biggs BA, Visvanathan K (2005) Staphylococcal toxic shock syndrome: still a problem. Med J Aust 182(12):651–652
Ellington MJ, Ganner M, East C, Ganner MA, Warner M, Kearns AM (2007) Community-associated MRSA clone encoding toxic shock syndrome toxin 1 (TSST-1) in England. In: Proceedings of the 17th European Congress of Clinical Microbiology and Infectious Diseases, Munich, Germany, March/April 2007. Blackwell Publishing
Durand G, Bes M, Meugnier H, Enright MC, Forey F, Liassine N, Wenger A, Kikuchi K, Lina G, Vandenesch F, Etienne J (2006) Detection of new methicillin-resistant Staphylococcus aureus clones containing the toxic shock syndrome toxin 1 gene responsible for hospital- and community-acquired infections in France. J Clin Microbiol 44(3):847–853. doi:10.1128/JCM.44.3.847-853.2006
Kikuchi K (2003) Genetic basis of neonatal methicillin-resistant Staphylococcus aureus in Japan. Pediatr Int 45(2):223–229. doi:10.1046/j.1442-200X.2003.01720.x
Tristan A, Ferry T, Durand G, Dauwalder O, Bes M, Lina G, Vandenesch F, Etienne J (2007) Virulence determinants in community and hospital meticillin-resistant Staphylococcus aureus. J Hosp Infect 65(Suppl 2):105–109. doi:10.1016/S0195-6701(07)60025-5
Parsonnet J, Goering RV, Hansmann MA, Jones MB, Ohtagaki K, Davis CC, Totsuka K (2008) Prevalence of toxic shock syndrome toxin 1 (TSST-1)-producing strains of Staphylococcus aureus and antibody to TSST-1 among healthy Japanese women. J Clin Microbiol 46(8):2731–2738. doi:10.1128/JCM.00228-08
Musser JM, Schlievert PM, Chow AW, Ewan P, Kreiswirth BN, Rosdahl VT, Naidu AS, Witte W, Selander RK (1990) A single clone of Staphylococcus aureus causes the majority of cases of toxic shock syndrome. Proc Natl Acad Sci USA 87(1):225–229. doi:10.1073/pnas.87.1.225
Nimmo GR, Bell JM, Mitchell D, Gosbell IB, Pearman JW, Turnidge JD (2003) Antimicrobial resistance in Staphylococcus aureus in Australian teaching hospitals, 1989–1999. Microb Drug Resist 9(2):155–160. doi:10.1089/107662903765826741
Coombs GW, Nimmo GR, Bell JM, Huygens F, O’Brien FG, Malkowski MJ, Pearson JC, Stephens AJ, Giffard PM (2004) Genetic diversity among community methicillin-resistant Staphylococcus aureus strains causing outpatient infections in Australia. J Clin Microbiol 42(10):4735–4743. doi:10.1128/JCM.42.10.4735-4743.2004
Munckhof WJ, Nimmo GR, Carney J, Schooneveldt JM, Huygens F, Inman-Bamber J, Tong E, Morton A, Giffard P (2008) Methicillin-susceptible, non-multiresistant methicillin-resistant and multiresistant methicillin-resistant Staphylococcus aureus infections: a clinical, epidemiological and microbiological comparative study. Eur J Clin Microbiol Infect Dis 27(5):355–364. doi:10.1007/s10096-007-0449-3
Nimmo GR, Coombs GW, Pearson PC, O’Brien FG, Christiansen KJ, Turnidge JD, Gosbell IB, Collignon P, McLaws M-L (2006) MRSA in the Australian community: an evolving epidemic. Med J Aust 184:384–388
Nimmo GR, Pearson JC, Collignon PJ, Christiansen KJ, Coombs GW, Bell JM, McLaws M-L (2007) Prevalence of MRSA among Staphylococcus aureus isolated from hospital inpatients, 2005: report from the Australian Group for Antimicrobial Resistance. Commun Dis Intell 31:288–296
Stephens AJ, Huygens F, Inman-Bamber J, Price EP, Nimmo GR, Schooneveldt J, Munckhof W, Giffard PM (2006) Methicillin-resistant Staphylococcus aureus genotyping using a small set of polymorphisms. J Med Microbiol 55(Pt 1):43–51. doi:10.1099/jmm.0.46157-0
Barski P, Piechowicz L, Galiński J, Kur J (1996) Rapid assay for detection of methicillin-resistant Staphylococcus aureus using multiplex PCR. Mol Cell Probes 10(6):471–475. doi:10.1006/mcpr.1996.0066
Unal S, Hoskins J, Flokowitsch JE, Wu CY, Preston DA, Skatrud PL (1992) Detection of methicillin-resistant staphylococci by using the polymerase chain reaction. J Clin Microbiol 30(7):1685–1691
Huygens F, Inman-Bamber J, Nimmo GR, Munckhof W, Schooneveldt J, Harrison B, McMahon JA, Giffard PM (2006) Staphylococcus aureus genotyping using novel real-time PCR formats. J Clin Microbiol 44(10):3712–3719. doi:10.1128/JCM.00843-06
Becker K, Roth R, Peters G (1998) Rapid and specific detection of toxigenic Staphylococcus aureus: use of two multiplex PCR enzyme immunoassays for amplification and hybridization of staphylococcal enterotoxin genes, exfoliative toxin genes, and toxic shock syndrome toxin 1 gene. J Clin Microbiol 36(9):2548–2553
Feil EJ, Cooper JE, Grundmann H, Robinson DA, Enright MC, Berendt T, Peacock SJ, Smith JM, Murphy M, Spratt BG, Moore CE, Day NPJ (2003) How clonal is Staphylococcus aureus? J Bacteriol 185(11):3307–3316. doi:10.1128/JB.185.11.3307-3316.2003
Multi Locus Sequence Typing. Home page at: http://saureus.mlst.net/
Monecke S, Slickers P, Ehricht R (2008) Assignment of Staphylococcus aureus isolates to clonal complexes based on microarray analysis and pattern recognition. FEMS Immunol Med Microbiol 53(2):237–251. doi:10.1111/j.1574-695X.2008.00426.x
Munckhof WJ, Schooneveldt J, Coombs GW, Hoare J, Nimmo GR (2003) Emergence of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) infection in Queensland, Australia. Int J Infect Dis 7(4):259–264. doi:10.1016/S1201-9712(03)90104-4
Parsonnet J, Hansmann MA, Delaney ML, Modern PA, Dubois AM, Wieland-Alter W, Wissemann KW, Wild JE, Jones MB, Seymour JL, Onderdonk AB (2005) Prevalence of toxic shock syndrome toxin 1-producing Staphylococcus aureus and the presence of antibodies to this superantigen in menstruating women. J Clin Microbiol 43(9):4628–4634. doi:10.1128/JCM.43.9.4628-4634.2005
Nakano M, Miyazawa H, Kawano Y, Kawagishi M, Torii K, Hasegawa T, Iinuma Y, Ohta M (2002) An outbreak of neonatal toxic shock syndrome-like exanthematous disease (NTED) caused by methicillin-resistant Staphylococcus aureus (MRSA) in a neonatal intensive care unit. Microbiol Immunol 46(4):277–284
Tierno PM Jr (2005) Reemergence of staphylococcal toxic shock syndrome in the United States since 2000. J Clin Microbiol 43(4):2032; author reply 2032–2033. doi:10.1128/JCM.43.4.2032-2033.2005
Layer F, Ghebremedhin B, König W, König B (2006) Heterogeneity of methicillin-susceptible Staphylococcus aureus strains at a German University Hospital implicates the circulating-strain pool as a potential source of emerging methicillin-resistant S. aureus clones. J Clin Microbiol 44(6):2179–2185. doi:10.1128/JCM.02321-05
Acknowledgements
The project was undertaken at the Pathology Queensland Central Microbiology Laboratory. The authors acknowledge the Study, Education and Research Trust Fund (SERTF) for providing the funding for the project and the Pathology Queensland Princess Alexandra Hospital Microbiology Laboratory for providing the stored isolates.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schlebusch, S., Schooneveldt, J.M., Huygens, F. et al. Prevalence of Staphylococcus aureus strains in an Australian cohort, 1989–2003: evidence for the low prevalence of the toxic shock toxin and Panton–Valentine leukocidin genes. Eur J Clin Microbiol Infect Dis 28, 1183–1189 (2009). https://doi.org/10.1007/s10096-009-0761-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-009-0761-1