Abstract
Objectives
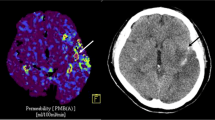
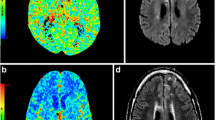
Blood-brain barrier (BBB) disruption is an important pathological change after cerebral infarction that exacerbates brain injury. We aimed to investigate and compare the predictive utility of pre-treatment BBB permeability (BBBP) and BBBP within 1 h after endovascular treatment (EVT) for hemorrhagic transformation (HT) and 90-day prognosis.
Methods
Patients underwent preoperative computed tomography perfusion (CTP) and non-contrast CT (NCCT) within 1 h after EVT. Preoperative BBBP was determined by the relative permeability surface area product (rPS) in the hypoperfusion area. Postoperative BBBP was determined by the post-EVT Alberta Stroke Program Early CT Score (Post-ASPECTS), which is based on brain parenchymal hyperdensity on the postoperative NCCT.
Outcomes
We included 100 patients. Univariate logistic regression analysis revealed correlations of preoperative rPS with HT, poor outcomes, and death. However, these correlations were not observed in multivariate logistic regression. A Post-ASPECTS ≤7 and could independently predict poor outcomes, while Post-ASPECTS ≤6 could independently predict death and HT. The baseline National Institutes of Health Stroke Scale (NIHSS) score could independently predict poor outcomes and death but not HT. A combined model using the baseline NIHSS and Post-ASPECTS scores had better predictive performance for poor outcomes and death than baseline NIHSS score alone; however, it was not superior to the predictive performance of the Post-ASPECTS score.
Conclusion
The preoperative rPS cannot independently predict clinical outcomes in EVT-treated patients; contrastingly, the Post-ASPECTS score could independently predict poor outcomes, death, and HT. This parameter could inform prompt postoperative treatment decisions.

Similar content being viewed by others
References
Neuberger U et al (2019) Risk factors of intracranial hemorrhage after mechanical thrombectomy of anterior circulation ischemic stroke. Neuroradiology 61:461–469. https://doi.org/10.1007/s00234-019-02180-6
Powers WJ et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the american heart association/american stroke association. Stroke 50:e344–e418. https://doi.org/10.1161/str.0000000000000211
Jiang X et al (2018) Blood-brain barrier dysfunction and recovery after ischemic stroke. Prog Neurobiol 163–164:144–171. https://doi.org/10.1016/j.pneurobio.2017.10.001
Chen L et al (2022) Post-aspects based on hyperdensity in ncct immediately after thrombectomy is an ultra-early predictor of hemorrhagic transformation and prognosis. Front Neurol 13:887277. https://doi.org/10.3389/fneur.2022.887277
Kassner A, Merali Z (2015) Assessment of blood-brain barrier disruption in stroke. Stroke 46:3310–3315. https://doi.org/10.1161/strokeaha.115.008861
Liu C et al (2018) Increased blood-brain barrier permeability in contralateral hemisphere predicts worse outcome in acute ischemic stroke after reperfusion therapy. J Neurointerv Surg 10:937–941. https://doi.org/10.1136/neurintsurg-2017-013663
Merali Z et al (2017) Evolution of blood-brain-barrier permeability after acute ischemic stroke. PLoS One 12:e0171558. https://doi.org/10.1371/journal.pone.0171558
Ng FC et al (2022) Reduced severity of tissue injury within the infarct may partially mediate the benefit of reperfusion in ischemic stroke. Stroke 53:1915–1923. https://doi.org/10.1161/strokeaha.121.036670
Wu L et al (2023) Mri arterial spin labeling in evaluating hemorrhagic transformation following endovascular recanalization of subacute ischemic stroke. Front Neurosci 17:1105816. https://doi.org/10.3389/fnins.2023.1105816
Leigh R et al (2014) Pretreatment blood-brain barrier damage and post-treatment intracranial hemorrhage in patients receiving intravenous tissue-type plasminogen activator. Stroke 45:2030–2035. https://doi.org/10.1161/strokeaha.114.005249
Li X et al (2020) The value of whole-brain perfusion parameters combined with multiphase computed tomography angiography in predicting hemorrhagic transformation in ischemic stroke. J Stroke Cerebrovasc Dis 29:104690. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104690
Liu C et al (2018) Severe blood-brain barrier disruption in cardioembolic stroke. Front Neurol 9:55. https://doi.org/10.3389/fneur.2018.00055
Liu N et al (2017) Ct permeability imaging predicts clinical outcomes in acute ischemic stroke patients treated with intra-arterial thrombolytic therapy. Mol Neurobiol 54:2539–2546. https://doi.org/10.1007/s12035-016-9838-x
Xu J et al (2023) Predictive value of ct perfusion in hemorrhagic transformation after acute ischemic stroke: A systematic review and meta-analysis. Brain Sci 13. https://doi.org/10.3390/brainsci13010156
Chen Z et al (2020) Contrast extravasation is predictive of poor clinical outcomes in patients undergoing endovascular therapy for acute ischemic stroke in the anterior circulation. J Stroke Cerebrovasc Dis 29:104494. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104494
Desilles JP et al (2013) Blood-brain barrier disruption is associated with increased mortality after endovascular therapy. Neurology 80:844–851. https://doi.org/10.1212/WNL.0b013e31828406de
Khatri R et al (2012) Blood-brain barrier, reperfusion injury, and hemorrhagic transformation in acute ischemic stroke. Neurology 79:S52–S57. https://doi.org/10.1212/WNL.0b013e3182697e70
Renú A et al (2015) Relevance of blood-brain barrier disruption after endovascular treatment of ischemic stroke: Dual-energy computed tomographic study. Stroke 46:673–679. https://doi.org/10.1161/strokeaha.114.008147
Wang T et al (2023) Hemorrhagic transformation assessment based on dual energy ct of immediately and twenty-four hours after endovascular thrombectomy for acute ischemic stroke. Diagnostics (Basel) 13. https://doi.org/10.3390/diagnostics13152493
Dankbaar JW et al (2009) Age- and anatomy-related values of blood-brain barrier permeability measured by perfusion-ct in non-stroke patients. J Neuroradiol 36:219–227. https://doi.org/10.1016/j.neurad.2009.01.001
Horsch AD et al (2016) Relation between stroke severity, patient characteristics and ct-perfusion derived blood-brain barrier permeability measurements in acute ischemic stroke. Clin Neuroradiol 26:415–421. https://doi.org/10.1007/s00062-015-0375-1
Cabral FB et al (2017) Hyper-attenuating brain lesions on ct after ischemic stroke and thrombectomy are associated with final brain infarction. Interv Neuroradiol 23:594–600. https://doi.org/10.1177/1591019917729550
Leigh R et al (2016) Pretreatment blood-brain barrier disruption and post-endovascular intracranial hemorrhage. Neurology 87:263–269. https://doi.org/10.1212/wnl.0000000000002862
Shi ZS et al (2018) Early blood-brain barrier disruption after mechanical thrombectomy in acute ischemic stroke. J Neuroimaging 28:283–288. https://doi.org/10.1111/jon.12504
Ma C et al (2022) Quantitative intracerebral iodine extravasation in risk stratification for intracranial hemorrhage in patients with acute ischemic stroke. AJNR Am J Neuroradiol 43:1589–1596. https://doi.org/10.3174/ajnr.A7671
Yang F et al (2023) Prognostic value of contrast staining on dual-energy ct after endovascular therapy in acute ischemic stroke: A meta-analysis. BMC Neurol 23:326. https://doi.org/10.1186/s12883-023-03370-9
Sandoval KE, Witt KA (2008) Blood-brain barrier tight junction permeability and ischemic stroke. Neurobiol Dis 32:200–219. https://doi.org/10.1016/j.nbd.2008.08.005
Kuroiwa T et al (1985) The biphasic opening of the blood-brain barrier to proteins following temporary middle cerebral artery occlusion. Acta Neuropathol 68:122–129. https://doi.org/10.1007/bf00688633
Broocks G et al (2021) Relationship between the degree of recanalization and functional outcome in acute ischemic stroke is mediated by penumbra salvage volume. J Neurol 268:2213–2222. https://doi.org/10.1007/s00415-021-10410-2
Wang DT et al (2015) Successful recanalization post endovascular therapy is associated with a decreased risk of intracranial haemorrhage: A retrospective study. BMC Neurol 15:185. https://doi.org/10.1186/s12883-015-0442-x
Guo X et al (2023) Ischemia reperfusion injury induced blood brain barrier dysfunction and the involved molecular mechanism. Neurochem Res 48:2320–2334. https://doi.org/10.1007/s11064-023-03923-x
Liu C et al (2018) Reperfusion facilitates reversible disruption of the human blood-brain barrier following acute ischaemic stroke. Eur Radiol 28:642–649. https://doi.org/10.1007/s00330-017-5025-3
Luo H et al (2023) Neutrophil extracellular traps in cerebral ischemia/reperfusion injury: Friend and foe. Curr Neuropharmacol 21:2079–2096. https://doi.org/10.2174/1570159x21666230308090351
Shi Y et al (2016) Rapid endothelial cytoskeletal reorganization enables early blood-brain barrier disruption and long-term ischaemic reperfusion brain injury. Nat Commun 7:10523. https://doi.org/10.1038/ncomms10523
Simpkins AN et al (2016) Identification of reversible disruption of the human blood-brain barrier following acute ischemia. Stroke 47:2405–2408. https://doi.org/10.1161/strokeaha.116.013805
Zhou Y et al (2023) Reperfusion injury is associated with poor outcome in patients with recanalization after thrombectomy. Stroke 54:96–104. https://doi.org/10.1161/strokeaha.122.039337
Menon BK et al (2018) Association of clinical, imaging, and thrombus characteristics with recanalization of visible intracranial occlusion in patients with acute ischemic stroke. Jama 320:1017–1026. https://doi.org/10.1001/jama.2018.12498
Honig A et al (2022) Predictors and prognostic implications of hemorrhagic transformation following cerebral endovascular thrombectomy in acute ischemic stroke: A multicenter analysis. Cardiovasc Intervent Radiol 45:826–833. https://doi.org/10.1007/s00270-022-03115-0
Kwon H et al (2022) Etiology-related outcome of endovascular therapy in posterior circulation stroke compared to anterior circulation stroke. J Stroke 24:245–255. https://doi.org/10.5853/jos.2022.01095
Lee YB et al (2019) Predictors and impact of hemorrhagic transformations after endovascular thrombectomy in patients with acute large vessel occlusions. J Neurointerv Surg 11:469–473. https://doi.org/10.1136/neurintsurg-2018-014080
Sun D et al (2022) Predictors of symptomatic intracranial hemorrhage after endovascular treatment for acute large vessel occlusion: Data from angel-act registry. J Thromb Thrombolysis 54:558–565. https://doi.org/10.1007/s11239-022-02688-4
Funding
This work was supported by the National Natural Science Foundation of China (81870918), the Research Fund Project of Anhui Medical University (2022xkj142), and the Key Project of the Research Foundation of Anhui Institute of Translational Medicine (No.2023zhyx-B04).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval and Informed consent
Ethical approval for the study was obtained from the First Affiliated Hospital of Anhui Medical University(reference number: Quick-PJ 2023-14-56).
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhai, H., Li, Y., Jia, R. et al. Post-endovascular treatment, blood-brain barrier disruption, predicts patient outcomes better than pre-treatment status. Neurol Sci (2024). https://doi.org/10.1007/s10072-024-07468-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10072-024-07468-x