Abstract
Background
Neurological outcome after endovascular treatment (EVT) of acute ischemic stroke (AIS) may depend on both patient-specific and procedural factors. We hypothesized that altered systemic homeostasis might be frequent and affect outcome in these patients. The aim of this study was to analyze secondary insults during EVT of AIS and its association with outcome and anesthesiologic regimen.
Methods
This was a single-center prospective observational study on patients undergoing EVT for AIS under local anesthesia (LA), conscious sedation (CS), or general anesthesia (GA). Altered systemic parameters were recorded and quantified as secondary insults. The primary endpoint was to evaluate number, duration, and severity of secondary insults during EVT. Secondary endpoints were to analyze association of insults with modified Rankin Scale at 90 days and anesthesiologic regimen.
Results and conclusions
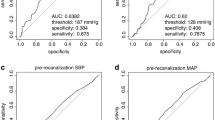
One hundred twenty patients were enrolled. Overall, 78% of patients experienced at least one episode of hypotension, 21% hypertension, 54% hypoxemia, 16% bradycardia, and 13% tachycardia. In patients monitored with capnometry, 70% experienced hypocapnia and 21% hypercapnia. LA was selected in 24 patients, CS in 84, and GA in 12. Hypotension insult was more frequent during GA than LA and CS (p = 0.0307), but intraprocedural blood pressure variation was higher during CS (p = 0.0357). Hypoxemia was more frequent during CS (p = 0.0087). Proportion of hypotension duration was higher in unfavorable outcome but secondary insults did not remain in the final model of multivariable analysis. Secondary insults occurred frequently during EVT for AIS but the main predictors of outcome were age, NIHSS at admission, and prompt and successful recanalization.

Similar content being viewed by others
Data Availability
All relevant data are within the paper.
References
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL et al (2015) 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment. Stroke 46:3020–3035. https://doi.org/10.1161/STR.0000000000000074
Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, Guillemin F (2016) Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke ( THRACE ): a randomised controlled trial. Lancet Neurol 15:1138–1147. https://doi.org/10.1016/S1474-4422(16)30177-6
Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387:1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
Rabinstein AA, Albers GW, Brinjikji W, Koch S (2019) Factors that may contribute to poor outcome despite good reperfusion after acute endovascular stroke therapy. Int J Stroke 14:23–31
Jones PA, Andrews PJ, Midgley S, Anderson SI, Piper IR et al (1994) Measuring the burden of secondary insults in head-injured patients during intensive care. J Neurosurg Anesthesiol 6:4–14
Mazzeo AT, Filippini C, Rosato R, Fanelli V, Assenzio B et al (2016) Multivariate projection method to investigate inflammation associated with secondary insults and outcome after human traumatic brain injury: a pilot study. J Neuroinflammation 13:1–15. https://doi.org/10.1186/s12974-016-0624-5
Brinjikji W, Murad MH, Rabinstein AA, Cloft HJ, Lanzino G, Kallmes DF (2015) Conscious sedation versus general anesthesia during endovascular acute ischemic stroke treatment: a systematic review and meta-analysis. Am J Neuroradiol 36:525–529. https://doi.org/10.3174/ajnr.A4159
Brinjikji W, Pasternak J, Murad MH, Cloft HJ, Welch TL, Kallmes DF, Rabinstein AA (2017) Anesthesia-related outcomes for endovascular stroke revascularization: a systematic review and meta-analysis. Stroke 48:2784–2791. https://doi.org/10.1161/STROKEAHA.117.017786
Ilyas A, Chen CJ, Ding D, Foreman PM, Buell TJ et al (2018) Endovascular mechanical thrombectomy for acute ischemic stroke under general anesthesia versus conscious sedation: a systematic review and meta-analysis. World Neurosurg 112:e355–e367. https://doi.org/10.1016/j.wneu.2018.01.049
Campbell BCV, van Zwam WH, Goyal M, Menon BK, Dippel DWJ et al (2018) Effect of general anaesthesia on functional outcome in patients with anterior circulation ischaemic stroke having endovascular thrombectomy versus standard care: a meta-analysis of individual patient data. Lancet Neurol 17:47–53. https://doi.org/10.1016/S1474-4422(17)30407-6
Goyal N, Malhotra K, Ishfaq MF, Tsivgoulis G, Nickele C, Hoit D, Arthur AS, Alexandrov AV, Elijovich L (2019) Current evidence for anesthesia management during endovascular stroke therapy: updated systematic review and meta-analysis. J Neurointerv Surg 11:107–113. https://doi.org/10.1136/neurintsurg-2018-013916
Schönenberger S, Uhlmann L, Hacke W, Schieber S, Mundiyanapurath S et al (2016) Effect of conscious sedation vs general anesthesia on early neurological improvement among patients with ischemic stroke undergoing endovascular thrombectomy. JAMA 316:1986. https://doi.org/10.1001/jama.2016.16623
Hendén LP, Rentzos A, Karlsson J-E, Rosengren L, Leiram B et al (2017) General anesthesia versus conscious sedation for endovascular treatment of acute ischemic stroke. Stroke 48:1601–1607. https://doi.org/10.1161/STROKEAHA.117.016554
Simonsen CZ, Yoo AJ, Sørensen LH, Juul N, Johnsen SP, Andersen G, Rasmussen M (2018) Effect of general anesthesia and conscious sedation during endovascular therapy on infarct growth and clinical outcomes in acute ischemic stroke. JAMA Neurol 75:470. https://doi.org/10.1001/jamaneurol.2017.4474
Sun J, Liang F, Wu Y, Zhao Y, Miao Z et al (2018) Choice of ANesthesia for EndoVAScular Treatment of Acute Ischemic Stroke (CANVAS): results of the CANVAS pilot randomized controlled trial. J Neurosurg Anesthesiol 00:1–7. https://doi.org/10.1097/ANA.0000000000000567
Campbell D, Diprose WK, Deng C, Barber PA (2019) General anesthesia versus conscious sedation in endovascular thrombectomy for stroke : a meta-analysis of 4 randomized controlled trials. J Neurosurg Anesthesiol 00:1–7. https://doi.org/10.1097/ANA.0000000000000646
Gensini G, Carolei A, Ricci S, Mazzoli T, Padiglioni C, Patoia L, Quaglini S, Reboldi G (2016) SPREAD – stroke prevention and educational awareness diffusion VIII EDIZIONE - Ictus cerebrale: Linee guida italiane di prevenzione e trattamento. Raccomandazioni e Sintesi. 1–296
Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, Von Kummer R et al (2013) Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 44:2650–2663. https://doi.org/10.1161/STROKEAHA.113.001972
Petersen NH, Ortega-Gutierrez S, Wang A, Lopez GV, Strander S et al (2019) Decreases in blood pressure during thrombectomy are associated with larger infarct volumes and worse functional outcome. Stroke 50:1797–1804. https://doi.org/10.1161/STROKEAHA.118.024286
Fandler-Höfler S, Heschl S, Argüelles-Delgado P, Kneihsl M, Hassler E et al (2020) Single mean arterial blood pressure drops during stroke thrombectomy under general anaesthesia are associated with poor outcome. J Neurol 267:1331–1339. https://doi.org/10.1007/s00415-020-09701-x
Rasmussen M, Espelund US, Juul N, Yoo AJ, Sørensen LH, Sørensen KE, Johnsen SP, Andersen G, Simonsen CZ (2018) The influence of blood pressure management on neurological outcome in endovascular therapy for acute ischaemic stroke. Br J Anaesth 120:1287–1294. https://doi.org/10.1016/j.bja.2018.01.039
Chen M, Kronsteiner D, Pfaff J, Schieber S, Jäger L et al (2021) Hemodynamic status during endovascular stroke treatment: association of blood pressure with functional outcome. Neurocrit Care. https://doi.org/10.1007/s12028-021-01229-w
Meyer L, Stracke CP, Jungi N, Wallocha M, Broocks G et al (2021) Thrombectomy for primary distal posterior cerebral artery occlusion stroke: the TOPMOST study. JAMA Neurol 78:434–444. https://doi.org/10.1001/jamaneurol.2021.0001
Langezaal LCM, van der Hoeven EJRJ, Mont’ Alverne FJA, de Carvalho JJF, Lima FO et al (2021) Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med 384:1910–1920
Funding
This work was supported by (grant no. S1618_L2_MAZA_01 from Compagnia San Paolo, Torino).
Author information
Authors and Affiliations
Contributions
ATM: study conception and design, analysis and interpretation of data, and writing the paper. SCB, SM, and GC: patient recruitment, data collection, and analysis and interpretation of data. CF: conception and design, statistical analysis, and interpretation of data; AN, PC, and MB: data collection, analysis and interpretation of data, and revising the manuscript critically for important intellectual content; LM: study design, analysis and interpretation of data, and revising the article critically for important intellectual content. VFT revising the article critically for important intellectual content. ATM, SCB, SM GC, CF, VFT, AN, PC, MB, and LM: final approval of the version to be published and agreement to be accountable for all aspects of the work thereby ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
Ethical Committee of the AOU Città della Salute e della Scienza of Turin (Italy) approved (CS2/905).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mazzeo, A.T., Cappio Borlino, S., Malerba, S. et al. Occurrence of secondary insults during endovascular treatment of acute ischemic stroke and impact on outcome: the SIR-STROKE prospective observational study. Neurol Sci 44, 2061–2069 (2023). https://doi.org/10.1007/s10072-023-06599-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-06599-x