Abstract
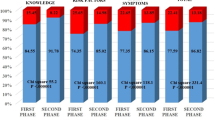
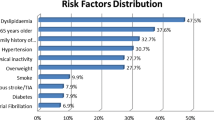
Timely access to medical assistance is the first crucial step to improving clinical outcomes of stroke patients. Many educational campaigns have been organized with the purpose of making people aware of what a stroke is and what is necessary to do after its clinical onset. The PRESTO campaign was organized in Genoa (Italy) to spread easy messages regarding the management of the acute phase of stroke. Educational material was disseminated to educate people to call the emergency medical services as soon as symptoms appear. Data collected were analyzed in three different phases of the campaign: before the beginning, during, and after the end. We enrolled 1,132 patients with ischemic stroke admitted to hospital within 24 hours of symptoms onset. Our data showed a mild reduction in onset-to-door time (24 minutes) during the months following the end of the campaign and a slight increase in number of patients who arrived at hospitals, in particular with milder symptoms and transient ischemic attack, as opposed to the same period before the campaign. Interestingly, in the months after the end of the campaign, we observed a slight reduction of the percentage of patients who accessed hospitals after 4.5 hours from symptoms onset. In conclusion, our results may suggest that an informative campaign can be successful in making people rapidly aware of stroke onset, with the consequent rapid access to hospitals. Considering the changing of way of access to information, we think that an extensive multimedia campaign should be evaluated in the next future.


Similar content being viewed by others
References
Johnson CO, Nguyen M, Roth GA et al (2019) Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurology 18:439–458. https://doi.org/10.1016/S1474-4422(19)30034-1
The GBD (2016) Lifetime Risk of Stroke Collaborators (2018) Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med 379:2429–2437. https://doi.org/10.1056/NEJMoa1804492
Campbell BCV, De Silva DA, Macleod MR et al (2019) Ischaemic stroke. Nat Rev Dis Primers 5:70. https://doi.org/10.1038/s41572-019-0118-8
Wardlaw JM, Murray V, Berge E, del Zoppo GJ (2014) Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000213.pub3
Wahlgren N, Ahmed N, Dávalos A et al (2007) Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. The Lancet 369:275–282. https://doi.org/10.1016/S0140-6736(07)60149-4
Hacke W, Kaste M, Bluhmki E et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359:1317–1329. https://doi.org/10.1056/NEJMoa0804656
Centers for Disease Control and Prevention (CDC) (2007) Prehospital and hospital delays after stroke onset—United States, 2005–2006. MMWR Morb Mortal Wkly Rep 56:474–478
Powers WJ, Rabinstein AA, Ackerson T et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke50:e344–e418. https://doi.org/10.1161/STR.0000000000000211
InformMe — clinical guidelines for stroke management. https://informme.org.au/en/Guidelines/Clinical-Guidelines-for-Stroke-Management
Ictus Cerebrale: linee guida italiane di prevenzione e trattamento. SPREAD VIII edizione 2016. https://www.iso-stroke.it/wp-content/uploads/2017/02/LIBRO-SPREAD-VIII-ED-13-09-16.pdf
Nogueira RG, Jadhav AP, Haussen DC et al (2017) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378:11–21. https://doi.org/10.1056/NEJMoa1706442
Moser DK, Kimble LP, Alberts MJ et al (2006) Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke. Circulation 114:168–182. https://doi.org/10.1161/CIRCULATIONAHA.106.176040
Walker G, Yip S, Zhelev Z, Henschke N (2014) Prehospital stroke scales as screening tools for early identification of stroke and transient ischemic attack. Cochrane Database Syst Rev 4(4):CD011427. https://doi.org/10.1002/14651858.CD011427
De Luca A, Mariani M, Riccardi MT, Damiani G (2019) The role of the Cincinnati Prehospital Stroke Scale in the emergency department: evidence from a systematic review and meta-analysis. Open Access Emerg Med. https://doi.org/10.2147/OAEM.S178544
Kothari R, Hall K, Brott T, Broderick J (1997) Early stroke recognition: developing an out-of-hospital NIH Stroke Scale. Acad Emerg Med 4:986–990. https://doi.org/10.1111/j.1553-2712.1997.tb03665.x
Joseph H, Omar H, Damian J et al (2003) Diagnostic accuracy of stroke referrals from primary care, emergency room physicians, and ambulance staff using the face arm speech test. Stroke 34:71–76. https://doi.org/10.1161/01.STR.0000044170.46643.5E
Lima FO, Silva GS, Furie KL et al (2016) The field assessment stroke triage for emergency destination (FAST-ED): a simple and accurate pre-hospital scale to detect large vessel occlusion strokes. Stroke 47:1997–2002. https://doi.org/10.1161/STROKEAHA.116.013301
de la Ossa P, Natalia CD, Montse G et al (2014) Design and validation of a prehospital stroke scale to predict large arterial occlusion. Stroke 45:87–91. https://doi.org/10.1161/STROKEAHA.113.003071
Kidwell CS, Saver JL, Schubert GB et al (1998) Design and retrospective analysis of the Los Angeles Prehospital Stroke Screen (LAPSS). Prehosp Emerg Care 2:267–273. https://doi.org/10.1080/10903129808958878
Rosamond W, Flegal K, Furie K et al (2008) Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 117:e25-146. https://doi.org/10.1161/CIRCULATIONAHA.107.187998
Kwan J, Hand P, Sandercock P (2004) Improving the efficiency of delivery of thrombolysis for acute stroke: a systematic review. QJM 97:273–279. https://doi.org/10.1093/qjmed/hch054
Clark JM, Renier SA (2001) A community stroke study: factors influencing stroke awareness and hospital arrival time. J Stroke Cerebrovasc Dis 10:274–278. https://doi.org/10.1053/jscd.2001.123774
Agyeman O, Nedeltchev K, Arnold M et al (2006) Time to admission in acute ischemic stroke and transient ischemic attack. Stroke 37:963–966. https://doi.org/10.1161/01.STR.0000206546.76860.6b
Rossnagel K, Jungehülsing GJ, Nolte CH et al (2004) Out-of-hospital delays in patients with acute stroke. Ann Emerg Med 44:476–483. https://doi.org/10.1016/j.annemergmed.2004.06.019
Brandler ES, Sharma M, Sinert RH, Levine SR (2014) Prehospital stroke scales in urban environments. Neurology 82:2241–2249. https://doi.org/10.1212/WNL.0000000000000523
Kobayashi A, Czlonkowska A, Ford GA et al (2018) European Academy of Neurology and European Stroke Organization consensus statement and practical guidance for pre-hospital management of stroke. Eur J Neurol 25:425–433. https://doi.org/10.1111/ene.13539
Statistiche demografiche ISTAT. http://demo.istat.it/pop2019/index1.html. Accessed 20 Oct 2019
Hage V (2011) The NIH stroke scale: a window into neurological status. Nurs Spectr 24:44–49
Rioux B, Brissette V, Marin FF, et al (2021) The impact of stroke public awareness campaigns differs between sociodemographic groups. Can J Neurol Sci 1–8. https://doi.org/10.1017/cjn.2021.76
Fladt J, Meier N, Thilemann S et al (2019) Reasons for prehospital delay in acute ischemic stroke. J Am Heart Assoc 8:e013101. https://doi.org/10.1161/JAHA.119.013101
Pulvers JN, Watson JDG (2017) If time is brain where is the improvement in prehospital time after stroke? Front Neurol 8:617. https://doi.org/10.3389/fneur.2017.00617
Denti L, Caminiti C, Scoditti U et al (2017) Impact on prehospital delay of a stroke preparedness campaign. Stroke 48:3316–3322. https://doi.org/10.1161/STROKEAHA.117.018135
Müller-Nordhorn J (2009) Population-based intervention to reduce prehospital delays in patients with cerebrovascular events. Arch Intern Med 169:1484. https://doi.org/10.1001/archinternmed.2009.232
More than a fifth of the EU population are aged 65 or over. https://ec.europa.eu/eurostat/web/products-eurostat-news/-/ddn-20210316-1. Accessed 18 Sept 2021
Hodgson C, Lindsay P, Rubini F (2007) Can mass media influence emergency department visits for stroke? Stroke 38:2115–2122. https://doi.org/10.1161/STROKEAHA.107.484071
Gandolfo C, Alberti F, Del Sette M et al (2020) Results of an educational campaign on stroke awareness in the 2032 Rotary District in Northern-Western Italy. Neurol Sci 41:411–416. https://doi.org/10.1007/s10072-019-04126-5
Funding
The PRESTO campaign was financially supported by Fondazione Cassa di Risparmio di Genova ed Imperia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
None.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gandoglia, I., Schirinzi, E., Hamedani, M. et al. The PRESTO study: awareness of stroke symptoms and time from onset to intervention. Neurol Sci 44, 229–236 (2023). https://doi.org/10.1007/s10072-022-06399-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06399-9