Abstract
Background
Chronic migraine (CM) is one of the most disabling neurological diseases, often associated to medication overuse headache (MOH). These patients make high use of pharmacological and non-pharmacological treatments, and experience high work-related indirect costs. The aim of this study was to address and compare the main driver of cost associated to CM-MOH and EM, and to evaluate the effect of improvement in migraine profile on disease cost.
Methods
We selected patients with baseline CM-MOH who reverted to an episodic pattern by 3 months after structured withdrawal. Paired sample t-test was used to explore the variation in headache frequency and its costs. Regression models were run to address the impact of single cost categories on total migraine cost.
Results
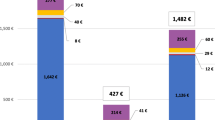
A total of 261 patients were included. Significant reductions in headache frequency and its costs were observed, with the exception of medical prophylaxis cost. The cost of migraine from chronic to episodic pattern is reduced by 533€ per month and 80% of this reduction is accountable to reduced indirect costs, i.e., loss of productive time.
Conclusions
The results of our study open to future considerations on future approaches to the treatment of CM-MOH in which new migraine-specific treatments, i.e., monoclonal antibodies, should be combined with other pharmacological and non-pharmacological ones.
Similar content being viewed by others
References
Raggi A, Monasta L, Beghi E, Caso V, Castelpietra G, Mondello S, Giussani G, Logroscino G, Magnani FG, Piccininni M, Pupillo E, Ricci S, Ronfani L, Santalucia P, Sattin D, Schiavolin S, Toppo C, Traini E, Steinmetz J, Nichols E, Ma R, Vos T, Feigin V, Leonardi M (2022) Incidence, prevalence and disability associated with neurological disorders in Italy between 1990 and 2019: an analysis based on the Global Burden of Disease Study 2019. J Neurol 269(4):2080–2098. https://doi.org/10.1007/s00415-021-10774-5
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders, 3rd edition. Cephalalgia 38(1):1–211. https://doi.org/10.1177/0333102417738202
VanderPluym JH, Halker Singh RB, Urtecho M, Morrow AS, Nayfeh T, Torres Roldan VD, Farah MH, Hasan B, Saadi S, Shah S, Abd-Rabu R, Daraz L, Prokop LJ, Murad MH, Wang Z (2021) Acute treatments for episodic migraine in adults: a systematic review and meta-analysis. JAMA 325(23):2357–2369. https://doi.org/10.1001/jama.2021.7939
Tepper SJ (2019) Acute treatment of migraine. Neurol Clin 37(4):727–742. https://doi.org/10.1016/j.ncl.2019.07.006
May A, Schulte LH (2016) Chronic migraine: risk factors, mechanisms and treatment. Nat Rev Neurol 12(8):455–464. https://doi.org/10.1038/nrneurol.2016.93
Sarchielli P, Granella F, Prudenzano MP, Pini LA, Guidetti V, Bono G, Pinessi L, Alessandri M, Antonaci F, Fanciullacci M, Ferrari A, Guazzelli M, Nappi G, Sances G, Sandrini G, Savi L, Tassorelli C, Zanchin G (2012) Italian guidelines for primary headaches: 2012 revised version. J Headache Pain 13(Suppl 2):S31–S70. https://doi.org/10.1007/s10194-012-0437-6
Agostoni EC, Barbanti P, Calabresi P, Colombo B, Cortelli P, Frediani F, Geppetti P, Grazzi L, Leone M, Martelletti P, Pini LA, Prudenzano MP, Sarchielli P, Tedeschi G, Russo A (2019) Italian chronic migraine group. Current and emerging evidence-based treatment options in chronic migraine: a narrative review. J Headache Pain 20(1):92. https://doi.org/10.1186/s10194-019-1038-4
Grazzi L, Toppo C, D’Amico D, Leonardi M, Martelletti P, Raggi A, Guastafierro E (2021) Non-pharmacological approaches to headaches: non-invasive neuromodulation, nutraceuticals, and behavioral approaches. Int J Environ Res Public Health 18(4):1503. https://doi.org/10.3390/ijerph18041503
Linde M, Gustavsson A, Stovner LJ, Steiner TJ, Barré J, Katsarava Z, Lainez JM, Lampl C, Lantéri-Minet M, Rastenyte D, Ruiz de la Torre E, Tassorelli C, Andrée C (2012) The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol 19:703–711. https://doi.org/10.1111/j.1468-1331.2011.03612.x
Raggi A, Leonardi M, Sansone E, Curone M, Grazzi L, D’Amico D (2020) The cost and the value of treatment of medication overuse headache in Italy: a longitudinal study based on patient-derived data. Eur J Neurol 27(1):62-e1. https://doi.org/10.1111/ene.14034
Sansone E, Grazzi L, Raggi A, Leonardi M, D’Amico D (2020) Mindfulness as an add-on treatment for patients with chronic migraine and medication overuse: a preliminary analysis. Neurol Sci 41(Suppl 2):469–471. https://doi.org/10.1007/s10072-020-04662-5
Raggi A, Giovannetti AM, Leonardi M, Sansone E, Schiavolin S, Curone M, Grazzi L, Usai S, D’Amico D (2017) Predictors of 12-months relapse after withdrawal treatment in hospitalized patients with chronic migraine associated with medication overuse: a longitudinal observational study. Headache 57(1):60–70. https://doi.org/10.1111/head.12979
Evers S, Jensen R, Federation E, of Neurological Societies, (2011) Treatment of medication overuse headache–guideline of the EFNS headache panel. Eur J Neurol 18(9):1115–21. https://doi.org/10.1111/j.1468-1331.2011.03497.x
Lipton RB, Buse DC, Dodick DW, Schwedt TJ, Singh P, Munjal S, Fanning K, Bostic Bs R, Reed ML (2021) Burden of increasing opioid use in the treatment of migraine: results from the Migraine in America Symptoms and Treatment Study. Headache 61(1):103–116. https://doi.org/10.1111/head.14018
Lipton RB, Buse DC, Friedman BW, Feder L, Adams AM, Fanning KM, Reed ML, Schwedt TJ (2020) Characterizing opioid use in a US population with migraine: results from the CaMEO study. Neurology 95(5):e457–e468. https://doi.org/10.1212/WNL.0000000000009324
Kangethe A, Polson M, Evangelatos TM, Speicher LC, Tenaglia AT, Staats PS, Liebler EJ, Mwamburi M (2020) Real-world assessment of concomitant opioid utilization and associated trends in patients with migraine. Am J Manag Care. 26(1 Suppl):S8–S14. https://doi.org/10.37765/ajmc.2020.42544
Bonafede M, Wilson K, Xue F (2019) Long-term treatment patterns of prophylactic and acute migraine medications and incidence of opioid-related adverse events in patients with migraine. Cephalalgia 39(9):1086–1098. https://doi.org/10.1177/0333102419835465
Levin M (2014) Opioids in headache. Headache 54(1):12–21. https://doi.org/10.1111/head.12266
Morasco BJ, Yarborough BJ, Smith NX, Dobscha SK, Deyo RA, Perrin NA, Green CA (2017) Higher prescription opioid dose is associated with worse patient-reported pain outcomes and more health care utilization. J Painv 18(4):437–445. https://doi.org/10.1016/j.jpain.2016.12.004
Jiang W, Li Z, Wei N, Chang W, Chen W, Sui HJ (2019) Effectiveness of physical therapy on the suboccipital area of patients with tension-type headache: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 98(19):e15487. https://doi.org/10.1097/MD.0000000000015487
Racicki S, Gerwin S, Diclaudio S, Reinmann S, Donaldson M (2013) Conservative physical therapy management for the treatment of cervicogenic headache: a systematic review. J Man Manip Ther 21(2):113–24. https://doi.org/10.1179/2042618612Y.0000000025
Van der Meer HA, Calixtre LB, Engelbert RHH, Visscher CM, Nijhuis-van der Sanden MW, Speksnijder CM (2020) Effects of physical therapy for temporomandibular disorders on headache pain intensity: a systematic review. Musculoskelet Sci Pract 50:102277. https://doi.org/10.1016/j.msksp.2020.102277
Blumenfeld A, Schim J, Brower J (2010) Pure tension-type headache versus tension-type headache in the migraineur. Curr Pain Headache Rep 14:465–469. https://doi.org/10.1007/s11916-010-0147-1
Olesen J, Burstein R, Ashina M, Tfelt-Hansen P (2009) Origin of pain in migraine: evidence for peripheral sensitisation. Lancet Neurol 8:679–690. https://doi.org/10.1016/S1474-4422(09)70090-0
May A, Schulte LH (2016) Chronic migraine: risk factors, mechanisms and treatment. Nat Rev Neurol 12:455–464. https://doi.org/10.1038/nrneurol.2016.93
Federfarma. https://www.federfarma.it/Farmaci-e-farmacie/Cerca-un-farmaco.aspx (Accessed 17/02/2022)
AIFA (Italian Drugs Agency). https://www.aifa.gov.it/en/-/modifica-registri-aimovig-ajovy-ed-emgality-emicrania- (Accessed 17/02/2022)
Barbanti P, Aurilia C, Egeo G, Fofi L, Cevoli S, Colombo B, Filippi M, Frediani F, Bono F, Grazzi L, Salerno A, Mercuri B, Carnevale A, Altamura C, Vernieri F (2021) Erenumab in the prevention of high-frequency episodic and chronic migraine: Erenumab in Real Life in Italy (EARLY), the first Italian multicenter, prospective real-life study. Headache 61(2):363–372. https://doi.org/10.1111/head.14032
Vernieri F, Altamura C, Brunelli N, Costa CM, Aurilia C, Egeo G, Fofi L, Favoni V, Pierangeli G, Lovati C, Aguggia M, d’Onofrio F, Doretti A, Di Fiore P, Finocchi C, Rao R, Bono F, Ranieri A, Albanese M, Cevoli S, Barbanti P, GARLIT Study Group (2021) Galcanezumab for the prevention of high frequency episodic and chronic migraine in real life in Italy: a multicenter prospective cohort study (the GARLIT study). J Headache Pain 22(1):35
Vernieri F, Brunelli N, Messina R, Costa CM, Colombo B, Torelli P, Quintana S, Cevoli S, Favoni V, d’Onofrio F, Egeo G, Rao R, Filippi M, Barbanti P, Altamura C (2021) Discontinuing monoclonal antibodies targeting CGRP pathway after one-year treatment: an observational longitudinal cohort study. J Headache Pain 22(1):154. https://doi.org/10.1186/s10194-021-01363-y
Gazzetta Ufficiale della Repubblica Italiana, 21/07/2020. Italian Drugs Agency determination of cost and administration of erenumab, galcanezumab and fremanezumab https://www.gazzettaufficiale.it/eli/gu/2020/07/21/182/sg/pdf (Accessed 17/02/2022)
Pensato U, Baraldi C, Favoni V, Mascarella D, Matteo E, Andrini G, Cainazzo MM, Cortelli P, Pierangeli G, Guerzoni S, Cevoli S (2022) Detoxification vs non-detoxification before starting an anti-CGRP monoclonal antibody in medication overuse headache. Cephalalgia. Epub ahead of print. On Feb 9, 2022. https://doi.org/10.1177/03331024211067791.
Raggi A, Grignani E, Leonardi M, Andrasik F, Sansone E, Grazzi L, D’Amico D (2018) Behavioral approaches for primary headaches: recent advances. Headache 58(6):913–925. https://doi.org/10.1111/head.13337
Barbanti P, Fofi L, Cevoli S, Torelli P, Aurilia C, Egeo G, Grazzi L, D’Amico D, Manzoni GC, Cortelli P, Infarinato F, Vanacore N (2018) Establishment of an Italian chronic migraine database: a multicenter pilot study. Neurol Sci 39(5):933–937. https://doi.org/10.1007/s10072-018-3280-y
Funding
The MIND-CM project was funded by the Italian Ministry of Health under grant agreement number RF-2016–02364801. The MOH-Cost study was partially funded by FICEF Onlus.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raggi, A., Grazzi, L., Guastafierro, E. et al. Addressing the cost of chronic and episodic migraine and its main drivers: a short-term longitudinal analysis from a third-level Italian center. Neurol Sci 43, 5717–5724 (2022). https://doi.org/10.1007/s10072-022-06164-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06164-y