Abstract
Introduction
This study aims to evaluate the effect of metabolic syndrome (MetS) and anthropometric indices on carpal tunnel syndrome (CTS).
Methods
Forty-three healthy controls and 41 CTS patients were enrolled. Complaints of patients were assessed by Boston Questionnaire (BQ). MetS components were investigated. Wrist circumference, wrist depth, wrist width, palm width, and palm length were measured. Routine nerve conduction studies of median and ulnar nerves as well as the “sensitive” comparison tests were performed. Cutaneous silent period (CuSP) was studied by stimulating both second and fifth digital nerves while recording over thenar muscles.
Results
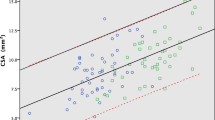
The vast majority of the participants were female and right-handed. CTS was bilateral in 61% of patients. Data of 109 hands were analyzed. MetS was more frequent in CTS patients. BQ scores were not related to MetS. Waist circumference, serum TG, and fasting glucose levels were higher in CTS patients. CTS hands with MetS had lower median CMAP amplitudes and increased sensory thresholds. Sensory thresholds were increased with both median and ulnar nerve stimulations suggesting a wider spread of peripheral nerve excitability changes in MetS presence. CuSPs were recorded from all 109 hands. CuSP latencies and durations were similar between controls and CTS patients. Wrist ratio was the only anthropometric index that was a statistically significant predictor for CTS development.
Conclusion
MetS was more prevalent in CTS patients. Some clinical and electrophysiological features (mainly sensory thresholds) may worsen in presence of MetS, but not the wrist ratio.


Similar content being viewed by others
References
Pourmemari MH, Heliövaara M, Viikari-Juntura E, Shiri R (2018) Carpal tunnel release: lifetime prevalence, annual incidence, and risk factors. Muscle Nerve 58:497–502
Mondelli M, Giannini F, Giacchi M (2002) Carpal tunnel syndrome incidence in a general population. Neurology 58:289–294
Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosén I (1999) Prevalence of carpal tunnel syndrome in a general population. JAMA 282:153–158
Preston DC, Shapiro BE (2013) Electromyography and neuromuscular disorders: clinical-electrophysiologic correlations, 3rd edition
Durham CO, Ravenstein KV (2017) It’s all in the wrist. Diagnosis and management of carpal tunnel syndrome. Orthop Nurs 36:323–327
Jablecki CK, Andary MT, So YT, Wilkins DE, Williams FH (1993) Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. AAEM Quality Assurance Committee Muscle Nerve 16:1392–1414
Alanazy MH (2017) Clinical and electrophysiological evaluation of carpal tunnel syndrome: approach and pitfalls. Neurosciences (Riyadh) 22:169–180
Floeter MK (2003) Cutaneous silent periods. Muscle Nerve 28:391–401
Leis AA, Stetkarova I, Beric A, Stokic DS (1995) Spinal motor neuron excitability during the cutaneous silent period. MuscleNerve 18:1464–1470
Kaneko K, Kawai S, Taguchi T, Fuchigami Y, Yonemura H, Fujimoto H (1998) Cortical motor neuron excitability during cutaneous silent period. Electroencephalogr Clin Neurophysiol 109:364–368
Svilpauskaite J, Truffert A, Vaiciene N, Magistris MR (2006) Cutaneous silent period in carpal tunnel syndrome. Muscle Nerve 33:487–493
Yaman M, Uluduz D, Solak O, Pay G, Kiziltan ME (2007) The cutaneous silent period in carpal tunnel syndrome. Electromyogr Clin Neurophysiol 47:215–220
Koo YS, Park HR, Joo BE, Choi JY, Jung KY, Park KW, Cho SC, Kim BJ (2010) Utility of the cutaneous silent period in the evaluation of carpal tunnel syndrome. Clin Neurophysiol 121:1584–1588
Uchiyama S, Itsubo T, Yasutomi T (2005) Quantitative MRI of the wrist and nerve conduction studies in patient with idiopathic carpal tunnel syndrome. J Neural Neurosurg Psychiatry 76:1103–1108
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. DiabetMed 15:539–553
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002) Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 106:3143–3421
Balci K, Utku U (2007) Carpal tunnel syndrome and metabolic syndrome. Acta Neurol Scand 116:113–117
Onder B, Yalcin E, Selcuk B, Kurtaran A, Akyüz M (2013) Carpal tunnel syndrome and metabolic syndrome co-occurrence. Rheumatol Int 33:583–586
Ozcakir S, Sigirli D, Avsaroglu H (2018) High wrist ratio is a risk factor for carpal tunnel syndrome. Clin Anat 31:698–701
Thiese MS, Merryweather A, Koric A, Ott U, Wood EM, Kapellusch J, Foster J, Garg A, Deckow-Schaefer G, Tomich S, Kendall R, Drury DL, Wertsch J, Hegmann KT, Wistah Study Team (2017) Association between wrist ratio and carpal tunnel syndrome: effect modification by body mass index. Muscle Nerve 56:1047–1053
Arslan Y, Bulbul I, Ocek L, Sener U, Zorlu Y (2017) Effect of hand volume and other anthropometric measurements on carpal tunnel syndrome. Neurol Sci 38:605–610
Kamolz LP, Beck H, Haslik W, Högler R, Rab M, Schrögendorfer KF, Frey M (2004) Carpal tunnel syndrome: a question of hand and wrist configurations? J Hand Surg Br 29:321–324
Hlebš S, Majhenič K, Vidmar G (2014) Body mass index and anthropometric characteristics of the hand as risk factors for carpal tunnel syndrome. Coll Antropol 38:219–226
Levine DW et al (1993) A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. JBJS 75:1585–1592
Sezgin M, Incel NA, Serhan S, Camdeviren H, As I, Erdogan C (2006) Assessment of symptom severity and functional status in patients with carpal tunnel syndrome: reliability and functionality of the Turkish version of the Boston Questionnaire. Disabil Rehabil 28:1281–1285
Werner RA, Andary M (2011) Electrodiagnostic evaluation of carpal tunnel syndrome. Muscle Nerve 44:597–607
American Association of Electrodiagnostic Medicine, American Academy of Neurology, and American Academy of Physical Medicine and Rehabilitation (2002) Practice parameter for electrodiagnostic studies in carpal tunnel syndrome: summary statement. MuscleNerve 25:918–922
Moghtaderi A, Izadi S, Sharafadinzadeh N (2005) An evaluation of gender, body mass index, wrist circumference and wrist ratio as independent risk factors for carpal tunnel syndrome. Acta Neurol Scand 112:375–379
Shiri R, Pourmemari MH, Hassaniand KF, Viikari-Juntura E (2015) The effect of excess body mass on the risk of carpal tunnel syndrome: a meta-analysis of 58 studies. Obes Rev 16:1094–1104
Werner RA, Jacobson JA, Jamadar DA (2004) Influence of body mass index on median nerve function, carpal canal pressure, and cross-sectional area of the median nerve. Muscle Nerve 30:481–485
Spahn G, Wollny J, Hartmann B, Schiele R, Hofmann GO (2012) Metaanalysis for the evaluation of risk factors for carpal tunnel syndrome part I. General factors Z Orthop Unfall 150:503–515
Pourmemari MH, Shiri R (2016) Diabetes as a risk factor for carpal tunnel syndrome: a systematic review and meta-analysis. Diabet Med 33:10–16
Kim YH, Yang KS, Kim H, Seok HY, Lee JH, Son MH, Kim BJ (2017) Does diabetes mellitus influence carpal tunnel syndrome? J Clin Neurol 13:243–249
Tekin F, Surmeli M, Simsek H, Ceran C, Tezcan S, Taner OT, Simsek G (2015) Comparison of the histopathological findings of patients with diabetic and idiopathic carpal tunnel syndrome. Int Orthop 39:2395–2401
Taser F, Deger AN, Deger H (2017) Comparative histopathological evaluation of patients with diabetes, hypothyroidism and idiopathic carpal tunnel syndrome. Turk Neurosurg 6:991–997
Bischoff C, Isenberg C, Conrad B (1991) Lack of hyperlipidemia in carpal tunnel syndrome. Eur Neurol 31:33–35
Nakamichi KI, Tachibana S (2005) Hypercholesterolemia as a risk factor idiopathic carpal tunnel syndrome. Muscle Nerve 32:364–367
Guan W, Lao J, Yudong GU, Zhao X, Rui J, Gao K (2018) Case-control study on individual risk factors of carpal tunnel syndrome. Exp Ther Med 15:2761–2766
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr, International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120:1640–1645
Iftikhar S, Javed MA, Kasuri MN (2016) Frequency of metabolic syndrome and its components in patients with carpal tunnel syndrome. Journal of the College of Physicians and Surgeons Pakistan 26:380–383
Aurora SK, Ahmad BK, Aurora TK (1998) Silent period abnormalities in carpal tunnel syndrome. Muscle Nerve 21:1213–1215
Zhang J, Liu N, Wang YW, Zhang ZC, Zheng LN, Zhu J (2015) Evaluation of the function status of the ulnar nerve in carpal tunnel syndrome. Genet Mol Res 14:3680–3686
Yemisci OU, Yalbuzdag SA, Cosar SN, Oztop P, Karatas M (2011) Ulnar nerve conduction abnormalities in carpal tunnel syndrome. Muscle Nerve 44:352–357
Tinazzi M, Zanette G, Volpato D et al (1998) Neurophysiological evidence of neuroplasticity at multiple levels of the somatosensory system in patients with carpal tunnel syndrome. Brain 121:1785–1794
Lu YC, Zhang H, Zheng MX, Hua XY, Qiu YQ, Shen YD, Jiang S, Xu JG, Gu YD, Xu WD (2017) Local and extensive neuroplasticity in carpal tunnel syndrome: a resting-state fMRI study. Neurorehabil Neural Repair 31:898–909
Kassem HS, Azar ST, Zantout MS, Sawaya RA (2005) Hypertriglyceridemia and peripheral neuropathy in neurologically asymptomatic patients. Neuro Endocrinol Lett 26:775–779
Caglayan HZB, Nazliel B, Irkec C (2013) Nerve conduction velocities in hyperlipidemic patients. Neuro Endocrinol Lett 34:643–647
Kuwabara S, Ogawara K, Harrori T, Suzuki Y, Hashimoto N (2002) The acute effects of glycemic control on axonal excitability in human diabetic nerves. Intern Med 41:360–365
Johnson EW, Gatens T, Poindexter D, Bowers D (1983) Wrist dimensions: correlation with median sensory latencies. ArchPhysMedRehabil 64:556–557
Kuhlman KA, Hennessey WJ (1997) Sensitivity and specificity of carpal tunnel syndrome signs. Am J Phys Med Rehabil 76:451–457
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was given by Ethical Committee of University of Health Sciences Bakirkoy Prof. Dr. Mazhar Osman Training and Research Hospital for Psychiatric, Neurologic and Neurosurgical Diseases with protocol number 25.09.2018–217.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Both Mahir Yusifov and Sezin Alpaydin Baslo will be the first writers as co-authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yusifov, M., Alpaydin Baslo, S., Tekin, B. et al. Metabolic syndrome and anthropometric indices in CTS hands: an electrophysiological study. Neurol Sci 43, 1375–1384 (2022). https://doi.org/10.1007/s10072-021-05430-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-021-05430-9