Abstract
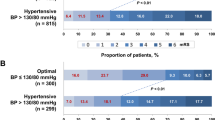
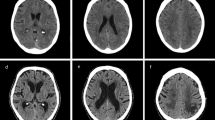
Complete middle cerebral artery (MCA) stroke is a life-threatening condition, which can lead to death in the form of “malignant MCA syndrome”; characterized by massive brain edema and cerebral herniation. Moreover, patients with complete MCA infarct have high mortality due to complications. The aim of this study was to evaluate the clinical predictors of in-hospital mortality in patients with complete MCA stroke. Consecutive patients with complete MCA stroke were enrolled in a prospective single center in-hospital outcome study having mortality as its end point. Among 780 ischemic stroke patients, 125 had complete MCA strokes (16%) and 44 (35.2%) of these died in hospital. A high NIHSS-score (OR 1.17 95%CI 1.03–1.34, P = 0.013) and high diastolic blood pressure on admission (OR 1.05 95%CI 1.01–1.09) resulted being independent predictors of in-hospital mortality in patients with complete MCA stroke. The median value of diastolic blood pressure at admission was 90 mmHg in patients who died and 80 mmHg in survivors (P = 0.01). The risk of death increased by 5% for each mmHg increase in diastolic blood pressure on admission after adjusting for other risk factors. The rate of mortality was 22% in patients with diastolic blood pressure lower than 90 mmHg, 56% for those with diastolic blood pressure between 90 and 109 mmHg and 67% for those with diastolic blood pressure higher than 110 mmHg. This study suggests that high diastolic blood pressure on admission in acute MCA stroke patients is linearly correlated with in-hospital mortality.


Similar content being viewed by others
References
Silver FL, Norris JW, Lewis AJ, Hachinski VC (1984) Early mortality following stroke: a prospective review. Stroke 15:492–496
Ropper AH, Shafran B (1984) Brain oedema after stroke. Clinical syndrome and intracranial pressure. Arch Neurol 41:26–29
Hacke W, Schwab S, Horn M, Spranger M, DeGeorgia M, von Kummer R (1996) ‘Malignant’ middle cerebral artery infarction. Clinical course and prognostic signs. Arch Neurol 53:309–315
Ayata C, Ropper AH (2002) Ischaemic brain oedema. J Clin Neurosci 9:113–124
Frank JI (1995) Large hemispheric infarction, deterioration, and intracranial pressure. Neurology 45:1286–1290
Hofmeijer J, van der Worp HB, Kappelle LJ (2003) Treatment of space-occupying cerebral infarction. Crit Care Med 31:617–625
Kasner SE, Demchuk AM, Berrouschot J, Schmutzhard E, Harms L, Verro P et al (2001) Predictors of fatal brain oedema in massive hemispheric ischemic stroke. Stroke 32:2117–2123
Bamford J, Sandercock P, Dennis M, Burn J, Warlow C (1991) Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 337:1521–1526
Wardlaw JM, Sellar R (1994) A simple practical classification of cerebral infarcts on CT and its interobserver reliability. AJNR Am J Neuroradiol 15:1933–1939
National Institute of Neurological Disorders and Stroke (NINDS) rtPA Stroke Study Group (1995) TPA for acute ischemic stroke. NEJM 333:1581–1587
Wahlgren N, Ahmed N, Davalos A, Ford GA, Grond M, Hacke W et al (2007) Thrombolysis with alteplase for acute ischemic stroke in the Safe Implementation of Thrombolysis in Stroke. Monitoring Study (SITS-MOST): an observational study. Lancet 369:275–282
Adams HP Jr, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
European Stroke Organisation (ESO) Executive Committee; ESO Writing Committee (2008) Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 25(5):457–507
Tikhonoff V, Zhang H, Richart T, Staessen JA (2009) Blood pressure as a prognostic factor after acute stroke. Lancet Neurol 8:938–948
Abboud H, Labreuche J, Plouin F, Amarenco P, GENIC Investigators (2006) High blood pressure in early acute stroke: a sign of a poor outcome? J Hypertens 24:381–386
Qureshi AI (2008) Acute hypertensive response in patients with stroke. Pathophysiology and management. Circulation 118:176–187
Olsen TS, Larsen B, Herning M, Skriver EB, Lassen NA (1983) Blood flow and vascular reactivity in collaterally perfused brain tissue. Evidence of an ischemic penumbra in patients with acute stroke. Stroke 14:332–341
Ahmed N, Näsman P, Wahlgren NG (2000) Effect of intravenous nimodipine on blood pressure and outcome after acute stroke. Stroke 31(6):1250–1255
Schrader J, Lüders S, Kulschewski A et al (2003) The ACCESS Study. Evaluation of acute candesartan cilexetil therapy in stroke survivors. Stroke 34:1699–1703
Blood pressure in Acute Stroke Collaboration (BASC): Interventions for deliberately altering blood pressure in acute stroke. Cochrane Database Syst Rev 2001:CD000039
The ENOS Investigators (2006) Glyceryl trinitrate vs. control, and continuing vs. stopping temporarily antihypertensive therapy, in acute stroke: rationale and design of the Efficacy of Nitric Oxide in Stroke (ENOS) trial (ISRCTN99414122). Int J Stroke 1:245–49
Acute Candesartan Cilexetil Outcomes Stroke Trial (ACCOST). NCT00108706. http://www.clinicaltrials.gov/ct2/show/NCT00108706
Acknowledgments
Valeria Caso has served on the speaker’s bureau of Boehringer Ingelheim. Giancarlo Agnelli has received honoraria as a member of the speakers’ bureaus of Astra Zeneca and Bayer. Maurizio Paciaroni has served on the speakers’ bureaus of Sanofi Aventis, Guidotti and Boehringer Ingelheim.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Caso, V., Agnelli, G., Alberti, A. et al. High diastolic blood pressure is a risk factor for in-hospital mortality in complete MCA stroke patients. Neurol Sci 33, 545–549 (2012). https://doi.org/10.1007/s10072-011-0767-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-011-0767-1