Abstract
Introduction
Disease Activity Score-28 (DAS28) with erythrocyte sedimentation rate (DAS28ESR), DAS28 with C-reactive protein (DAS28CRP), and simplified disease activity index (SDAI) are widely used to assess disease activity as low, moderate, or high or in remission in patients with rheumatoid arthritis (RA). However, these indicators can generate inconsistent results, influencing treatment decisions and limiting comparisons across studies. We aimed to establish equations for conversion from DAS28ESR and DAS28CRP to SDAI.
Methods
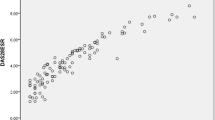
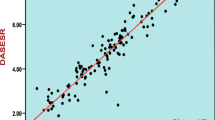
We conducted a retrospective study, including 933 outpatients who were simultaneously assessed using DAS28ESR, DAS28CRP, and SDAI. The patients were divided into a training set (70%) and a validation set (30%). We developed equations to convert DAS28ESR and DAS28CRP values into SDAI values by bisquare-weighted robust regression to obtain SDAI–DAS28ESR and SDAI–DAS28CRP. In addition to using kappa values to assess consistency, differences in disease activity classification between SDAI–DAS28ESR and SDAI–DAS28CRP were examined by the Stuart–Maxwell test and the Bowker test.
Results
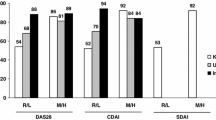
Two quadratic equations were developed as follows: SDAI–DAS28ESR = 1.168 × (DAS28ESR)^2 − 2.432 × (DAS28ESR) + 2.649 and SDAI–DAS28CRP = 1.2 × (DAS28CRP)^2 − 0.3522 × (DAS28CRP) − 0.6014. After applying the equations, the Stuart–Maxwell test and the Bowker test were no longer significant between SDAI–DAS28ESR and SDAI or between SDAI–DAS28CRP and SDAI. The kappa values increased from 0.57 to 0.73 between SDAI–DAS28ESR and SDAI and 0.76 to 0.86 between SDAI–DAS28CRP and SDAI.
Conclusion
SDAI–DAS28ESR and SDAI–DAS28CRP are interchangeable with the SDAI on the group level, which will facilitate comparisons among studies. In addition, the equations improved consistency between indicators.
Key Points • There is disagreement in assessing disease activity in patients with rheumatoid arthritis between Disease Activity Score-28 (DAS28) with erythrocyte sedimentation rate (DAS28ESR), DAS28 with C-reactive protein (DAS28CRP), and simplified disease activity index (SDAI). • We developed and validated two quadratic equations to convert DAS28ESR and DAS28CRP into SDAI. We found there was no longer significant difference in disease activity between indicators after applying the equations. • This work may allow comparisons across studies which use different indicators. |

Similar content being viewed by others
References
McInnes IB, Schett G (2011) The pathogenesis of rheumatoid arthritis. N Engl J Med 365(23):2205–2219. https://doi.org/10.1056/NEJMra1004965
Smolen JS, Aletaha D, Bijlsma JW, Breedveld FC, Boumpas D, Burmester G et al (2010) Treating rheumatoid arthritis to target: recommendations of an international task force. Ann Rheum Dis 69(4):631–637. https://doi.org/10.1136/ard.2009.123919
Aletaha D, Smolen JS (2019) Remission in rheumatoid arthritis: missing objectives by using inadequate DAS28 targets. Nat Rev Rheumatol 15(11):633–634. https://doi.org/10.1038/s41584-019-0279-6
Mierau M, Schoels M, Gonda G, Fuchs J, Aletaha D, Smolen JS (2007) Assessing remission in clinical practice. Rheumatology (Oxford) 46(6):975–979. https://doi.org/10.1093/rheumatology/kem007
Smolen JS, Landewé RBM, Bijlsma JWJ, Burmester GR, Dougados M, Kerschbaumer A et al (2020) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis 79(6):685–699. https://doi.org/10.1136/annrheumdis-2019-216655
Combe B, Landewe R, Daien CI, Hua C, Aletaha D, Álvaro-Gracia JM et al (2017) 2016 update of the EULAR recommendations for the management of early arthritis. Ann Rheum Dis 76(6):948–959. https://doi.org/10.1136/annrheumdis-2016-210602
Smolen JS, Landewé R, Breedveld FC, Buch M, Burmester G, Dougados M et al (2014) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis 73(3):492–509. https://doi.org/10.1136/annrheumdis-2013-204573
Singh JA, Saag KG, Bridges SL Jr, Akl EA, Bannuru RR, Sullivan MC et al (2016) 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res 68(1):1–25. https://doi.org/10.1002/acr.22783
Singh JA, Furst DE, Bharat A, Curtis JR, Kavanaugh AF, Kremer JM et al (2012) 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res 64(5):625–639. https://doi.org/10.1002/acr.21641
Dasgupta A, Ward MM (2019) Translating treatment effects between rheumatoid arthritis activity measures and American College of Rheumatology responses in direct comparison trials. Arthritis Care Res 71(11):1482–1487. https://doi.org/10.1002/acr.23825
Hazlewood GS, Barnabe C, Tomlinson G, Marshall D, Devoe D, Bombardier C (2016) Methotrexate monotherapy and methotrexate combination therapy with traditional and biologic disease modifying antirheumatic drugs for rheumatoid arthritis: abridged Cochrane systematic review and network meta-analysis. BMJ (Clinical research ed) 353:i1777. https://doi.org/10.1136/bmj.i1777
Anderson J, Caplan L, Yazdany J, Robbins ML, Neogi T, Michaud K et al (2012) Rheumatoid arthritis disease activity measures: American College of Rheumatology recommendations for use in clinical practice. Arthritis Care Res 64(5):640–647. https://doi.org/10.1002/acr.21649
Prevoo ML, van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL (1995) Modified disease activity scores that include twenty-eight-joint counts Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis and rheumatism 38(1):44–8. https://doi.org/10.1002/art.1780380107
Fransen J, Welsing PM, Keijzer RM , Van Riel PLCM (2004) Disease activity scores using C-reactive protein: CRP may replace ESR in the assessment of RA disease activity. Ann Rheum Dis 62(Suppl 1):151
Smolen JS, Breedveld FC, Schiff MH, Kalden JR, Emery P, Eberl G et al (2003) A simplified disease activity index for rheumatoid arthritis for use in clinical practice. Rheumatology (Oxford) 42(2):244–257. https://doi.org/10.1093/rheumatology/keg072
Aletaha D, Ward MM, Machold KP, Nell VP, Stamm T, Smolen JS (2005) Remission and active disease in rheumatoid arthritis: defining criteria for disease activity states. Arthritis Rheum 52(9):2625–2636. https://doi.org/10.1002/art.21235
Fujiwara M, Kita Y (2013) Reexamination of the assessment criteria for rheumatoid arthritis disease activity based on comparison of the Disease Activity Score 28 with other simpler assessment methods. Mod Rheumatol 23(2):260–268. https://doi.org/10.1007/s10165-012-0652-7
Matsui T, Kuga Y, Nishino J, Kaneko A, Eto Y, Tohma S (2011) Comparison of composite disease activity indices for rheumatoid arthritis. Mod Rheumatol 21(2):134–143. https://doi.org/10.1007/s10165-010-0367-6
Medeiros MMdC, Oliveira BMGBd, Cerqueira JVMd, Quixadá RTdS, Oliveira ÍMAXd (2015) Correlation of rheumatoid arthritis activity indexes (Disease Activity Score 28 measured with ESR and CRP, simplified disease activity index and clinical disease activity index) and agreement of disease activity states with various cut-off points in a Northeastern Brazilian population. Revista Brasileira de Reumatologia (English Edition) 55(6):477–84. https://doi.org/10.1016/j.rbre.2014.12.005
Slama IB, Allali F, Lakhdar T, El Kabbaj S, Medrare L, Ngeuleu A et al (2015) Reliability and validity of CDAI and SDAI indices in comparison to DAS-28 index in Moroccan patients with rheumatoid arthritis. BMC Musculoskelet Disord 16:268. https://doi.org/10.1186/s12891-015-0718-8
Martins FM, da Silva JA, Santos MJ, Vieira-Sousa E, Duarte C, Santos H et al (2015) DAS28, CDAI and SDAI cut-offs do not translate the same information: results from the Rheumatic Diseases Portuguese Register Reuma.pt. Rheumatology (Oxford, England). 54(2):286–91. https://doi.org/10.1093/rheumatology/keu313
Song X, Wang YH, Li MT, Duan XW, Li HB, Zeng XF (2021) Chinese registry of rheumatoid arthritis: IV. Correlation and consistency of rheumatoid arthritis disease activity indices in China. Chin Med J 134(12):1465–70. https://doi.org/10.1097/cm9.0000000000001517
Restrepo-Correa R, Rodríguez-Padilla LM, Zapata-Castellanos AL, Ocampo A, García JJ, Muñoz-Grajales C et al (2018) Concordance and correlation of activity indices in patients with rheumatoid arthritis in northwestern Colombia: a cross-sectional study. Int J Rheum Dis 21(11):1946–1954. https://doi.org/10.1111/1756-185x.13227
Smolen JS, Aletaha D, Gruben D, Zwillich SH, Krishnaswami S, Mebus C (2017) Brief report: remission rates with tofacitinib treatment in rheumatoid arthritis: a comparison of various remission criteria. Arthritis & rheumatology (Hoboken, NJ) 69(4):728–734. https://doi.org/10.1002/art.39996
Gaujoux-Viala C, Mouterde G, Baillet A, Claudepierre P, Fautrel B, Le Loët X et al (2012) Evaluating disease activity in rheumatoid arthritis: which composite index is best? A systematic literature analysis of studies comparing the psychometric properties of the DAS, DAS28, SDAI and CDAI. Joint bone spine 79(2):149–155. https://doi.org/10.1016/j.jbspin.2011.04.008
Leong KP, Tan JWL, Gao X, Koh ET (2020) Conversion among the 28-joint count activity indices for rheumatoid arthritis. Eur J Rheumatol 7(3):105–111. https://doi.org/10.5152/eurjrheum.2020.19199
Aletaha D, Smolen JS (2011) Joint damage in rheumatoid arthritis progresses in remission according to the Disease Activity Score in 28 joints and is driven by residual swollen joints. Arthritis Rheum 63(12):3702–3711. https://doi.org/10.1002/art.30634
van der Heijde D, Klareskog L, Boers M, Landewé R, Codreanu C, Bolosiu HD et al (2005) Comparison of different definitions to classify remission and sustained remission: 1 year TEMPO results. Ann Rheum Dis 64(11):1582–1587. https://doi.org/10.1136/ard.2004.034371
Schoels M, Alasti F, Smolen JS, Aletaha D (2017) Evaluation of newly proposed remission cut-points for disease activity score in 28 joints (DAS28) in rheumatoid arthritis patients upon IL-6 pathway inhibition. Arthritis Res Ther 19(1):155. https://doi.org/10.1186/s13075-017-1346-5
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31(3):315–324. https://doi.org/10.1002/art.1780310302
Inoue M, Kanda H, Tateishi S, Fujio K (2020) Evaluation of response criteria in rheumatoid arthritis treated with biologic disease-modifying antirheumatic drugs. Arthritis Care Res 72(7):942–949. https://doi.org/10.1002/acr.23914
Stuart A(1955) A test for homogeneity of the marginal distributions in a two-way classification. Biometrika 42(3–4):412–416
Maxwell AE (1970) Comparing the classification of subjects by two independent judges. B J Psychiatry: J Ment Sci 116(535):651–655. https://doi.org/10.1192/bjp.116.535.651
McNemar Q (1947) Note on the sampling error of the difference between correlated proportions or percentages. Psychometrika 12(2):153–157
Bowker AH (1948) A test for symmetry in contingency tables. J Am Stat Assoc 43(244). https://doi.org/10.2307/2280710
Uebersax J. User Guide for the MH Program (v. 1.2) Tests of marginal homogeneity for two-way tables. http://www.john-uebersax.com/stat/mh.htm. Accessed 22 May 2021
Hmamouchi I, Combe B, Fautrel B, Rincheval N, Lukas C (2014) Prevalence and concordance of early and sustained remission assessed by various validated indices in the early arthritis “ESPOIR” cohort. Joint Bone Spine 81(5):409–415. https://doi.org/10.1016/j.jbspin.2014.02.007
Alma ÖG (2011) Comparison of robust regression methods in linear regression. Int J Comput Math Sci 6(9):409–421
Fleischmann R, van der Heijde D, Koenig AS, Pedersen R, Szumski A, Marshall L et al (2015) How much does Disease Activity Score in 28 joints ESR and CRP calculations underestimate disease activity compared with the simplified disease activity index? Ann Rheum Dis 74(6):1132–1137. https://doi.org/10.1136/annrheumdis-2013-204920
Sheehy C, Evans V, Hasthorpe H, Mukhtyar C (2014) Revising DAS28 scores for remission in rheumatoid arthritis. Clin Rheumatol 33(2):269–272. https://doi.org/10.1007/s10067-013-2468-z
Wetteland P, Røger M, Solberg HE, Iversen OH (1996) Population-based erythrocyte sedimentation rates in 3910 subjectively healthy Norwegian adults. A statistical study based on men and women from the Oslo area. J Int Med 240(3):125–31. https://doi.org/10.1046/j.1365-2796.1996.30295851000.x
Jin S, Li M, Fang Y, Li Q, Liu J, Duan X et al (2017) Chinese Registry of rheumatoid arthritis (CREDIT): II. Prevalence and risk factors of major comorbidities in Chinese patients with rheumatoid arthritis. Arthritis Res Ther 19(1):251. https://doi.org/10.1186/s13075-017-1457-z
Acknowledgements
We would like to thank all the patients and healthcare professionals who participated in this study.
Funding
This work was supported by a research grant from the National Science and Technology Major Project for Major New Drugs Innovation and Development (no. 2018ZX09734003) and National Natural Science Foundation of China (no. 82171780).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pu, Lm., Liu, Y., Zhou, Dx. et al. Development and validation of equations for conversion from DAS28ESR and DAS28CRP to the SDAI in patients with rheumatoid arthritis. Clin Rheumatol 41, 3697–3706 (2022). https://doi.org/10.1007/s10067-022-06259-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06259-z