Abstract
Objectives
The aim was to comparatively assess the clinical and imaging features in patients with SAPHO syndrome.
Methods
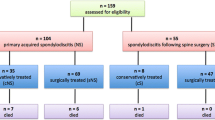
The clinical data, laboratory results, imaging data of forty-six SAPHO patients were reviewed and the SAPHO patients were divided into spinal involvement group and non-spinal involvement group. Fifty patients with ankylosing spondylitis were recruited as control group. The clinical and radiological features of them were analyzed and compared.
Results
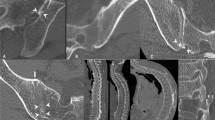
Thirty-four of 46 (73.9%) of all the SAPHO patients had spinal involvement. The lesions exhibited as abnormal hyper-intensity signal in vertebral bodies, vertebral body erosion or collapse, bone marrow edema, endplate inflammation, spondyldiscitis, paravertebral ossification, and facet joint involvement. Compared with patients in non-spinal involvement group, the age at disease onset was older (P = 0.033), the disease duration was longer (P = 0.048), and CRP level was elevated (P = 0.047) in patients in spinal involvement group. Compared with patients with ankylosing spondylitis, SAPHO patients were more likely to have cervical vertebra involvement (P = 0.024), endplate inflammation (P = 0.019), and spondyldiscitis (P = 0.001), but less multiple vertebral body and facet joint involvement (P = 0.002). Patients regularly received DMARDS or biologics treatment had symptoms relieved and lesions turned into chronic stage or better than before.
Conclusions
A total of 73.9% of the SAPHO patients had spinal involvement and the involvement could affect any part of the spine. Cervical vertebral involvement, endplate inflammation, and sponlypodiscitis were more common in SAPHO than in patients with ankylosing spondylitis. In SAPHO patients with spinal involvement, the disease duration was longer and the inflammatory reaction was more intensive. DMARDs and biologics may help to prevent the disease progress.
Key points: • To the best of our knowledge, this paper is the first one to comparatively study the clinical and radiological features of SAPHO syndrome, especially the characteristics of spinal involvement. |





Similar content being viewed by others
References
Chamot A M, Benhamou C L, Kahn M F, Beraneck, L, Kaplan G, Prost A. Acne-pustulosis-hyperostosis-osteitis syndrome. Results of a national survey. 85 cases. Rev Rhum Mal Osteoartic 1987;54:187–196
Kahn MF, Khan MA (1994) The SAPHO syndrome. Baillieres Clin Rheumatol 8:333–362
Cotten A, Flipo RM, Mentre A, Delaporte E, Duquesnoy B, Chastanet P (1995) SAPHO syn- drome. RadioGraphics 15:1147–1154
Boutin RD, Resnick D (1998) The SAPHO syndrome: an evolving concept for unifying several idiopathic disorders of bone and skin. AJR Am J Roentgenol 170:585–591
Laredo JD, Vuillemin-Bodaghi V, Boutry N, Cotten A, Parlier-Cuau C (2007) SAPHO syndrome: MR appearance of vertebral involvement. Radiology 242:825–831
Govoni M, Colina MA, Trotta F (2009) SAPHO syndrome and infections. Autoimmun Rev 8:256–259
Nguyen MT, Borchers A, Selmi C, Naguwa SM, Cheema G, Gershwin ME (2012) The SAPHO syndrome. Semin Arthritis Rheum 42:254–265
Na D, Xiao C, Liu Y, Wang J, Wang Z (2016) Multimodal imaging findings of SAPHO syndrome with no skin lesions: a report of three cases and review of the literature. Exp Ther Med 12:2665–2670
Mcgauvran AM, Kotsenas AL, Diehn FE, Wald JT, Carr CM, Morris JM (2016) SAPHO syndrome: imaging findings of vertebral involvement. AJNR Am J Neuroradiol 37:1567–1572
Kundu BK, Naik AK, Bhargava S, Srivastava D (2013) Diagnosing the SAPHO syndrome: a report of three cases and review of literature. Clin Rheumatol 32:1237–1243
Doornum SV, Barraclough D, Mccoll G, Wicks I (2000) SAPHO: rare or just not recognized? Semin Arthritis Rheum 30:70–77
Rukavina ISAPHO (2015) Syndrome: a review. J Child Orthop 9:19–27
Sapho HG (1999) Syndrome. A long-term follow-up study of 120 case. Semin Arthritis Rheum 29:159–171
Zimmermann P, Curtis N (2016) Synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome-a challenging diagnosis not to be missed. J Inf Secur 5:106–114
Queiro R, Alonso S, Alperi M, Fernández M, Tejón P, Riestra JL et al (2012) Entheseal ultrasound abnormalities in patients with sapho syndrome. Clin Rheumatol 31:913–919
Hurtado-Nedelec M, Chollet-Martin S, Nicaise-Roland P, Grootenboer-Mignot S, Ruimy R, Meyer O et al (2008) Characterization of the immune response in the synovitis, acne, pustulosis, hyperostosis, osteitis (SAPHO) syndrome. Rheumatology (Oxford) 47:1160–1167
Ferguson PJ, Lokuta MA, El-Shanti HI, Muhle L, Bing X, Huttenlocher A (2010) Neutrophil dysfunction in a family with a SAPHO syndrome-like phenotype. Arthritis Rheum 58:3264–3269
Earwaker JWS, Cotten A (2003) SAPHO: syndrome or concept? Imaging findings. Skelet Radiol 32:311–327
Maugars Y, Berthelot JM, Ducloux JM, Prost A (1995) SAPHO syndrome: a followup study of 19 cases with special emphasis on enthesis involvement. J Rheumatol 22:2135–2141
Takigawa T, Tanaka M, Nakanishi K, Misawa H, Sugimoto Y, Takahata T, Nakahara H, Nakahara S, Ozaki T (2008) SAPHO syndrome associated spondylitis. Eur Spine J 17:1391–1397
Xu W, Li C, Zhao X, Lu J, Li L, Wu N, Zuo Y, Jing H, Dong Z, Zhang W, Zhang W (2017) Whole-spine computed tomography findings in SAPHO syndrome. J Rheumatol 44:648–654
Leone A, Cassar-Pullicino VN, Casale R, Magarelli N, Semprini A, Colosimo C (2015) The SAPHO syndrome revisited an emphasis on spinal manifestations. Skelet Radiol 44:9–24
Paparo F, Aleo E, Revelli M et al (2013) Spondyloarthropathies: what radiologists should know. ECR
Toussirot E, Dupond JL, Wendling D (1997) Spondylodiscitis in SAPHO syndrome. A series of eight cases. Ann Rheum Dis 56:52–58
Sonozaki H, Kawashima M, Hongo O, Yaoita H, Ikeno M, Okai K et al (1981) Incidence of arthro-osteitis in patients with pustulosis palmaris et plantaris. Ann Rheum Dis 40:554–557
Rudwaleit M, Landewe R, van der Heijde D, Listing J, Brandt J, Braun J, Burgos-Vargas R, Collantes-Estevez E, Davis J, Dijkmans B, Dougados M, Emery P, van der Horst-Bruinsma IE, Inman R, Khan MA, Leirisalo-Repo M, van der Linden S, Maksymowych WP, Mielants H, Olivieri I, Sturrock R, de Vlam K, Sieper J (2009) The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis: classification of paper patients by expert opinion including uncertainty appraisal. Ann Rheum Dis 68:770–776
Iampreechakul P, Lertbutsayanukul P, Suanprasert N (2019) Acute calcific discitis or symptomatic calcified Schmorl’s node of the upper thoracic spine in an adult: a case report and literature review. Asian J Neurosurg 14(3):1021–1029
Grivé E, Rovira A, Capellades J, Rivas A, Pedraza S (1999) Radiologic findings in two cases of acute Schmörl’s nodes. AJNR Am J Neuroradiol 20(9):1717–1721
Nicolas, Amoretti, Sylvain et al (2019) Symptomatic Schmorl’s nodes: role of percutaneous vertebroplasty. Open study on 52 patients. Neuroradiology 61(4):405–410
Takatalo J, Karppinen J, Niinimaki J, Taimela S, Mutanen P, Sequeiros RB, Nayha S, Jarvelin MR, Kyllonen E, Tervonen O (2012) Association of modic changes, Schmorl’s nodes, spondylolytic defects, highintensity zone lesions, disc herniations, and radial tears with low back symptom severity among young Finnish adults. Spine. 37:1231–1239
Williams FM, Manek NJ, Sambrook PN, Spector TD, Macgregor AJ. Schmorl’s nodes: common,highly heritable, and related to lumbardisc disease. Arthritis Rheum2007;57:855–860, Schmorl’s nodes: c
Assmann G, Kueck O, Kirchhoff T, Rosenthal H, Voswinkel J, Pfreundschuh M et al (2009) Efficacy of antibiotic therapy for SAPHO syndrome is lost after its discontinuation: an interventional study. Arthritis Res Ther 11:1–8
Firinu D, Garcialarsen V, Manconi PE, Del Giacco SR (2016) SAPHO syndrome: current developments and approaches to clinical treatment. Curr Rheumatol Rep 18:35
Burgemeister LT, Baeten DL, Tas SW (2012) Biologics for rare inflammatory diseases: TNF blockade in the SAPHO syndrome. Neth J Med 70:444–449
Ben Abdelghani K, Dran DG, Gottenberg JE, Morel J, Sibilia J, Combe B (2010) Tumor necrosis factor-alpha blockers in SAPHO syndrome. J Rheumatol 37:1699–1704
Funding
This study was supported by a Project of The National Natural Science Foundation of China (81501390).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gao, S., Deng, X., Zhang, L. et al. The comparison analysis of clinical and radiological features in SAPHO syndrome. Clin Rheumatol 40, 349–357 (2021). https://doi.org/10.1007/s10067-020-05187-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05187-0