Abstract
Pulmonary arterial hypertension (PAH) is a severe complication and leading cause of mortality in patients with primary Sjogren’s syndrome (pSS). This study was to investigate the overall survival rates and the utility of red blood cell distribution width (RDW) as a potential prognostic factor of pSS-PAH. This cohort study retrospectively enrolled 55 patients with pSS-PAH who were followed up at the Department of Rheumatology of Peking Union Medical College Hospital (PUMCH) between August 2007 and May 2017. The patients were stratified according to the level of RDW (≤ 15.0 and > 15.0%). Baseline demographics, laboratory results, pulmonary function conditions, hemodynamic assessments, and treatment regimens were analyzed. Cox proportional hazards regression analysis was used to identify whether RDW level is a factor related to adverse outcome. A total of 55 patients were recruited, with an average age of 38.9 ± 9.3 years. Fifty-four were female (98.2%), and the average duration at the time of PAH diagnosis was 25.5 ± 33.2 months. Higher RDW levels were found in patients who deceased in follow-up (13.8 ± 2.6 vs 16.5 ± 1.6%, p = 0.003) and with higher NYHA classes (13.8 ± 1.8 vs 16.5 ± 2.9%, p < 0.001). Patients with RDW > 15% had a significantly worse overall survival than patients with RDW ≤ 15% (3-year survival rate 59.5 vs. 88.7% log-rank p = 0.015). Cox regression analysis identified RDW > 15% as a prognostic factor for adverse outcome (HR 1.786, 95% CI 1.137–2.803, p = 0.012). RDW can serve as a potential negative prognostic factor of pSS-PAH.
Similar content being viewed by others
Introduction
Pulmonary artery hypertension (PAH) is a severe complication of primary Sjogren’s syndrome (pSS) and one of the leading causes of morbidity and mortality for these patients. Although pSS (15.3%) is less likely to be the underlying connective tissue disease of the PAH patients than systemic lupus erythematosus (SLE) (58.4%) and systemic sclerosis (SSc) (26.3%) [1], outcomes are generally poor for patients with pSS-PAH and are even worse than patients with idiopathic PAH (iPAH) [2]. Treatment of PAH associated with pSS (pSS-PAH) is still challenging, though several PAH-specific therapies have been implemented since the last decades. Accurate risk stratification of patients with pSS-PAH is critically important to efficiently target the use of evidence-based therapies and identify high-risk patients who may benefit from advanced treatments. Thus, new prognostic markers may aid to identify at-risk patients early and may provide insight into therapeutic avenues for patients with pSS-PAH. A variety of such markers have been used to create predictive models for survival in patients with chronic heart failure, as well as idiopathic pulmonary arterial hypertension (IPAH), the experience of which could be gained to enlighten prognosis prediction in patients with pSS-PAH [3, 4].
Red blood cell distribution width (RDW) is one of the parameters routinely reported in the complete blood cell count test, pointing to the degree of an isocytosis in the complete blood count. It has been used in routine practice for several decades to make a differential diagnosis for various cases of anemia, such as an iron deficiency anemia [5, 6]. RDW level is elevated in several aberrations (e.g., iron deficiency, inflammation, and uremia), as both destruction and decreased production of red blood cells can increase its value. An independent association between increased RDW and the risk for adverse outcomes has been revealed in patients with acute and chronic heart failure, as well as iPAH, where it outperformed plenty of widely used markers, including NT-proBNP and 6-min walking distance (6MWD) [4, 7,8,9]. Furthermore, a lot more recent studies demonstrated that higher RDW levels may also correlate with long-term survival of other cardiopulmonary diseases, such as chronic obstructive pulmonary disease (COPD), pulmonary embolism (PE), and acute coronary syndrome (ACS) [10,11,12]. RDW has been identified as a simple and readily available marker of the development of PAH in patients with SSc [13]. However, no study till now has examined the association of RDW with the overall survival of PAH in pSS patients. Since identification of more readily prognostic markers may improve clinical decision making, provide insights into the pathophysiology of disease, and also help improve patient management, confirming the validity of RDW level as a prognostic predictor seems to be necessary.
We hypothesized that elevated RDW levels may be associated with the outcome of pSS-PAH patients and may serve as a potential prognostic predictor. The aim of this single-center, retrospective cohort study was to investigate the overall survival and utility of RDW as a simple and readily available prognostic factor of pSS-PAH patients, and its potential function in clinical practice.
Materials and methods
Study population
Fifty-five patients with pSS-PAH who were followed up at the Rheumatology Department of Peking Union Medical College Hospital (PUMCH) from August 2007 to May 2017 were enrolled in this study. Written informed consent was obtained from each patient before enrollment. pSS was diagnosed according to the revised criteria proposed by the American-European Consensus Group in 2002 [14]. Identification of PAH was based on the 2015 European Society of Cardiology/European Respiratory Society guidelines as mean pulmonary arterial pressure (mPAP) ≥ 25 mmHg at rest, pulmonary artery wedge pressure (PAWP) ≤ 15 mmHg, and pulmonary vascular resistance (PVR)> 3 Wood units in right heart catheterization (RHC) assessment [15]. The exclusion criteria were: (1) patients with pulmonary venous hypertension, chronic thromboembolic disease, or significant interstitial lung disease (ILD); (2) patients with comorbidities that may influence RDW levels, such as renal insufficiency, severe anemia, existing left heart diseases, cerebrovascular diseases, malnutrition, or blood transfusion. Renal insufficiency is defined as serum creatinine greater than 1.5 mg/dL (132.6 μmol/L) in men and greater than 1.2 mg/dL (106.1 μmol/L) in women. Anemia is defined as hemoglobin lower than 120 g/L. This study was approved by the medical ethics committee of PUMCH and was conducted in compliance with the ethics committee requirements. The ethical approval number is S-191.
Data collection
Demographic characteristics and clinical features, such as age, gender, disease duration, as well as the comorbidities which could affect prognosis (such as COPD, diabetes melitus, obesity, malignancy, and so on), were recorded at baseline from electronic medical record system. Results of laboratory tests, including complete blood count (covering RDW, mean cell volume, and hematocrit), inflammatory markers (including erythrocyte sedimentation rate (ESR) and high sensitivity C reactive protein (hsCRP)), creatinine (Cr), blood urea nitrogen (BUN), and N-terminal pro-brain natriuretic peptide (NT-pro BNP), were measured using an automatic hematology system on the day when the patient was diagnosed with PAH. RDW lower than 15% in our laboratory is defined as normal. The 6MWD and New York Heart Association (NYHA) functional classification was determined on the same day with blood sample collection by a team of experienced physicians. All the patients underwent RHC at baseline to firmly diagnose PAH, and various hemodynamic parameters, including mPAP, PAWP, cardiac indexes (CI), and PVR, were measured during assessment. Pulmonary function tests, including forced vital capacity (FVC), total lung capacity (TLC), and diffusing capacity for carbon monoxide (DLCO), were performed using standard methods. Conditions of treatments were also gathered on enrollment. Glucocorticoids and immune suppressants were routinely administered. Basic treatments for PAH (e.g., diuretics, digoxin, antiplatelet, and anticoagulant therapy) were given when it is necessary. PAH-targeted therapies, including endothelial blockers, phosphodiesterase inhibitors, and prostacyclin derivatives, were used in compliance with current guidelines and depending on their availability in China.
Statistical analysis
All the patients were stratified according to the level of RDW (< 15.0%, and > 15.0%). Continuous variables were expressed as mean ± SD and compared using Student’s t test between groups. Categorical variables were presented as numbers and percentages (%), the clinically relevant differences of which were evaluated by Chi-square test or Fischer’s exact test, as appropriate. Because of the ambiguously ascribed causes of death, the primary end-point of this study was all-cause death. Survival analysis was performed using Kaplan-Meier analysis, while comparison between groups using the log-rank test. Besides the analysis of all-cause mortality, 1-, 3-, and 5-year survival rates were also assessed. Correlations between RDW and some relevant variables in clinical practice were determined using Spearman’s correlation coefficient. Univariate Cox proportional regression analyses were performed to identify whether the RDW level is a potential predictor of mortality. Statistical analyses were performed using SPSS statistics version 24.0 (IBM, Armonk, NY, USA). A p value < 0.05 was considered statistically significant.
Results
Demographics and clinical characteristics
The baseline characteristics of 55 patients divided according to levels of RDW are presented in Table 1. For the overall study population, the mean age was 38.9 ± 9.3 (24–62) years old with 98.2% female subjects. There were no significant differences in gender, age, disease duration, or comorbidities between the group with normal RDW levels and the other group with elevated RDW levels. RDW ranged from 12.3 to 23.9% (mean14.9 ± 2.5%SD), and 22 patients (40.0%) had an RDW above the upper limit of normal (15%). Patients with higher RDW did not differ significantly from other subjects in most red blood cell variables, including the frequency of anemia, levels of hemoglobin and hematocrit. Although it is not statistically significant (p = 0.053), elevated RDW was associated with lower mean corpuscular volume (MCV). Neither impaired renal function parameters, including creatinine levels and blood urea nitrogen, nor NT-proBNP levels which usually increase in heart failure showed significant difference between groups with normal and elevated RDW levels. Meanwhile, no strong increases in ESR and hsCRP as RDW levels elevated were found as expected. RHC was undertaken in all the subjects. Overall, all the patients in this study cohort had hemodynamic changes (right atrial pressure 6.81 ± 5.02 mmHg, mPAP 49.9 ± 9.5 mmHg, cardiac index 2.5 ± 0.75 L/min/ m2, and PVR 8.2 ± 3.0 Wood units) and poor cardiac function status (52.7% in WHO class II and 47.3% in class III). However, no significant differences are found between the two groups. As for the respiratory markers, TLC was significantly lower in patients with elevated RDW (p = 0.017). The patients in the elevated RDW levels had markedly lower DLCO% compared to patients in the normal range (p = 0.034). The 6MWD showed no significant difference. At the therapeutic level, although the patients had received different therapies at baseline, there was no significant difference in the medication usage between the group with normal RDW level and the one with elevated RDW level. Patients who deceased in the follow-up tended to have higher baseline RDW values (13.8 ± 2.6 vs 16.5 ± 1.6%, p = 0.003; shown in Fig. 1a). Mean RDW levels were significantly higher among patients in WHO class III than those in class II (13.8 ± 1.8 vs 16.5 ± 2.9%, p < 0.001, shown in Fig. 1b).
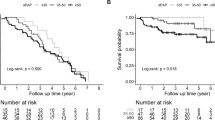
Red blood cell distribution width and survival
During a mean follow-up period of 40.2 ± 31.5 (2.8–146) months, 7 (12.7%) patients died. Four patients were lost to follow-up. For the entire study population, overall 1-, 3-, and 5-year survival rates from the time of diagnosis were 98.1, 82.2, and 75.3%, respectively. Patients with RDW > 15% had a significantly worse 3-year overall survival than patients with RDW ≤ 15% (59.5 vs. 88.7%, log rank test, p = 0.015). Patients with elevated RDW had shorter expected overall survival than patients with normal RDW (132.7 vs 52.7 months, log-rank test, p = 0.015). The Kaplan-Meier overall survival curves showed a significant separation in the two subgroups (Fig. 2).
Identification of RDW as a prognostic factor
The results of univariate Cox proportional regression analysis verified that elevated baseline RDW level (HR 1.79, 95% CI 1.14–2.80, p = 0.012) was a potential risk factor for poor overall survival and clinical outcomes (Table 2). A graphic representation of the Spearman’s correlation coefficient between RDW and NT-proBNP, as well as that between RDW and 6MWD is presented in Fig. 3. Spearman’s correlation coefficient for the suspected correlations was 0.271 (p = 0.087) for the correlation between RDW and NT-proBNP (Fig. 3a) and 0.107 (p = 0.560) for the correlation between RDW and 6-min walking distance (Fig. 3b). NT-proBNP, which has been established as reliable diagnostic and prognostic markers in heart failure and a serum indicator for the degree of ventricular dysfunction, tended to have no statistically significant correlation with RDW. In addition, the irregular distribution of 6MWD across RDW levels could also exclude the impact of impaired exercise capacity on RDW. We also calculated Spearman correlation coefficients between RDW and other potential related variables, including hemoglobin (0.118, p = 0.400), mean corpuscular volume (− 0.395, p = 0.056), mean pulmonary artery pressure (0.024, p = 0.864), cardiac index (− 0.141, p = 0.320), and pulmonary vascular resistance (0.139, p = 0.317), which collectively exhibit no significant correlations. According to previous analysis, RDW at diagnosis in patients with pSS-PAH was concluded to be a potential predictor for overall survival and clinical outcomes.
Discussion
In this retrospective cohort study of 55 patients, we investigated the clinical outcomes and overall survival rates in a cohort of Chinese patients with pSS-PAH. Moreover, we confirmed, for the first time, that RDW can serve as a negative prognostic factor of pSS-PAH, in addition to some established predictors such as NT-pro BNP, 6MWD, cardiac function class, etc. In light of the capability to provide robust mortality prediction, the simple and readily available marker could be widely applied in clinical practice and inspire progression on patient management.
pSS is a chronic autoimmune disease, possibly involving different organs and systems along with exocrine glands. Lung involvement is one of the important extra-glandular presentations, in which pulmonary artery involvement is among the most prominent findings [16]. PAH associated with pSS may progress into a fatal outcome by resulting in congestive heart failure, pulmonary edema, arrhythmia, and/or even sudden death. The overall 1-, 3-, and 5-year survival rates calculated in this literature were 98.1, 82.2, and 75.3%, respectively. Several other prior studies have examined survival rates in patients with iPAH. One multicenter research conducted by National Institutes of Health (NIH) Registry from1981 through 1985 show that the median survival was 2.8 years with 1-, 3-, and 5-year survival rates of 68, 48, and 34%, respectively [17]. More recently, French Registry has shed light on the prognosis of patients with iPAH, demonstrating that the survival of patients with PAH has improved compared with the predicted survival based on the NIH Registry, although it still remains suboptimal with 1-, 2-, and 3-year survival of 85.7, 69.5, and 54.9% for incident cases [18]. Despite the great enhancement of survival rates after decades of endeavor, the overall outcome of iPAH patients seems to be still worse than that of pSS-PAH patients, according to findings of this study. One possible explanation for this result is that patients with pSS-PAH tend to screen on cardiopulmonary function through pulmonary function test, ultrasonic cardiography, or RHC and confirm PAH diagnosis at an earlier stage, attributed to onset of symptoms from existing pSS. Besides, these differences in survival may also be due to the standard patient managements in PUMCH, as well as the application of some newly developed targeted medications.
Increased RDW is usually an indicator of ineffective red cell production or hemolysis but has recently been reported to be related to adverse outcomes in cardiovascular and non-cardiovascular disease states [19]. In a prospective cohort without specific classification of pulmonary hypertension, RDW was found to be independently correlated to death and superior to NT-proBNP as a prognostic indicator [20]. Several prior literatures have proved the prognostic significance of NT-pro BNP and 6MWD in iPAH [21, 22]. Almost at the same time, Christopher J Rhodes et al. [4] reported that circulating RDW is related to disease severity and may be used to predict survival in patients with iPAH. Moreover, RDW was identified to add significant prognostic value to measurements of NT-proBNP and exercise capacity and may prove value in a multiple biomarker approach to disease stratification in patients with iPAH in the same study. In an ambulatory cohort of patients with chronic heart failure, baseline and serial increase in RDW was associated with poor long-term outcomes independent of standard cardiac, hematologic, and renal indices [23], although RDW are used to be regarded as a combined presentation of chronic inflammation, dysfunctional erythropoiesis, kidney dysfunction, oxidative stress, and nutritional state [24]. In survival analysis of this study, elevated RDW levels showed a significantly negative relation with clinical outcomes and long-term survival rates. The survival curves intersect twice within approximately 2 years and then diverge, the cause of which is unknown. This phenomenon may reflect the ability of RDW to provide insight into risk for more chronic causes of death that are the culmination of multiple pathophysiologic processes. Besides, those patients who deceased during follow-up have an obviously higher average level of RDW than those who stayed alive, which is conformed to the survival analysis. A hazard rate more than 1.0 shed lights on a negative predictive value of pSS-PAH prognosis. The prognostic value of RDW was independent of 6MWD or NT-pro BNP, based on the insignificant Spearman’s correlation analysis results. Even so, general correlative trends between the 6MWD or NT-pro BNP and RDW levels in pSS-PAH were still shown in this analysis, but without significance. The possible causes of the insignificance could be as follows: (1) the sample size is not large enough; (2) plenty of interfering factors for RDW leads to its variability; (3) continuous elevation in repetitive measurements may be more indicative than single elevation. Although anemia is also a strong prognostic marker in heart failure syndromes, the association between RDW and adverse outcomes of pSS-PAH in our study was independent of baseline hemoglobin and mean corpuscular volume, according to the insignificant difference between the two groups as well as the insignificant Spearman’s correlation analysis results. These findings lead to the identification of RDW as a potential negative predictor of survival in patients with PAH associated with pSS. As part of the complete blood count, RDW is widely available to clinicians and brought no additional costs, thus may be widely applied in clinical practice to provide guidance for patient management.
The mechanisms underlying the association between RDW and adverse outcomes in pSS-PAH patients are not fully understood. However, we still identified some interesting clues which could possibly bring them to light. TLC (total lung capacity) and DLCO (carbon monoxide diffusing capacity), as meaningful parameters reflecting pulmonary function, differed significantly between the two groups with normal and elevated RDW, marking a possible pathologic process of fibrosis in pulmonary interstitial which are usually irreversible and predicts adverse outcome. Besides, in accordance with previous article [25], we observed higher RDW levels in patients with higher NYHA class, showing that decrease in cardiac function may be an underlying contributor to mortality as well. It could be confirmed by a previous Chinese cohort study, revealing that worse cardiac function is a predictor of mortality in patients with pSS-PAH [26]. Impaired exercise capacity or exercise tolerance, a reflection of decrease in cardiac function, was reported to be linked with elevated RDW levels in chronic heart failure patients [27], based on which a speculation that exercise inactivity may have joined the mechanisms causing mortality could be made, even if 6MWD was not significantly different between groups in this study. 6MWD used to be regarded as a simple, safe, noninvasive, reproducible parameter of exercise capacity, but a recent editorial challenged its validity in management of SSc-PAH. Although 6MWD is clearly sensitive to the presence of cardiovascular and pulmonary complications of SSc, such as PAH, SSc patients are also limited by musculoskeletal dysfunction and pain, conclusion of which may improve the status of RDW as a stable index in pSS-PAH management [28]. Meanwhile, an EPIC—Norfolk study claimed that RDW levels were associated with physical inactivity, but this did not influence the RDW-associated risk of heart failure [29]. In addition, elevation of RDW levels was also found to be related with a chronic inflammatory state in patients with heart failure, or even in an unselected patient population, with increased circulating pro-inflammatory cytokines, such as tumor necrosis factor α, interleukin (IL)-1, and IL-6 [30, 31], which may also be a potential factor affecting survival rates in pSS-PAH patients. Qunying Xi et al. [32] pointed out that RDW independently predicts responsiveness of acute pulmonary vasodilator testing in patients with iPAH. Patients with lower RDW levels are prone to have a positive response in acute pulmonary vasodilator testing indicating a greater possibility to benefit from long-term use of calcium channel blocker. Based on these facts, RDW level works to predict a better survival in iPAH patients by aiding selection of more appropriate medical therapy and more delightful responsiveness to medications, and similar principles may also exist in PAH caused by pSS. Furthermore, they also concluded that RDW is associated with disease severity of both iPAH, which may mediate the correlation between RDW levels and the all-cause mortality in patients with iPAH, while another research confirmed the same principle in chronic heart failure [33]. Therefore, it could be reasonably inferred that the reason why RDW levels can be a potential predictor of survival in pSS-PAH patients may be due to the role as a marker of disease severity, waiting for verification in larger populations. As is shown in results, there was no significant association between RDW levels and hemodynamic variables, suggesting that the relation between RDW and death is not simply due to hemodynamic abnormalities in patients with elevated RDW.
As far as we know, this is the first study reporting the correlation between the RDW levels and survival rates for pSS-PAH in a large cohort of patients confirmed by RHC. Primary SS is a common systemic autoimmune disease and pulmonary involvement in pSS consists mainly of small airway disease and ILD. PAH is a rare complication, with few case reports and case series describing the clinical characteristics and survival of patients with pSS-PAH. Since delayed diagnosis and non-standard treatment may account for the comparatively poor outcomes in pSS-PAH, our results highlight a simple and rapid way to assess pSS-PAH patients on their prognosis so they can benefit from advanced treatments. Thus, future studies are needed to predict the prognosis more accurately in patients with pSS-PAH.
There are several limitations of this study. Since PUMCH is a referral center which concentrate on difficult and complicated diseases, a probability of selection bias can hardly be avoided. A considerable number of patients in this study had never been screened for PAH before admission in PUMCH due to non-specific and insidious presentations, resulting in longer disease durations, increased severity of PAH, as well as more adverse outcomes. Moreover, the single-center study in which the cohort was recruited from only PUMCH leaded to the limited sample size. As a consequence, multi-variable Cox analysis cannot be made, since the number of death cases is no more than seven. It is obvious that large-scale, multi-center studies are still required. In conclusion, in this study, we investigate the role RDW plays in the prognosis of pSS-PAH. Our study is the first to describe the correlation between RDW levels and outcomes of patients with pSS-PAH and to identify RDW as a potential negative prognostic factor for pSS-PAH. Further studies are needed to confirm its validity in larger population and develop its function in patient management.
References
Zhao J, Wang Q, Liu Y, Tian Z, Guo X, Wang H, Lai J, Huang C, Yang X, Li M, Zeng X (2017) Clinical characteristics and survival of pulmonary arterial hypertension associated with three major connective tissue diseases: a cohort study in China. Int J Cardiol 236:432–437. https://doi.org/10.1016/j.ijcard.2017.01.097
Rhee RL, Gabler NB, Sangani S, Praestgaard A, Merkel PA, Kawut SM (2015) Comparison of treatment response in idiopathic and connective tissue disease-associated pulmonary arterial hypertension. Am J Respir Crit Care Med 192(9):1111–1117. https://doi.org/10.1164/rccm.201507-1456OC
Pocock SJ, Wang D, Pfeffer MA, Yusuf S, McMurray JJ, Swedberg KB, Ostergren J, Michelson EL, Pieper KS, Granger CB (2006) Predictors of mortality and morbidity in patients with chronic heart failure. Eur Heart J 27(1):65–75. https://doi.org/10.1093/eurheartj/ehi555
Rhodes CJ, Wharton J, Howard LS, Gibbs JS, Wilkins MR (2011) Red cell distribution width outperforms other potential circulating biomarkers in predicting survival in idiopathic pulmonary arterial hypertension. Heart 97(13):1054–1060. https://doi.org/10.1136/hrt.2011.224857
Bhambhani K, Aronow R (1990) Lead poisoning and thalassemia trait or iron deficiency. The value of the red blood cell distribution width. American journal of diseases of children (1960) 144(11):1231–1233
van Zeben D, Bieger R, van Wermeskerken RK, Castel A, Hermans J (1990) Evaluation of microcytosis using serum ferritin and red blood cell distribution width. Eur J Haematol 44(2):106–109
He W, Jia J, Chen J, Qin S, Tao H, Kong Q, Xue Q, Zhang D (2014) Comparison of prognostic value of red cell distribution width and NT-proBNP for short-term clinical outcomes in acute heart failure patients. Int Heart J 55(1):58–64
Nunez J, Nunez E, Rizopoulos D, Minana G, Bodi V, Bondanza L, Husser O, Merlos P, Santas E, Pascual-Figal D, Chorro FJ, Sanchis J (2014) Red blood cell distribution width is longitudinally associated with mortality and anemia in heart failure patients. Circulation journal : official journal of the Japanese Circulation Society 78(2):410–418
van Kimmenade RR, Mohammed AA, Uthamalingam S, van der Meer P, Felker GM, Januzzi JL Jr (2010) Red blood cell distribution width and 1-year mortality in acute heart failure. Eur J Heart Fail 12(2):129–136. https://doi.org/10.1093/eurjhf/hfp179
Montagnana M, Cervellin G, Meschi T, Lippi G (2011) The role of red blood cell distribution width in cardiovascular and thrombotic disorders. Clin Chem Lab Med 50(4):635–641. https://doi.org/10.1515/cclm.2011.831
Ozsu S, Ozcelik N, Oztuna F, Ozlu T (2015) Prognostic value of red cell distribution width in patients with sarcoidosis. Clin Respir J 9(1):34–38. https://doi.org/10.1111/crj.12101
Seyhan EC, Ozgul MA, Tutar N, Omur I, Uysal A, Altin S (2013) Red blood cell distribution and survival in patients with chronic obstructive pulmonary disease. Copd 10(4):416–424. https://doi.org/10.3109/15412555.2012.758697
Zhao J, Mo H, Guo X, Wang Q, Xu D, Hou Y, Tian Z, Liu Y, Wang H, Lai J, Li M, Zeng X (2018) Red blood cell distribution width as a related factor of pulmonary arterial hypertension in patients with systemic sclerosis. Clin Rheumatol 37(4):979–985. https://doi.org/10.1007/s10067-017-3918-9
Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RI, Kassan SS, Pillemer SR, Talal N, Weisman MH (2002) Classification criteria for Sjogren's syndrome: a revised version of the European criteria proposed by the American-European consensus group. Ann Rheum Dis 61(6):554–558
Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, Ghofrani A, Gomez Sanchez MA, Hansmann G, Klepetko W, Lancellotti P, Matucci M, McDonagh T, Pierard LA, Trindade PT, Zompatori M, Hoeper M (2015) 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the joint task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J 46(4):903–975. https://doi.org/10.1183/13993003.01032-2015
Kobak S, Kalkan S, Kirilmaz B, Orman M, Ercan E (2014) Pulmonary arterial hypertension in patients with primary Sjogren's syndrome. Autoimmune diseases 2014:710401–710405. https://doi.org/10.1155/2014/710401
D'Alonzo GE, Barst RJ, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, Fishman AP, Goldring RM, Groves BM, Kernis JT et al (1991) Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med 115(5):343–349
Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, Yaici A, Weitzenblum E, Cordier JF, Chabot F, Dromer C, Pison C, Reynaud-Gaubert M, Haloun A, Laurent M, Hachulla E, Cottin V, Degano B, Jais X, Montani D, Souza R, Simonneau G (2010) Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation 122(2):156–163. https://doi.org/10.1161/circulationaha.109.911818
Yang T, Sun YJ, Xiong CM, Zeng WJ, Ni XH, Zhao ZH, Liu ZH, Gu Q, He JG (2014) Red blood cell distribution width predicts survival in patients with Eisenmenger syndrome. Clin Chem Lab Med 52(5):743–750. https://doi.org/10.1515/cclm-2013-0747
Hampole CV, Mehrotra AK, Thenappan T, Gomberg-Maitland M, Shah SJ (2009) Usefulness of red cell distribution width as a prognostic marker in pulmonary hypertension. Am J Cardiol 104(6):868–872. https://doi.org/10.1016/j.amjcard.2009.05.016
Casserly B, Klinger JR (2009) Brain natriuretic peptide in pulmonary arterial hypertension: biomarker and potential therapeutic agent. Drug design, development and therapy 3:269–287
Golpe R, Castro-Anon O, Perez-de-Llano LA, Gonzalez-Juanatey C, Muniz-Fernandez C, Testa-Fernandez A, Perez-Fernandez R (2014) Prognostic significance of six-minute walk test in non-group 1 pulmonary hypertension. Heart & lung : the journal of critical care 43(1):72–76. https://doi.org/10.1016/j.hrtlng.2013.08.007
Cauthen CA, Tong W, Jain A, Tang WH (2012) Progressive rise in red cell distribution width is associated with disease progression in ambulatory patients with chronic heart failure. J Card Fail 18(2):146–152. https://doi.org/10.1016/j.cardfail.2011.10.013
Forhecz Z, Gombos T, Borgulya G, Pozsonyi Z, Prohaszka Z, Janoskuti L (2009) Red cell distribution width in heart failure: prediction of clinical events and relationship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. Am Heart J 158(4):659–666. https://doi.org/10.1016/j.ahj.2009.07.024
Holmstrom A, Sigurjonsdottir R, Hammarsten O, Gustafsson D, Petzold M, Fu ML (2012) Red blood cell distribution width and its relation to cardiac function and biomarkers in a prospective hospital cohort referred for echocardiography. European journal of internal medicine 23(7):604–609. https://doi.org/10.1016/j.ejim.2012.05.005
Liu Z, Yang X, Tian Z, Qian J, Wang Q, Zhao J, Huang C, Liu Y, Guo X, Wang H, Lai J, Li M, Zhao Y, Zeng X (2018) The prognosis of pulmonary arterial hypertension associated with primary Sjogren's syndrome: a cohort study. Lupus 961203318756287:1072–1080. https://doi.org/10.1177/0961203318756287
Van Craenenbroeck EM, Pelle AJ, Beckers PJ, Possemiers NM, Ramakers C, Vrints CJ, Van Hoof V, Denollet J, Conraads VM (2012) Red cell distribution width as a marker of impaired exercise tolerance in patients with chronic heart failure. Eur J Heart Fail 14(1):54–60. https://doi.org/10.1093/eurjhf/hfr136
Pamidi S, Mehta S (2009) Six-minute walk test in scleroderma-associated pulmonary arterial hypertension: are we counting what counts? J Rheumatol 36(2):216–218. https://doi.org/10.3899/jrheum.081243
Emans ME, Gaillard CA, Pfister R, Tanck MW, Boekholdt SM, Wareham NJ, Khaw KT (2013) Red cell distribution width is associated with physical inactivity and heart failure, independent of established risk factors, inflammation or iron metabolism; the EPIC-Norfolk study. Int J Cardiol 168(4):3550–3555. https://doi.org/10.1016/j.ijcard.2013.05.002
Inuzuka R, Abe J (2015) Red blood cell distribution width as a link between ineffective erythropoiesis and chronic inflammation in heart failure. Circulation journal : official journal of the Japanese Circulation Society 79(5):974–975. https://doi.org/10.1253/circj.CJ-15-0254
Lippi G, Targher G, Montagnana M, Salvagno GL, Zoppini G, Guidi GC (2009) Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients. Archives of pathology & laboratory medicine 133(4):628–632. https://doi.org/10.1043/1543-2165-133.4.628
Xi Q, Liu Z, Zhao Z, Luo Q (2015) Red blood cell distribution width predicts responsiveness of acute pulmonary vasodilator testing in patients with idiopathic pulmonary arterial hypertension. Clinica chimica acta; international journal of clinical chemistry 446:272–276. https://doi.org/10.1016/j.cca.2015.04.041
Liu S, Wang P, Shen PP, Zhou JH (2016) Predictive values of red blood cell distribution width in assessing severity of chronic heart failure. Medical science monitor : international medical journal of experimental and clinical research 22:2119–2125
Funding
This study was supported by the Chinese National Key Research R&D Program (2017YFC0907601, 2017YFC0907605).
Author information
Authors and Affiliations
Contributions
Min Hui, Jiuliang Zhao, and Zhuang Tian were the authors who contributed to interpretation of data, completed drafting of the article, and revised it critically.
Jieying Wang was in charge of original data collection for forming the entire cohort.
Junyan Qian and Xiaoxi Yang contributed to the basic conception and the design of the retrospective cohort study.
Qian Wang, Mengtao Li, Yan Zhao, and Xiaofeng Zeng did a lot for reading and the approval of final version. Xiaofeng Zeng and Yan Zhao were both the correspondence authors of this manuscript.
Corresponding authors
Ethics declarations
This study was approved by the medical ethics committee of PUMCH and was conducted in compliance with the ethics committee requirements. The ethical approval number is S-191.
ᅟ
Disclosures
None.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hui, M., Zhao, J., Tian, Z. et al. Red blood cell distribution width as a potential predictor of survival of pulmonary arterial hypertension associated with primary Sjogren’s syndrome: a retrospective cohort study. Clin Rheumatol 38, 477–485 (2019). https://doi.org/10.1007/s10067-018-4281-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4281-1