Abstract
Purpose
The aim of the present study was to evaluate the effect of the anesthesia type on the postoperative quality of life in patients who underwent trans-abdominal pre-peritoneal (TAPP) inguinal hernia repair.
Methods
In this study, 70 patients submitted to TAPP for inguinal hernia repair, were randomized between spinal and general anesthesia. Overall, 58 patients completed the follow-up process and were, therefore, included. The quality of life evaluation was based on the SF-36 questionnaire. Significance was considered at the level of P < 0.05
Results
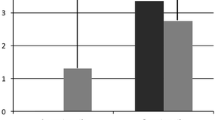
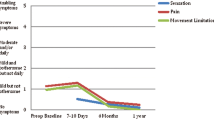
General anesthesia was applied to 31 patients, whereas 27 operations were performed under spinal anesthesia. Except gender, the two study subgroups were similar in terms of demographics. Although spinal anesthesia displayed higher energy, emotional health, and general health scores these findings were not statistically significant. A positive correlation was identified between age and physical and emotional role. Operative time was associated with the estimated energy and general health.
Conclusion
Our study could not identify a difference between spinal and general anesthesia on the postoperative quality of life. Spinal anesthesia is as effective as general anesthesia and remains an attractive anesthetic alternative for TAPP inguinal hernia repair. Given several study limitations, further high-quality trials are required.

Similar content being viewed by others
References
Gutlic N, Gutlic A, Petersson U et al (2019) Randomized clinical trial comparing total extraperitoneal with Lichtenstein inguinal hernia repair (TEPLICH trial). Br J Surg 106:845–855. https://doi.org/10.1002/bjs.11230
Fortelny RH, Schwab R, Glaser KS et al (2008) The assessment of quality of life in a trial on lightweight mesh fixation with fibrin sealant in transabdominal preperitoneal hernia repair. Hernia 12:499–505. https://doi.org/10.1007/s10029-008-0365-1
Georgiou E, Schoina E, Markantonis S-L et al (2018) Laparoscopic total extraperitoneal inguinal hernia repair: retrospective study on prosthetic materials, postoperative management, and quality of life. Medicine (Baltimore) 97:e13974. https://doi.org/10.1097/MD.0000000000013974
Quail J, Spence D, Hannon M (2017) Perioperative gabapentin improves patient-centered outcomes after inguinal hernia repair. Mil Med 182:e2052–e2055. https://doi.org/10.7205/MILMED-D-17-00107
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Myers E, Browne KM, Kavanagh DO, Hurley M (2010) Laparoscopic (TEP) versus lichtenstein inguinal hernia repair: a comparison of quality-of-life outcomes. World J Surg 34:3059–3064. https://doi.org/10.1007/s00268-010-0730-y
Isil RG, Avlanmis O (2020) Effects of totally extraperitoneal and lichtenstein hernia repair on men’s sexual function and quality of life. Surg Endosc 34:1103–1111. https://doi.org/10.1007/s00464-019-06857-0
Wei FX, Zhang YC, Han W et al (2015) Transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) for laparoscopic hernia repair: a meta-analysis. Surg Laparosc Endosc Percutan Tech 25:375–383. https://doi.org/10.1097/SLE.0000000000000123
Aiolfi A, Cavalli M, Micheletto G et al (2019) Primary inguinal hernia: systematic review and Bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia 23:473–484. https://doi.org/10.1007/s10029-019-01964-2
Sarakatsianou C, Georgopoulou S, Baloyiannis I et al (2017) Spinal versus general anesthesia for transabdominal preperitoneal (TAPP) repair of inguinal hernia: interim analysis of a controlled randomized trial. Am J Surg 214:239–245. https://doi.org/10.1016/j.amjsurg.2017.01.032
Bansal VK, Krishna A, Manek P et al (2017) A prospective randomized comparison of testicular functions, sexual functions and quality of life following laparoscopic totally extra-peritoneal (TEP) and trans-abdominal pre-peritoneal (TAPP) inguinal hernia repairs. Surg Endosc 31:1478–1486. https://doi.org/10.1007/s00464-016-5142-0
Drissi F, Jurczak F, Cossa JP et al (2018) Outpatient groin hernia repair: assessment of 9330 patients from the French “Club Hernie” database. Hernia 22:427–435. https://doi.org/10.1007/s10029-017-1689-5
Chen TH, Li L, Kochen MM (2005) A systematic review: how to choose appropriate health-related quality of life (HRQOL) measures in routine general practice? J Zhejiang Univ Sci B 6:936–940
Sarakatsianou C, Georgopoulou S, Tzovaras G et al (2019) Hemodynamic effects of anesthesia type in patients undergoing laparoscopic transabdominal preperitoneal inguinal hernia repair under spinal vs general anesthesia. Hernia. https://doi.org/10.1007/s10029-018-01874-9
Rosenberg J, Bisgaard T, Kehlet H et al (2011) Danish Hernia Database recommendations for the management of inguinal and femoral hernia in adults. Dan Med Bull 58:C4243
Li L, Pang Y, Wang Y et al (2020) Comparison of spinal anesthesia and general anesthesia in inguinal hernia repair in adult: a systematic review and meta-analysis. BMC Anesthesiol 20:64. https://doi.org/10.1186/s12871-020-00980-5
Eizaga Rebollar R, García Palacios MV, Morales Guerrero J, Torres Morera LM (2018) Spinal anesthesia for pediatric laparoscopic hernia repair: a case report. A&A Pract 11:293–295. https://doi.org/10.1213/XAA.0000000000000810
Hajibandeh S, Hajibandeh S, Mobarak S et al (2020) Meta-analysis of spinal anesthesia versus general anesthesia during laparoscopic total extraperitoneal repair of inguinal hernia. Surg Laparosc Endosc Percutan Tech. https://doi.org/10.1097/SLE.0000000000000783
Bökkerink WJVW, Persoon AMA, Akkersdijk WLW et al (2017) The TREPP as alternative technique for recurrent inguinal hernia after Lichtenstein’s repair: a consecutive case series. Int J Surg 40:73–77. https://doi.org/10.1016/j.ijsu.2017.02.022
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Pappa E, Kontodimopoulos N, Niakas D (2005) Validating and norming of the Greek SF-36 Health Survey. Qual Life Res 14:1433–1438. https://doi.org/10.1007/s11136-004-6014-y
Hedberg HM, Hall T, Gitelis M et al (2018) Quality of life after laparoscopic totally extraperitoneal repair of an asymptomatic inguinal hernia. Surg Endosc 32:813–819. https://doi.org/10.1007/s00464-017-5748-x
Krpata DM, Schmotzer BJ, Flocke S et al (2012) Design and initial implementation of HerQLes: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 215:635–642. https://doi.org/10.1016/j.jamcollsurg.2012.06.412
Zhang R, Zhu ZJ, Sun LY (2018) Application of pediatric donor livers after circulatory death in adult liver transplantation: a single-center experience. Exp Clin Transpl 16:575–581. https://doi.org/10.6002/ect.2017.0358
Rogmark P, Petersson U, Bringman S et al (2016) Quality of life and surgical outcome 1 year after open and laparoscopic incisional hernia repair: PROLOVE: a randomized controlled trial. Ann Surg 263:244–250. https://doi.org/10.1097/SLA.0000000000001305
Wennergren JE, Plymale M, Davenport D et al (2016) Quality-of-life scores in laparoscopic preperitoneal inguinal hernia repair. Surg Endosc 30:3467–3473. https://doi.org/10.1007/s00464-015-4631-x
Gong W, Li J (2018) Operation versus watchful waiting in asymptomatic or minimally symptomatic inguinal hernias: the meta-analysis results of randomized controlled trials. Int J Surg 52:120–125. https://doi.org/10.1016/j.ijsu.2018.02.030
Ismail M, Garg P (2009) Laparoscopic inguinal total extraperitoneal hernia repair under spinal anesthesia without mesh fixation in 1,220 hernia repairs. Hernia 13:115–119. https://doi.org/10.1007/s10029-008-0442-5
Patterson TJ, Beck J, Currie PJ et al (2019) Meta-analysis of patient-reported outcomes after laparoscopic versus open inguinal hernia repair. Br J Surg 106:824–836. https://doi.org/10.1002/bjs.11139
Bullen NL, Massey LH, Antoniou SA et al (2019) Open versus laparoscopic mesh repair of primary unilateral uncomplicated inguinal hernia: a systematic review with meta-analysis and trial sequential analysis. Hernia 23:461–472. https://doi.org/10.1007/s10029-019-01989-7
Yildirim D, Hut A, Uzman S et al (2017) Spinal anesthesia is safe in laparoscopic total extraperitoneal inguinal hernia repair. A retrospective clinical trial. Wideochirurg Tech Maloinwazyjne 12:417–427. https://doi.org/10.5114/wiitm.2017.72325
Bansal VK, Misra MC, Babu D et al (2013) A prospective, randomized comparison of long-term outcomes: chronic groin pain and quality of life following totally extraperitoneal (TEP) and transabdominal preperitoneal (TAPP) laparoscopic inguinal hernia repair. Surg Endosc 27:2373–2382. https://doi.org/10.1007/s00464-013-2797-7
Wright D, Paterson C, Scott N et al (2002) Five-year follow-up of patients undergoing laparoscopic or open groin hernia repair: a randomized controlled trial. Ann Surg 235:333–337. https://doi.org/10.1097/00000658-200203000-00004
Arnold MR, Coakley KM, Fromke EJ et al (2019) Long-term assessment of surgical and quality-of-life outcomes between lightweight and standard (heavyweight) three-dimensional contoured mesh in laparoscopic inguinal hernia repair. Surgery 165:820–824. https://doi.org/10.1016/j.surg.2018.10.016
Dhankhar DS, Sharma N, Mishra T et al (2014) Totally extraperitoneal repair under general anesthesia versus Lichtenstein repair under local anesthesia for unilateral inguinal hernia: a prospective randomized controlled trial. Surg Endosc 28:996–1002. https://doi.org/10.1007/s00464-013-3269-9
Ladurner R, Chiapponi C, Linhuber Q, Mussack T (2011) Long term outcome and quality of life after open incisional hernia repair–light versus heavy weight meshes. BMC Surg 11:25. https://doi.org/10.1186/1471-2482-11-25
Donati M, Brancato G, Grosso G et al (2016) Immunological reaction and oxidative stress after light or heavy polypropylene mesh implantation in inguinal hernioplasty. Medicine (Baltimore) 95:e3791. https://doi.org/10.1097/MD.0000000000003791
Rutegård M, Gümüsçü R, Stylianidis G et al (2018) Chronic pain, discomfort, quality of life and impact on sex life after open inguinal hernia mesh repair: an expertise-based randomized clinical trial comparing lightweight and heavyweight mesh. Hernia 22:411–418. https://doi.org/10.1007/s10029-018-1734-z
Li W, Sun D, Sun Y et al (2017) The effect of transabdominal preperitoneal (TAPP) inguinal hernioplasty on chronic pain and quality of life of patients: mesh fixation versus non-fixation. Surg Endosc 31:4238–4243. https://doi.org/10.1007/s00464-017-5485-1
Langbach O, Bukholm I, Benth JŠ, Røkke O (2016) Long-term quality of life and functionality after ventral hernia mesh repair. Surg Endosc 30:5023–5033. https://doi.org/10.1007/s00464-016-4850-9
Licari L, Guercio G, Campanella S et al (2019) Clinical and functional outcome after abdominal wall incisional hernia repair: evaluation of quality-of-life improvement and comparison of assessment scales. World J Surg 43:1914–1920. https://doi.org/10.1007/s00268-019-05003-0
Lawrence K, McWhinnie D, Jenkinson C, Coulter A (1997) Quality of life in patients undergoing inguinal hernia repair. Ann R Coll Surg Engl 79:40–45
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Institution Ethis Commitee with the registration number of UTH5535/12/11.
Statement of human and animal rights
The research was conducted according to the principles of the World Medical Association Declaration of Helsinki “Ethical principles for Medical Research Involving Human Subjects”.
Informed consent
Patients were informed in detail and inform consent was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sarakatsianou, C., Baloyiannis, I., Perivoliotis, K. et al. Quality of life after laparoscopic trans-abdominal pre-peritoneal inguinal hernia repair: spinal vs general anesthesia. Hernia 25, 789–796 (2021). https://doi.org/10.1007/s10029-020-02313-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02313-4