Abstract
Introduction
Evidence is needed to justify whether investment in an internationally agreed core outcome set for inguinal hernia surgery is needed. This study aimed to assess outcome reporting from randomised controlled trials (RCTs) and meta-analyses in inguinal hernia surgery.
Methods
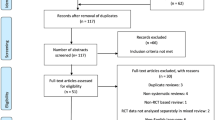
RCTs and meta-analyses comparing surgical technique or mesh type for primary inguinal hernia repair were systematically identified. Verbatim details, type, frequency and definition of clinician-observed and -assessed outcomes were summarised. Patient-reported outcome measures (PROMs) were analysed for instrument validity and frequency of domain reporting.
Results
40 RCTs (10,810 patients) and 7 meta-analyses (17,280 patients) were identified. No single PROM was reported by all studies. There were 58 different clinician-observed outcomes, with recurrence (n = 47, 100 %), wound infection (n = 33, 70.2 %), haematoma (n = 31, 77.5 %) and seroma formation (n = 22, 46.8 %) being most frequently reported. All studies measured patients’ views, although only 12 (30.0 %) used validated instruments. The SF36 was the most commonly used multi-dimensional valid PROM (n = 7), and a visual analogue scale assessing pain (n = 32) was the most frequently used unidimensional scale. Non-validated questionnaires assessed 25 other aspects of patients’ health. Two meta-analyses defined recurrence and three chronic pain although neither ensured that included RCTs adhered to the definitions.
Conclusions
Outcome reporting from RCTs concerning inguinal hernia repair is inconsistent and poorly defined, limiting meta-analyses, which themselves do not control for the differing definitions of assessed outcomes. This study justifies investment in a standardised core outcome set for inguinal hernia surgery, to improve outcome reporting and evidence synthesis.



Similar content being viewed by others
References
Rutkow IM (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am 83:1045–51, v–vi
Hospital Episode Statistics. Admitted Patient Care-England 2011–2012. Total procedures and interventions. http://www.hscic.gov.uk/catalogue/PUB08288/hosp-epis-stat-admi-tot-ops-11-12-tab.xls. Accessed Aug 2013
Sajid MS, Leaver C, Baig MK et al (2012) Systematic review and meta-analysis of the use of lightweight versus heavyweight mesh in open inguinal hernia repair. Br J Surg 99:29–37
O’Reilly EA, Burke JP, O’Connell PR (2012) A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg 255:846–853
McCormack K, Scott NW, Go PM et al (2003) Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev CD001785
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Eklund A, Montgomery A, Bergkvist L et al (2010) Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. Br J Surg 97:600–608
Moher D, Hopewell S, Schulz KF et al (2010) CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 63:e1–e37
Williamson P, Clarke M (2012) The COMET (Core Outcome Measures in Effectiveness Trials) Initiative: its role in improving Cochrane reviews. Cochrane Database Syst Rev 5:ED000041
Zhao G, Gao P, Ma B et al (2009) Open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Ann Surg 250:35–42
Teng YJ, Pan SM, Liu YL et al (2011) A meta-analysis of randomized controlled trials of fixation versus nonfixation of mesh in laparoscopic total extraperitoneal inguinal hernia repair. Surg Endosc 25:2849–2858
Gao M, Han J, Tian J et al (2010) Vypro II mesh for inguinal hernia repair: a meta analysis of randomized controlled trials. Ann Surg 251:838–842
Amato B, Moja L, Panico S et al (2014) Shouldice technique versus other open techniques for inguinal hernia repair. Cochrane Database Syst Rev 4:CD001543
Tam KW, Liang HH, Chai CY (2010) Outcomes of staple fixation of mesh versus nonfixation in laparoscopic total extraperitoneal inguinal repair: a meta-analysis of randomized controlled trials. World J Surg 34:3065–3074
Markar SR, Karthikesalingam A, Alam F et al (2010) Partially or completely absorbable versus nonabsorbable mesh repair for inguinal hernia: a systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech 20:213–219
Kucuk HF, Sikar HE, Kurt N et al (2010) Lichtenstein or darn procedure in inguinal hernia repair: a prospective randomized comparative study. Hernia 14:357–360
Langeveld HR, van’t Riet M, Weidema WF et al (2010) Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial): a randomized controlled trial. Ann Surg 251:819–24
Ansaloni L, Catena F, Coccolini F et al (2009) Inguinal hernia repair with porcine small intestine submucosa: 3-year follow-up results of a randomized controlled trial of Lichtenstein’s repair with polypropylene mesh versus Surgisis Inguinal Hernia Matrix. Am J Surg 198:303–312
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Testini M, Lissidini G, Poli E et al (2010) A single-surgeon randomized trial comparing sutures, N-butyl-2-cyanoacrylate and human fibrin glue for mesh fixation during primary inguinal hernia repair. Can J Surg pp 155–60
Peeters E, Spiessens C, Oyen R et al (2010) Laparoscopic inguinal hernia repair in men with lightweight meshes may significantly impair sperm motility: a randomized controlled trial. Ann Surg 252:240–246
Sadowski B, Rodriguez J, Symmonds R et al (2011) Comparison of polypropylene versus polyester mesh in the Lichtenstein hernia repair with respect to chronic pain and discomfort. Hernia 15:643–654
Bhangu A, Fletcher L, Kingdon S et al (2012) A clinical and radiological assessment of incisional hernias following closure of temporary stomas. Surgeon 10:321–325
Bay-Nielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study. Ann Surg 233:1–7
Franneby U, Gunnarsson U, Andersson M et al (2008) Validation of an Inguinal Pain Questionnaire for assessment of chronic pain after groin hernia repair. Br J Surg 95:488–493
Nienhuijs S, Staal E, Keemers-Gels M et al (2007) Pain after open preperitoneal repair versus Lichtenstein repair: a randomized trial. World J Surg 31:1751–1757
Kaafarani HM, Hur K, Campasano M et al (2010) Classification and valuation of postoperative complications in a randomized trial of open versus laparoscopic ventral herniorrhaphy. Hernia 14:231–235
Bruce J, Russell EM, Mollison J et al (2001) The quality of measurement of surgical wound infection as the basis for monitoring: a systematic review. J Hosp Infect 49:99–108
Mangram AJ, Horan TC, Pearson ML et al (1999) Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 27:97–132
Bruce J, Krukowski ZH, Al-Khairy G et al (2001) Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br J Surg 88:1157–1168
Blencowe NS, Strong S, McNair AG et al (2012) Reporting of short-term clinical outcomes after esophagectomy: a systematic review. Ann Surg 255:658–666
Whistance RN, Forsythe RO, McNair AG et al (2013) A systematic review of outcome reporting in colorectal cancer surgery. Colorectal Dis 15:e548–e560
Kirkham JJ, Dwan KM, Altman DG et al (2010) The impact of outcome reporting bias in randomised controlled trials on a cohort of systematic reviews. BMJ 340:c365
Wong JU, Leung TH, Huang CC et al (2011) Comparing chronic pain between fibrin sealant and suture fixation for bilayer polypropylene mesh inguinal hernioplasty: a randomized clinical trial. Am J Surg 202:34–38
Harjai MNB, Singh P, Singh Y (2007) A prospective randomized controlled study of Lichtenstein’s tension free versus modified Bassini repair in the management of groin hernias. Med J Armed Forces India 63:40–43
Pokorny H, Klingler A, Schmid T et al (2008) Recurrence and complications after laparoscopic versus open inguinal hernia repair: results of a prospective randomized multicenter trial. Hernia 12:385–389
Chui LB, Ng WT, Sze YS et al (2010) Prospective, randomized, controlled trial comparing lightweight versus heavyweight mesh in chronic pain incidence after TEP repair of bilateral inguinal hernia. Surg Endosc 24:2735–2738
Testini M, Lissidini G, Poli E et al (2010) A single-surgeon randomized trial comparing sutures, N-butyl-2-cyanoacrylate and human fibrin glue for mesh fixation during primary inguinal hernia repair. Can J Surg 53:155–160
Boldo E, Armelles A, Perez de Lucia G et al (2008) Pain after laparoscopic bilateral hernioplasty: early results of a prospective randomized double-blind study comparing fibrin versus staples. Surg Endosc 22:1206–1209
Agarwal BB, Agarwal KA, Mahajan KC (2009) Prospective double-blind randomized controlled study comparing heavy- and lightweight polypropylene mesh in totally extraperitoneal repair of inguinal hernia: early results. Surg Endosc 23:242–247
Dalenback J, Andersson C, Anesten B et al (2009) Prolene hernia system, Lichtenstein mesh and plug-and-patch for primary inguinal hernia repair: 3-year outcome of a prospective randomised controlled trial. The BOOP study: bi-layer and connector, on-lay, and on-lay with plug for inguinal hernia repair. Hernia 13:121–129 (discussion 231)
Gunal O, Ozer S, Gurleyik E et al (2007) Does the approach to the groin make a difference in hernia repair? Hernia 11:429–434
Al-Saiegh AA-SR, Al-Khassaki H (2009) Tension-free inguinal hernia repair comparing ‘mesh’ with ‘darn’ a prospective randomized clinical trial. Iraqi Postgrad Med J 8:220–227
Sanders DL, Samarakoon DH, Ganshirt SW et al (2009) A two-centre blinded randomised control study comparing the Lichtenstein patch, Perfix plug and ProLoop plug in the repair of primary inguinal hernia. Hernia 13:499–503
Chauhan A, Tiwari S, Gupta A (2007) Study of efficacy of bilayer mesh device versus conventional polypropylene hernia system in inguinal hernia repair: early results. World J Surg 31:1356–1359 (discussion 1360–1)
Langenbach MR, Schmidt J, Ubrig B et al (2008) Sixty-month follow-up after endoscopic inguinal hernia repair with three types of mesh: a prospective randomized trial. Surg Endosc 22:1790–1797
Hamza Y, Gabr E, Hammadi H et al (2010) Four-arm randomized trial comparing laparoscopic and open hernia repairs. Int J Surg 8:25–28
Kapischke M, Schulze H, Caliebe A (2010) Self-fixating mesh for the Lichtenstein procedure: a prestudy. Langenbecks Arch Surg 395:317–322
Torcivia A, Vons C, Barrat C et al (2011) Influence of mesh type on the quality of early outcomes after inguinal hernia repair in ambulatory setting controlled study: Glucamesh(R) vs Polypropylene(R). Langenbecks Arch Surg 396:173–178
Bender O, Balci FL, Yuney E et al (2009) Systemic inflammatory response after Kugel versus laparoscopic groin hernia repair: a prospective randomized trial. Surg Endosc 23:2657–2661
Kaynak B, Celik F, Guner A et al (2007) Moloney darn repair versus Lichtenstein mesh hernioplasty for open inguinal hernia repair. Surg Today 37:958–960
Smietanski M, Bury K, Smietanska IA et al (2011) Five-year results of a randomised controlled multi-centre study comparing heavy-weight knitted versus low-weight, non-woven polypropylene implants in Lichtenstein hernioplasty. Hernia 15:495–501
Frey DM, Wildisen A, Hamel CT et al (2007) Randomized clinical trial of Lichtenstein’s operation versus mesh plug for inguinal hernia repair. Br J Surg 94:36–41
Bektas H, Bilsel Y, Ersoz F et al (2011) Comparison of totally extraperitoneal technique and darn plication of primary inguinal hernia. J Laparoendosc Adv Surg Tech 21:583–588
Koch A, Bringman S, Myrelid P et al (2008) Randomized clinical trial of groin hernia repair with titanium-coated lightweight mesh compared with standard polypropylene mesh. Br J Surg 95:1226–1231
Nikkolo C, Lepner U, Murruste M et al (2010) Randomised clinical trial comparing lightweight mesh with heavyweight mesh for inguinal hernioplasty. Hernia 14:253–258
Chowbey PK, Garg N, Sharma A et al (2010) Prospective randomized clinical trial comparing lightweight mesh and heavyweight polypropylene mesh in endoscopic totally extraperitoneal groin hernia repair. Surg Endosc 24:3073–3079
Smietanski M (2008) Randomized clinical trial comparing a polypropylene with a poliglecaprone and polypropylene composite mesh for inguinal hernioplasty. Br J Surg 95:1462–1468
Gong K, Zhang N, Lu Y et al (2011) Comparison of the open tension-free mesh-plug, transabdominal preperitoneal (TAPP), and totally extraperitoneal (TEP) laparoscopic techniques for primary unilateral inguinal hernia repair: a prospective randomized controlled trial. Surg Endosc 25:234–239
Lovisetto F, Zonta S, Rota E et al (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg 245:222–231
Butters M, Redecke J, Koninger J (2007) Long-term results of a randomized clinical trial of Shouldice, Lichtenstein and transabdominal preperitoneal hernia repairs. Br J Surg 94:562–565
Fortelny RH, Petter-Puchner AH, May C et al (2012) The impact of atraumatic fibrin sealant vs. staple mesh fixation in TAPP hernia repair on chronic pain and quality of life: results of a randomized controlled study. Surg Endosc 26:249–254
Prieto-Diaz-Chavez E, Medina-Chavez JL, Anaya-Prado R (2009) A cost-effectiveness analysis of tension-free versus Shouldice inguinal hernia repair: a randomized double-blind clinical trial. Hernia 13:233–238
van Veen RN, Wijsmuller AR, Vrijland WW et al (2007) Long-term follow-up of a randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg 94:506–510
Berndsen FH, Petersson U, Arvidsson D et al (2007) Discomfort five years after laparoscopic and Shouldice inguinal hernia repair: a randomised trial with 867 patients. A report from the SMIL study group. Hernia 11:307–313
Eklund AS, Montgomery AK, Rasmussen IC et al (2009) Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair: a randomized, multicenter trial with 5-year follow-up. Ann Surg 249:33–38
Garg P, Nair S, Shereef M et al (2011) Mesh fixation compared to nonfixation in total extraperitoneal inguinal hernia repair: a randomized controlled trial in a rural center in India. Surg Endosc 25:3300–3306
Conflict of interest
AB declares no conflict of interest.
PS declares no conflict of interest.
TP declares no conflict of interest.
JMB declares no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhangu, A., Singh, P., Pinkney, T. et al. A detailed analysis of outcome reporting from randomised controlled trials and meta-analyses of inguinal hernia repair. Hernia 19, 65–75 (2015). https://doi.org/10.1007/s10029-014-1299-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-014-1299-4