Abstract
Background
The utilization of mesh reinforcement of the inguinal area with polypropylene mesh has increased drastically over the last decade. Infertility due to obstructive azoospermia is a rare but serious complication following inguinal hernia repair, especially in young patients. The aim of this study was to evaluate the effect of different mesh structures on integrity of the vas deferens.
Materials and methods
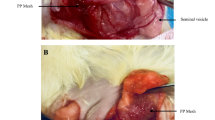
Twenty male Chinchilla rabbits were used. The spermatic cord was dissected free and a Lichtenstein repair was performed with a low-weight polypropylene mesh (UltraPro®) and a heavy-weight polypropylene mesh (Prolene®) on the contralateral side. A vasography was performed after six months in order to investigate obstructions of the vas deferens. Light microscopy of the mesh host tissue interface was also performed and the foreign body reaction analyzed. Spermatogenesis was evaluated using the Johnsen score.
Results
Vasography revealed relevant obstructions (>75% of lumen diameter) located at the mesh margins (50% of Prolene® and 22.2% of UltraPro® mesh samples). Microscopic investigation of the mesh–host tissue interface showed typical formation of foreign body granulomas. The diameters of the foreign body granulomas were significantly reduced in the UltraPro® mesh group (41.7 ± 5.5 μm) compared to the Prolene® mesh group (48.7 ± 7.7 μm). Upon investigating the percentages of apoptotic (TUNEL) and proliferating (Ki67) cells, no significant differences were found. Following Prolene® mesh implantation, a mean Johnsen score of 9.1 ± 1.2 was estimated, which was not significantly different from the UltraPro® mesh samples (8.9 ± 1.4, P > 0.05).
Conclusions
If a mesh material is needed for inguinal hernia repair in young patients, the use of modern low-weight large porous and elastic samples appears to have a beneficial effect on integrity of the vas deferens.



Similar content being viewed by others
References
Rutkow IM, Robbins AW (1993) Demographic, classificatory, and socioeconomic aspects of hernia repair in the United States. Surg Clin North Am 73:413–426
Peiper C, Klinge U, Junge K, Schumpelick V (2002) Meshes in inguinal hernia repair. Zentralbl Chir 127:573–577
Klosterhalfen B, Klinge U, Schumpelick V (1998) Functional and morphological evaluation of different polypropylene-mesh modifications for abdominal wall repair. Biomaterials 19:2235–2246
Junge K, Klinge U, Rosch R, Klosterhalfen B, Schumpelick V (2002) Functional and morphologic properties of a modified mesh for inguinal hernia repair. World J Surg 26:1472–1480
Junge K, Klinge U, Prescher A, Giboni P, Niewiera M, Schumpelick V (2001) Elasticity of the anterior abdominal wall and impact for reparation of incisional hernias using mesh implants. Hernia 5:113–118
Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski B, Ottinger AP et al (1998) Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg 164:951–960
Bringman S, Wollert S, Osterberg J, Smedberg S, Granlund H, Heikkinen TJ (2006) Three-year results of a randomized clinical trial of lightweight or standard polypropylene mesh in Lichtenstein repair of primary inguinal hernia. Br J Surg 93:1056–1059
O’dwyer PJ, Kingsnorth AN, Molloy RG, Small PK, Lammers B, Horeyseck G (2005) Randomized clinical trial assessing impact of a lightweight or heavyweight mesh on chronic pain after inguinal hernia repair. Br J Surg 92:166–170
Horstmann R, Hellwig M, Classen C, Rottgermann S, Palmes D (2006) Impact of polypropylene amount on functional outcome and quality of life after inguinal hernia repair by the TAPP procedure using pure, mixed, and titanium-coated meshes. World J Surg 30:1742–1749
Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 194:394–400
Johnson SG (1970) Testicular biopsy score count—a method for registration of spermatogenesis in human testes: normal values and results in 335 hypogonadal males. Hormones 1:2–25
Pollak R, Nyhus LM (1983) Complications of groin hernia repair. Surg Clin North Am 63:1363–1371
Shin D, Lipshultz LI, Goldstein M, Barme GA, Fuchs EF, Nagler HM, McCallum S, Niederberger C, Schoor R, Brugh V, Honig S (2005) Herniorrhaphy with polypropylene mesh causing inguinal vasal obstruction: a preventable cause of obstructive azoospermia. Ann Surg 241:553–558
Uzzo RG, Lemack GE, Morrissey KP, Goldstein M (1999) The effects of mesh bioprosthesis on the spermatic cord structures: a preliminary report in a canine model. J Urol 161:1344–1349
Goldenberg A, Matone J, Marcondes W, Herbella FA, Farah JF (2005) Comparative study of inflammatory response and adhesions formation after fixation of different meshes for inguinal hernia repair in rabbits. Acta Cir Bras 20:347–352
Peiper C, Junge K, Klinge U, Strehlau E, Krones C, Ottinger A et al. (2005) The influence of inguinal mesh repair on the spermatic cord: a pilot study in the rabbit. J Invest Surg 18:273–278
Berndsen FH, Bjursten LM, Simanaitis M, Montgomery A (2004) Does mesh implantation affect the spermatic cord structures after inguinal hernia surgery? An experimental study in rats. Eur Surg Res 36:318–322
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Junge, K., Binnebösel, M., Rosch, R. et al. Influence of mesh materials on the integrity of the vas deferens following Lichtenstein hernioplasty: an experimental model. Hernia 12, 621–626 (2008). https://doi.org/10.1007/s10029-008-0400-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-008-0400-2