Abstract
Objective
This study aimed to assess the effect of titanium dioxide (TiO2) and silver (Ag) nanoparticles dispersed in glycerol or water, serving as optical clearing agents nanocolloids (OCAs-NC), for improving optical coherence tomography (OCT) images and highlighting incipient lesions in ex vivo human teeth.
Materials and methods
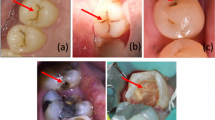
Twelve human teeth with incipient lesions were divided into seven groups according to the OCA-NC; they were subjected to G1 (air), G2 (glycerol), G3 (TiO2 0.1%), G4 (TiO2 0.01%), G5 (TiO2 0.001%), G6 (AgNO3 10%), and G7 (AgNO3 100%). The OCA-NC was applied to the occlusal surface, and two-dimensional images of the specimens were analyzed using OCT (930 nm central wavelength; 100 nm bandwidth; 5 mW output power; axial resolution of 7/5.3 μm in water and air, respectively; lateral resolution of 8 μm; and light penetration depth of 1.6 mm inside the sample).
Results
The findings demonstrated that the utilization of OCAs-NC containing metallic or dielectric nanoparticles (AgNO3 and TiO2) led to improved differentiation between sound and demineralized enamel on occlusal surfaces. Additionally, it enhanced the depth of image penetration when analyzing this hard tissue with OCT.
Clinical relevance
In the current context of minimally invasive dentistry, the use of OCAs-NC in conjunction with OCT can provide clinicians with early diagnosis, allowing for the determination of less/more invasive therapies and consequently halting the disease before cavitation of dental tissues occurs.







Similar content being viewed by others
Data availability
All data underlying the results are available as part of the article, and no additional source data is applicable.
References
Machiulskiene V et al (2020) Terminology of dental caries and dental caries management: consensus report of a workshop organized by ORCA and Cariology Research Group of IADR. Caries Res 54(1):7–14. https://doi.org/10.1159/000503309
Drancourt N et al (2019) Carious lesion activity assessment in clinical practice: a systematic review. Clin Oral Invest 23:1513–1524. https://doi.org/10.1007/s00784-019-02839-7
Pitts NB, Twetman S, Fisher J, Marsh PD (2021) Understanding dental caries as a non-communicable disease. Br Dent J 231(12):749–753. https://doi.org/10.1038/s41415-021-3775-4
Kapor S et al (2021) Systematic review and meta-analysis of diagnostic methods for occlusal surface caries. Clin Oral Invest 25(8):4801–4815. https://doi.org/10.1007/s00784-021-04024-1
Schwendicke F et al (2019) When to intervene in the caries process? An expert Delphi consensus statement. Clin Oral Invest 23:3691–3703. https://doi.org/10.1007/s00784-019-03058-w
Şen S et al (2020) Demineralization detection in orthodontics using an ophthalmic optical coherence tomography device equipped with a multicolor fluorescence module. Clin Oral Invest 24:2579–2590. https://doi.org/10.1007/s00784-019-03116-3
Gomes ASL, Valente D (2023) Optical coherence tomography: from basics to general applications. In: Optical coherence tomography in dentistry: scientific developments to clinical applications. (1st ed.). CRC Press. https://doi.org/10.1201/9781351104562
Shimada Y et al (2020) Evaluation of dental caries, tooth crack, and age-related changes in tooth structure using optical coherence tomography. Jpn Dent Sci Rev 56(1):109–118. https://doi.org/10.1016/j.jdsr.2020.08.001
Monteiro GQ et al (2011) Marginal analysis of resin composite restorative systems using optical coherence tomography. Dent Mater 27(12):e213–e223. https://doi.org/10.1016/j.dental.2011.08.400
Mota CC et al (2013) Optical coherence tomography as an auxiliary tool for the screening of radiation-related caries. Photomed Laser Surg 31(7):301–306. https://doi.org/10.1089/pho.2012.3415
Kitasako Y et al (2019) Remineralization capacity of carious and non-carious white spot lesions: clinical evaluation using ICDAS and SS-OCT. Clin Oral Inv 23(2):863–872. https://doi.org/10.1007/s00784-018-2503-1
Bolukbasi S et al (2020) Retinal structural changes in patients receiving tamoxifen therapy by spectral-domain optical coherence tomography. Cutan Ocul Toxicol 39(2):115–121. https://doi.org/10.1080/15569527.2020.1734816
Gune S et al (2020) Spectral-domain OCT-based prevalence and progression of macular atrophy in the HARBOR study for neovascular age-related macular degeneration. Ophthalmology 127(4):523–532. https://doi.org/10.1016/j.ophtha.2019.09.030
Fernandes LO et al (2019) Optical coherence tomography follow-up of patients treated from periodontal disease. J Biophotonics 12(2):e201800209. https://doi.org/10.1002/jbio.201800209
Merle CL et al (2022) Clinical and OCT assessment of application modes of a universal adhesive in a 12-month RCT. J Dent 119:104068. https://doi.org/10.1016/j.jdent.2022.104068
Das A et al (2022) Exploiting nanomaterials for optical coherence tomography and photoacoustic imaging in nanodentistry. Nanomaterials (Basel, Switzerland) 12(3):506. https://doi.org/10.3390/nano12030506
Gomes AS, Zezell DM, Mota CC, Girkin, JM (Eds.) (2023) Optical coherence tomography in Dentistry: scientific developments to clinical applications (1st ed.). CRC Press. https://doi.org/10.1201/9781351104562
Zezel DM, Ana PA (2024) OCT in cariology: in vitro and in vivo studies. In: Optical coherence tomography in dentistry: scientific developments to clinical applications. (1st ed.). CRC Press. https://doi.org/10.1201/9781351104562
Ţogoe MM et al (2021) Endodontic fillings evaluated using en face OCT, microCT and SEM. Rom J Morphol Embryol 62(3):793–800. https://doi.org/10.47162/RJME.62.3.17
Kim Y et al (2021) Non-invasive optical coherence tomography data-based quantitative algorithm for the assessment of residual adhesive on bracket-removed dental surface. Sensors (Basel) 21(14):4670. https://doi.org/10.3390/s21144670
Matheus TC et al (2010) Fracture process characterization of fiber-reinforced dental composites evaluated by optical coherence tomography, SEM and optical microscopy. Braz Dent J 21(5):420–427. https://doi.org/10.1590/s0103-64402010000500008
Kim DH, Kim SW, Hwang SH (2023) Efficacy of optical coherence tomography in the diagnosing of oral cancerous lesion: systematic review and meta-analysis. Head Neck 45(2):473–481. https://doi.org/10.1002/hed.27232
Kang H, Darling CL, Fried D (2016) Enhancement of OCT images with vinyl polysiloxane (VPS). Proc SPIE Int Soc Opt Eng 9692:96920T. https://doi.org/10.1117/12.2218649
Bykov A et al (2016) Imaging of subchondral bone by optical coherence tomography upon optical clearing of articular cartilage. J Biophotonics 9(3):270–275. https://doi.org/10.1002/jbio.201500130
Liang Y, Yuan W, Mavadia-Shukla J, Li X (2016) Optical clearing for luminal organ imaging with ultrahigh-resolution optical coherence tomography. J Biomed Opt 21(8):081211. https://doi.org/10.1117/1.JBO.21.8.081211
Ali S et al (2021) Optical coherence tomography’s current clinical medical and dental applications: a review. F1000 Research 10:310. https://doi.org/10.12688/f1000research.52031.1
Larin K et al (2011) Optical clearing for OCT image enhancement and in-depth monitoring of molecular diffusion. IEEE J Sel Top Quantum Electron 18(3):1244–1259
Yu T et al (2018) Optical clearing for multiscale biological tissues. Journal of Biophotonics 11(2):https://doi.org/10.1002/jbio.201700187.
Yin X et al (2019) Spatial distribution of motor endplates and its adaptive change in skeletal muscle. Theranostics 9(3):734–746. https://doi.org/10.7150/thno.28729
Zhang BW et al (2019) Multidither coherent optical adaptive technique for deep tissue two-photon microscopy. J Innov Opt Health Sci 12(04):1942003. https://doi.org/10.1142/S1793545819420033
Zaytsev SM, Amouroux M, Tuchin VV, Genina EA, Blondel W (2023) In vivo skin optical clearing efficacy quantification of clinically compatible agents using line-field confocal optical coherence tomography. J Biomed Opt 28(5):055002. https://doi.org/10.1117/1.JBO.28.5.055002
Mota CC, Fernandes LO, Cimoes R, Gomes AS (2015) Non-invasive periodontal probing through Fourier-domain optical coherence tomography. J Periodontol 86(9):1087–1094
Foros P et al (2021) Detection methods for early caries diagnosis: a systematic review and meta-analysis. Caries Res 55(4):247–259. https://doi.org/10.1159/000516084
Sahyoun CC et al (2020) An experimental review of optical coherence tomography systems for noninvasive assessment of hard dental tissues. Caries Res 54(1):43–54. https://doi.org/10.1159/000502375
Nguyen TT, Miller A, Orellana MF (2011) Characterization of the porosity of human dental enamel and shear bond strength in vitro after variable etch times: initial findings using the BET method. Angle Orthod 81(4):707–715. https://doi.org/10.2319/083010-506.1
Kang H, Darling CL, Fried D (2014) Enhancing the detection of hidden occlusal caries lesions with OCT using high index liquids. Proc SPIE Int Soc Opt Eng 8929:89290O. https://doi.org/10.1117/12.2045681
Butt MA et al (2019) Investigating the optical properties of a laser induced 3D self-assembled carbon-metal hybrid structure. Small 15(18):e1900512. https://doi.org/10.1002/smll.201900512
Kupriianov AS et al (2023) Trapped mode control in metasurfaces composed of particles with the form birefringence property. Opt Express 31(4):6996–7011. https://doi.org/10.1364/OE.483569
Funding
The work was supported by the CAPES (Coordination for the Improvement of Higher Education Personnel) for scholarship for VSMC, ELM, and JMM; the INCT-INFO (National Institutes of Science and Technology, Institute of Photonics) process 465.763/2014–6, supported by CNPq/MCTI (Brazilian National Council for Scientific and Technological Development and Ministry of Science, Technology and Innovation); and the PRONEX program (Center of Excellence on Biophotonics and Nanophotonics), process APQ-0504–1.05/14, sponsored by FACEPE/CNPq (Foundation for Science and Technology of Pernambuco State and Brazilian National Council for Scientific and Technological Development).
Author information
Authors and Affiliations
Contributions
VSMC conducted the research in its entirety; ELM prepared the manuscript and submitted it to the journal; CCBOM and EJS collaborated in conducting the experiments; AFS synthesized the nanoparticles for the experiments; NSD, JMM, and SISR edited the figures and tables; CLP translated the manuscript into English; ASLG co-supervised the research and revised the manuscript. MEMMG co-supervised the research.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All procedures performed in this study were conducted in accordance with the ethical standards of the local. Furthermore, this study followed all the guidelines outlined in the Helsinki Declaration.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Carneiro, V.S.M., de Melo, E.L., de Oliveira Mota, C.C.B. et al. Optical clearing agents based on metallic and dielectric nanoparticles for caries diagnostic by optical coherence tomography. Clin Oral Invest 28, 72 (2024). https://doi.org/10.1007/s00784-023-05473-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-023-05473-6