Abstract
Objectives
The purposes of this retrospective study were to investigate the prevalence of various periodontal chief complaints (pCCs) of patients, diagnosed with periodontitis, as well as to identify the association between pCCs and periodontal parameters or periodontitis staging according to AAP/EFP 2017 classification.
Materials and methods
Five hundred eighty-nine patients, applied to the clinic with pCCs, were screened. The demographic characteristics, smoking status, brushing behaviors, history of periodontal therapy, medical data, and periodontal parameters were obtained. A multinomial logistic regression analysis was performed to determine the most common pCCs and co-variables among the indicators of Stage III and IV periodontitis.
Results
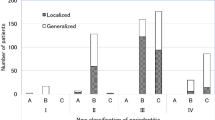
In Stage IV periodontitis, patients with pCC of mobility were observed the most (26.8%), and pCC of halitosis were the least (7.3%). Among all pCCs of patients, those with the pCC of gingival enlargement and tooth mobility had the highest percentage of sites with PPD ≥ 4 mm and CAL ≥ 5 mm, respectively (p < .001). According to regression analysis, those with pCC of gingival bleeding, recession and mobility were more likely to be in Stage IV than those in Stage I/II.
Conclusion
Among pCCs, only patients with pCCs of mobility, gingival recession and bleeding are related to periodontitis staging. Moreover, the extent of periodontal pockets in patients with pCC of gingival enlargement, and the extent of attachment loss in patients with pCC of mobility are greater than other patients.
Clinical relevance
New machine-learning technology models can be developed with the aim of classifying the patients based on their chief complaints, to support diagnosing the severity of periodontal diseases.
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Page RC, Kornman KS (1997) The pathogenesis of human periodontitis: an introduction. Periodontol 2000 14:9–11. https://doi.org/10.1111/j.1600-0757.1997.tb00189.x
Kassebaum N, Bernabé E, Dahiya M, Bhandari B, Murray C, Marcenes W (2014) Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res 93:1045–1053
Janakiram C, Dye BA (2020) A public health approach for prevention of periodontal disease. Periodontol 2000 84:202–214. https://doi.org/10.1111/prd.12337
Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J (2017) Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J Clin Periodontol 44:456–462. https://doi.org/10.1111/jcpe.12732
Jin L (2015) Group E. Initiator paper. Interprofessional education and multidisciplinary teamwork for prevention and effective management of periodontal disease. J Int Acad Periodontol 17:74–79
Liu KZ, Duarte PM, Santos VR, Xiang X, Xu M, Miranda TS, Fermiano D, Gonçalves TE, Sowa MG (2014) Assessment of tissue oxygenation of periodontal inflammation in smokers using optical spectroscopy. J Clin Periodontol 41:340–347. https://doi.org/10.1111/jcpe.12225
Chapple ILC (2014) Time to take periodontitis seriously. BMJ Br Med J 348:g2645. https://doi.org/10.1136/bmj.g2645
Chapple ILC, Bouchard P, Cagetti MG, Campus G, Carra M-C, Cocco F, Nibali L, Hujoel P, Laine ML, Lingström P, Manton DJ, Montero E, Pitts N, Rangé H, Schlueter N, Teughels W, Twetman S, Van Loveren C, Van der Weijden F, Vieira AR, Schulte AG (2017) Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol 44:S39–S51. https://doi.org/10.1111/jcpe.12685
Hansoti B, Hahn E, Rao A, Harris J, Jenson A, Markadakis N, Moonat S, Osula V, Pousson A (2021) Calibrating a chief complaint list for low resource settings: a methodologic case study. Int J Emerg Med 14:32. https://doi.org/10.1186/s12245-021-00347-8
Abdulkareem AA, Abdulbaqi HR, Nayyef AK, Saleem SS (2019) Investigation of the consistency between reported chief complaint and periodontal health status of Iraqi patients in relation to age and gender (A retrospective study). J Bagh Coll Dent 31:65–69. https://doi.org/10.26477/jbcd.v31i2.2626
Brunsvold MA, Nair P, Oates TW Jr (1999) Chief complaints of patients seeking treatment for periodontitis. J Am Dent Assoc 130:359–64. https://doi.org/10.14219/jada.archive.1999.0205
Yeh HC, Lai H (2011) Association between patients’ chief complaints and their compliance with periodontal therapy. J Clin Periodontol 38:449–456
Abdulkareem AA, Imran NK, Abdulraheam RH, Gul SS (2021) Prevalence and factors influencing reporting of true periodontal chief complaints: A retrospective analysis. Clin Exp Dent Res 7:443–449. https://doi.org/10.1002/cre2.385
Elhassan AT, Alfakry H, Peeran SW (2017) Reasons to seek periodontal treatment in a libyan community. Dent Med Res 5:38
Grover V, Malhotra R, Kapoor A, Kaur G, Kaur RK, Sahota JK (2017) Chief complaints of patients seeking treatment for Periodontitis. Int Dent J Stud Res 5:19–24
Ertaş K, Pence I, Cesmeli MS, Ay ZY (2023) Determination of the stage and grade of periodontitis according to the current classification of periodontal and peri-implant diseases and conditions (2018) using machine learning algorithms. J Periodontal Implant Sci 53:38–53. https://doi.org/10.5051/jpis.2201060053
Farhadian M, Shokouhi P, Torkzaban P (2020) A decision support system based on support vector machine for diagnosis of periodontal disease. BMC Res Notes 13:337. https://doi.org/10.1186/s13104-020-05180-5
Ozden F, Ozgonenel O, Ozden B, Aydogdu A (2015) Diagnosis of periodontal diseases using different classification algorithms: A preliminary study. Niger J Clin Pract 18:416–421
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Clin Periodontol 45:S149–S161. https://doi.org/10.1111/jcpe.12945
Stewart M, Brown JB, Weston W, McWhinney IR, McWilliam CL, Freeman T (2013) Patient-centered medicine: transforming the clinical method. CRC Press
Romano F, Perotto S, Bianco L, Parducci F, Mariani GM, Aimetti M (2020) Self-perception of periodontal health and associated factors: A cross-sectional population-based study. Int J Environ Res Public Health 17:2758
Haveman-Nies A, de Groot LC, van Staveren WA (2003) Dietary quality, lifestyle factors and healthy ageing in Europe: the SENECA study. Age Ageing 32:427–434. https://doi.org/10.1093/ageing/32.4.427
Pruchno R, Hahn S, Wilson-Genderson M (2012) Cigarette smokers, never-smokers, and transitions: implications for successful aging. Int J Aging Hum Dev 74:193–209. https://doi.org/10.2190/AG.74.3.b
Silness J, Löe H (1964) Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 22:121–135
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25:229–235
Campos JR, Costa FO, Cota LOM (2020) Association between periodontitis and metabolic syndrome: A case-control study. J Periodontol 91:784–791. https://doi.org/10.1002/JPER.19-0298
Devaraj C, Eswar P (2012) Reasons for use and non-use of dental services among people visiting a dental college hospital in India: A descriptive cross-sectional study. Eur J Dent 6:422–427
Buchwald S, Kocher T, Biffar R, Harb A, Holtfreter B, Meisel P (2013) Tooth loss and periodontitis by socio-economic status and inflammation in a longitudinal population-based study. J Clin Periodontol 40:203–211. https://doi.org/10.1111/jcpe.12056
Baehni P, Giovannoli J-L (2014) Patient profile and decision-making in periodontal practice. Periodontol 2000 36:27–34. https://doi.org/10.1111/j.1600-0757.2004.03672.x
Coventry J, Griffiths G, Scully C, Tonetti M (2000) Periodontal disease. BMJ 321:36–39
Wong LB, Yap AU, Allen PF (2021) Periodontal disease and quality of life: Umbrella review of systematic reviews. J Periodontal Res 56:1–17. https://doi.org/10.1111/jre.12805
Jepsen K, Tietmann C, Kutschera E, Wüllenweber P, Jäger A, Cardaropoli D, Gaveglio L, Sanz Sanchez I, Martin C, Fimmers R, Jepsen S (2021) The effect of timing of orthodontic therapy on the outcomes of regenerative periodontal surgery in patients with stage IV periodontitis: A multicenter randomized trial. J Clin Periodontol 48:1282–1292. https://doi.org/10.1111/jcpe.13528
Montero E, Molina A, Palombo D, Morón B, Pradíes G, Sanz-Sánchez I (2022) Efficacy and risks of tooth-supported prostheses in the treatment of partially edentulous patients with stage IV periodontitis. A systematic review and meta-analysis. J Clin Periodontol 49(Suppl 24):182–207. https://doi.org/10.1111/jcpe.13482
Merli M, Fratini A, Sforza NM, Landi L, Pagliaro U, Franchi L, Nieri M (2022) Clinical decision-making and management of stage IV periodontitis: a survey. Oral Dis. https://doi.org/10.1111/odi.14366
Demetriou N, Tsami-Pandi A, Parashis A (1991) Is it possible for periodontal patients to recognize periodontal disease. Stomatologia (Bucur) 47:284–295
Mento C, Lombardo C, Milazzo M, Whithorn NI, Boronat-Catalá M, Almiñana-Pastor PJ, Fernàndez CS, Bruno A, Muscatello MRA, Zoccali RA (2021) Adolescence, adulthood and self-perceived halitosis: a role of psychological factors. Medicina 57:614
Adedapo AH, Kolude B, Dada-Adegbola HO, Lawoyin JO, Adeola HA (2020) Targeted polymerase chain reaction-based expression of putative halitogenic bacteria and volatile sulphur compound analysis among halitosis patients at a tertiary hospital in Nigeria. Odontology 108:450–461. https://doi.org/10.1007/s10266-019-00467-x
Lertpimonchai A, Rattanasiri S, Arj-Ong Vallibhakara S, Attia J, Thakkinstian A (2017) The association between oral hygiene and periodontitis: a systematic review and meta-analysis. Int Dent J 67:332–343. https://doi.org/10.1111/idj.12317
Kornman KS, Papapanou PN (2020) Clinical application of the new classification of periodontal diseases: Ground rules, clarifications and “gray zones.” J Periodontol 91:352–360. https://doi.org/10.1002/JPER.19-0557
Paulander J, Axelsson P, Lindhe J, Wennström J (2004) Some characteristics of 50/55-year-old individuals with various experience of destructive periodontal disease: a cross-sectional study. Acta Odontol Scand 62:199–206. https://doi.org/10.1080/00016350410001621
Acknowledgements
The authors would like to thank Prof. Dr. Emel Ökte, from the Department of Periodontology, Gazi University Faculty of Dentistry, who edited together in the organization of the periodontal indexes and anamnesis in the clinic before receiving the retrospective data. The authors dedicate this article to the memory of all those who lost their lives and to all people affected due to the devastating earthquake hitting Türkiye on February 6, 2023.
Funding
The authors declared that this study has received no financial support. This study did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SG planned and designed the research, wrote, and reviewed the manuscript. MA was responsible for obtaining ethical approval, and preparing data for statistical analysis. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Ethics committee approval was received for this study from the ethics committee of the Human Subjects Review Board of Gazi University (approval No: GUEC 2020–466).
Consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
No conflict of interest was declared by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Periodontal chief complaints and periodontal status
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gürbüz, S., Altıkat, M. The association between periodontitis patients’ chief complaints and the stage of periodontitis: A clinical retrospective study. Clin Oral Invest 27, 6261–6272 (2023). https://doi.org/10.1007/s00784-023-05258-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05258-x