Abstract
Objectives
To compare the effectiveness and side effects of miniscrew-assisted rapid maxillary expansion (MARME) with conventional rapid maxillary expansion (RME) in the treatment of transverse maxillary deficiency.
Materials and methods
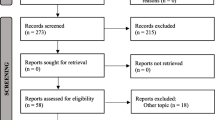
We conducted a systematic review and meta-analysis of randomized controlled trials (RCTs). We searched in the MEDLINE, Embase, and Cochrane Central databases. The quality of included RCTs was evaluated using the Cochrane risk-of-bias tool. The primary outcome was the extent of dentoskeletal expansion achieved. Secondary outcomes were the dental and periodontal side effects. We calculated summary weighted mean differences (MD) with 95% confidence intervals (CI) using random-effects meta-analysis.
Results
Six RCTs involving 287 participants met the inclusion criteria. Compared to conventional RME, MARME was associated with a greater palatal suture opening (mm) measured at the anterior nasal spine (MD = 1.21, 95% CI 0.75 to 1.66), first premolars (MD = 1.13, 95% CI 0.72 to 1.55), first molars (MD = 1.18, 95% CI 0.28 to 2.09), and posterior nasal spine (MD = 1.14, 95% CI 0.30 to 1.98), increased palatal width (mm) at the first molars (MD = 0.75, 95% CI 0.30 to 1.20), and reduced buccal inclination (degrees) of the first premolars (MD = − 6.06, 95% CI − 10.36 to − 1.76) and first molars (MD = − 3.17, 95% CI − 5.35 to − 0.99).
Conclusions
MARME is associated with the following advantages over traditional tooth-borne RME: increased palatal suture opening, increased palatal width, and reduced buccal tooth inclination.
Registration
This study is registered with PROSPERO, CRD42021256750.
Clinical relevance
MARME may be preferred over conventional RME in cases with fused mid-palatal sutures or where further buccal tooth inclination is undesirable.





Similar content being viewed by others
References
Menon S, Manerikar R, Sinha R (2010) Surgical management of transverse maxillary deficiency in adults. J Maxillofac Oral Surg 9:241–246. https://doi.org/10.1007/s12663-010-0034-7
D’Souza IM, Kumar HCK, Shetty KS (2015) Dental arch changes associated with rapid maxillary expansion: a retrospective model analysis study. Contemp Clin Dent 6:51–57. https://doi.org/10.4103/0976-237X.149292
Andrucioli MCD, Matsumoto MAN (2020) Transverse maxillary deficiency: treatment alternatives in face of early skeletal maturation. Dental Press J Orthod 25:70–79. https://doi.org/10.1590/2177-6709.25.1.070-079.bbo
Kapetanović A, Theodorou CI, Bergé SJ et al (2021) Efficacy of miniscrew-assisted rapid palatal expansion (MARPE) in late adolescents and adults: a systematic review and meta-analysis. Eur J Orthod 43:313–323. https://doi.org/10.1093/ejo/cjab005
Tripathi T, Kalra S, Rai P (2020) Management of skeletal Class III with facial asymmetry using skeletal anchorage: 4-year follow-up. Dental Press J Orthod 25:24. https://doi.org/10.1590/2177-6709.25.2.24.e1-9.onl
Haas AJ (1961) Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod 31:73–90. https://doi.org/10.1043/0003-3219(1961)031%3c0073:REOTMD%3e2.0.CO;2
Haas AJ (1965) The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod 35:200–217. https://doi.org/10.1043/0003-3219(1965)035%3c0200:TTOMDB%3e2.0.CO;2
Haas AJ (1970) Palatal expansion: just the beginning of dentofacial orthopedics. Am J Orthod 57:219–255. https://doi.org/10.1016/0002-9416(70)90241-1
Ghoneima A, Abdel-Fattah E, Hartsfield J et al (2011) Effects of rapid maxillary expansion on the cranial and circummaxillary sutures. Am J Orthod Dentofacial Orthop 140:510–519. https://doi.org/10.1016/j.ajodo.2010.10.024
Lione R, Franchi L, Cozza P (2013) Does rapid maxillary expansion induce adverse effects in growing subjects? Angle Orthod 83:172–182. https://doi.org/10.2319/041012-300.1
Suzuki H, Moon W, Previdente LH et al (2016) Miniscrew-assisted rapid palatal expander (MARPE): the quest for pure orthopedic movement. Dental Press J Orthod 21:17–23. https://doi.org/10.1590/2177-6709.21.4.017-023.oin
Agarwal A, Mathur R (2010) Maxillary expansion. Int J Clin Pediatr Dent 3:139–146. https://doi.org/10.5005/jp-journals-10005-1069
Lo Giudice A, Barbato E, Cosentino L et al (2018) Alveolar bone changes after rapid maxillary expansion with tooth-born appliances: a systematic review. Eur J Orthod 40:296–303. https://doi.org/10.1093/ejo/cjx057
Basciftci FA, Mutlu N, Karaman AI et al (2002) Does the timing and method of rapid maxillary expansion have an effect on the changes in nasal dimensions? Angle Orthod 72:118–123. https://doi.org/10.1043/0003-3219(2002)072%3c0118:DTTAMO%3e2.0.CO;2
Watson WG (1980) Expansion and fenestration or dehiscence. Am J Orthod 77:330–332. https://doi.org/10.1016/0002-9416(80)90086-x
Garib DG, Henriques JFC, Janson G et al (2006) Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: a computed tomography evaluation. Am J Orthod Dentofacial Orthop 129:749–758. https://doi.org/10.1016/j.ajodo.2006.02.021
Samandara A, Papageorgiou SN, Ioannidou-Marathiotou I et al (2019) Evaluation of orthodontically induced external root resorption following orthodontic treatment using cone beam computed tomography (CBCT): a systematic review and meta-analysis. Eur J Orthod 41:67–79. https://doi.org/10.1093/ejo/cjy027
Carmen M, Marcella P, Giuseppe C, Roberto A (2000) Periodontal evaluation in patients undergoing maxillary expansion. J Craniofac Surg 11:491–494. https://doi.org/10.1097/00001665-200011050-00009
Ribeiro Prado GP, Pereira MD, Rocha Biló JP et al (2013) Stability of surgically assisted rapid palatal expansion: a randomized trial. J Dent Res 92:S49–S54. https://doi.org/10.1177/0022034513486899
Carvalho PHA, Moura LB, Trento GS et al (2020) Surgically assisted rapid maxillary expansion: a systematic review of complications. Int J Oral Maxillofac Surg 49:325–332. https://doi.org/10.1016/j.ijom.2019.08.011
Lee K-J, Park Y-C, Park J-Y, Hwang W-S (2010) Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop 137:830–839. https://doi.org/10.1016/j.ajodo.2007.10.065
Krüsi M, Eliades T, Papageorgiou SN (2019) Are there benefits from using bone-borne maxillary expansion instead of tooth-borne maxillary expansion? A systematic review with meta-analysis. Prog Orthod 20:9. https://doi.org/10.1186/s40510-019-0261-5
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Bazargani F, Magnuson A, Ludwig B (2018) Effects on nasal airflow and resistance using two different RME appliances: a randomized controlled trial. Eur J Orthod 40:281–284. https://doi.org/10.1093/ejo/cjx081
Canan S, Şenışık NE (2017) Comparison of the treatment effects of different rapid maxillary expansion devices on the maxilla and the mandible. Part 1: Evaluation of dentoalveolar changes. Am J Orthod Dentofacial Orthop 151:1125–1138. https://doi.org/10.1016/j.ajodo.2016.11.022
Jia H, Zhuang L, Zhang N et al (2021) Comparison of skeletal maxillary transverse deficiency treated by microimplant-assisted rapid palatal expansion and tooth-borne expansion during the post-pubertal growth spurt stage. Angle Orthod 91:36–45. https://doi.org/10.2319/041920-332.1
Kayalar E, Schauseil M, Kuvat SV et al (2016) Comparison of tooth-borne and hybrid devices in surgically assisted rapid maxillary expansion: a randomized clinical cone-beam computed tomography study. J Craniomaxillofac Surg 44:285–293. https://doi.org/10.1016/j.jcms.2015.12.001
Koudstaal MJ, Wolvius EB, Schulten AJM et al (2009) Stability, tipping and relapse of bone-borne versus tooth-borne surgically assisted rapid maxillary expansion; a prospective randomized patient trial. Int J Oral Maxillofac Surg 38:308–315. https://doi.org/10.1016/j.ijom.2009.02.012
Lagravère MO, Oscar M (2009) Analysis of skeletal and dental changes with a tooth-borne and a bone-borne maxillary expansion appliance assessed through digital volumetric imaging. https://era.library.ualberta.ca/items/cd48f9ea-32f7-46aa-9c04-3c5d180a1ebe. Accessed June 19
Lagravère MO, Carey J, Heo G et al (2010) Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs traditional rapid maxillary expansion: a randomized clinical trial. Am J Orthod Dentofacial Orthop 137(304):e1-12. https://doi.org/10.1016/j.ajodo.2009.09.016
Mehta S, Chen P-J, Vich ML, et al (2021) Bone-anchored versus tooth-anchored expansion appliances: Long-term effects on the condyle-fossa relationship. J World Fed Orthod S2212–4438(21)00031-X. https://doi.org/10.1016/j.ejwf.2021.07.001
Mehta S, Wang D, Kuo C-L et al (2021) Long-term effects of mini-screw-assisted rapid palatal expansion on airway. Angle Orthod 91:195–205. https://doi.org/10.2319/062520-586.1
Pham V, Lagravère MO (2017) Alveolar bone level changes in maxillary expansion treatments assessed through CBCT. Int Orthod 15:103–113. https://doi.org/10.1016/j.ortho.2016.12.002
Khosravi M, Ugolini A, Miresmaeili A et al (2019) Tooth-borne versus bone-borne rapid maxillary expansion for transverse maxillary deficiency: a systematic review. Int Orthod 17:425–436. https://doi.org/10.1016/j.ortho.2019.06.003
Bazargani F, Feldmann I, Bondemark L (2013) Three-dimensional analysis of effects of rapid maxillary expansion on facial sutures and bones. Angle Orthod 83:1074–1082. https://doi.org/10.2319/020413-103.1
Lim H-M, Park Y-C, Lee K-J, Choi K-HK, YJ, (2017) Stability of dental, alveolar, and skeletal changes after miniscrew-assisted rapid palatal expansion. Korean J Orthod 47:313–322. https://doi.org/10.4041/kjod.2017.47.5.313
de Jesus AS, de Oliveira CB, Murata WH et al (2021) Would midpalatal suture characteristics help to predict the success rate of miniscrew-assisted rapid palatal expansion? Am J Orthod Dentofacial Orthop 160:363–373. https://doi.org/10.1016/j.ajodo.2020.04.035
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This article does not contain studies with human participants or animals performed by any of the authors.
Consent to participate
For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Bi, W.G., Li, K. Effectiveness of miniscrew-assisted rapid maxillary expansion: a systematic review and meta-analysis. Clin Oral Invest 26, 4509–4523 (2022). https://doi.org/10.1007/s00784-022-04415-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04415-y