Abstract
Objectives
Androgenic anabolic steroids (AAS) abuse is a serious health problem associated to several systemic complications. Here, we evaluated the periodontal clinical status, microbial profile, and expression of total protein (TP) and interleukin (IL)-1β in men using AAS.
Materials and methods
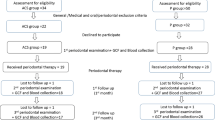
Men using AAS were recruited (case group) and matched for age with men who had never used AAS (control group) but also performed physical activities. Plaque index (PI), marginal bleeding (MB), probing depth (PD), clinical attachment level (CAL), and bleeding on probing (BoP) were evaluated. Crevicular fluid and subgingival biofilm were collected from healthy and diseased sites (PD ≥ 4 mm with CAL ≥ 1 mm and BoP) and evaluated for TP, IL-1β, and proportions of 40 bacterial species.
Results
Thirty patients were included (n = 15/group). AAS consumers had significantly higher mean PD and higher percentage of diseased sites; sites with PD ≥ 4 mm or with CAL ≥ 1 mm than non-consumers. Also, AAS users showed a more dysbiotic biofilm containing lower proportions of host-compatible species and higher proportions of pathogens. IL-1β expression was statistically higher in diseased than in healthy sites only in the control group. A statistically positive correlation was detected between periodontal pathogens and IL-1β expression. The number of AAS cycles was positively associated with higher percentages of periodontal pathogens, but not with IL-1β or total protein concentrations.
Conclusions
AAS intake can worsen clinical and immunological periodontal conditions and the biofilm composition in healthy sites.
Clinical relevance
Dental care professionals should perform full mouth periodontal screening and schedule regular follow-up appointments for patients under AAS use.




Similar content being viewed by others
References
Bain J (2010) Testosterone and the aging male: to treat or not to treat? Maturitas 66:16–22
Rahnema CD, Crosnoe LE, Kim ED (2015) Designer steroids - over-the-counter supplements and their androgenic component: review of an increasing problem. Andrology 3:150–155
Kanayama G, Kaufman MJ, Pope HG Jr (2018) Public health impact of androgens. Curr Opin Endocrinol Diabetes Obes 25:218–223
Brower KJ, Eliopulos GA, Blow FC, Catlin DH, Beresford TP (1990) Evidence for physical and psychological dependence on anabolic androgenic steroids in eight weight lifters. Am J Psychiatry 147:510–512
Basaria S (2010) Androgen abuse in athletes: detection and consequences. J Clin Endocrinol Metab 95:1533–1543
Korkia P, Stimson GV (1997) Indications of prevalence, practice and effects of anabolic steroid use in Great Britain. Int J Sports Med 18:557–562
Soory M (2000) Targets for steroid hormone mediated actions of periodontal pathogens, cytokines and therapeutic agents: some implications on tissue turnover in the periodontium. Curr Drug Targets 1:309–325
Kasasa SC, Soory M (1996) The synthesis of 5-alpha-dihydrotestosterone from androgens by human gingival tissues and fibroblasts in culture in response to TGF-beta and PDGF. J Periodontal Res 31:313–322
Coletta RD, Reynolds MA, Martelli-Junior H, Graner E, Almeida OP, Sauk JJ (2002) Testosterone stimulates proliferation and inhibits interleukin-6 production of normal and hereditary gingival fibromatosis fibroblasts. Oral Microbiol Immunol 17:186–192
Soory M, Tilakaratne A (2003) Anabolic potential of fibroblasts from chronically inflamed gingivae grown in a hyperglycemic culture medium in the presence or absence of insulin and nicotine. J Periodontol 74:1771–1777
Famili P, Cauley JA, Greenspan SL (2007) The effect of androgen deprivation therapy on periodontal disease in men with prostate cancer. J Urol 177:921–924
Engeland CG, Sabzehei B, Marucha PT (2009) Sex hormones and mucosal wound healing. Brain Behav Immun 23:629–635
Brusca MI, Verdugo F, Amighini C, Albaina O, Moragues MD (2014) Anabolic steroids affect human periodontal health and microbiota. Clin Oral Investig 18:1579–1586
Socransky SS, Haffajee AD (2005) Periodontal microbial ecology. Periodontol 38:135–187
Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL Jr (1998) Microbial complexes in subgingival plaque. J Clin Periodontol 25:134–144
Socransky SS, Haffajee AD (2002) Dental biofilms: difficult therapeutic targets. Periodontol 2000 28:12–55
Feres M, Figueiredo LC (2009) Current concepts in the microbial etiology and treatment of chronic periodontitis. J Int Acad Periodontol 11:234–249
Ozcelik O, Haytac MC, Seydaoglu G (2006) The effects of anabolic androgenic steroid abuse on gingival tissues. J Periodontol 77:1104–1109
Steffens JP, Wang X, Starr JR, Spolidorio LC, Van Dyke TE, Kantarci A (2015) Associations between sex hormone levels and periodontitis in men: results from NHANES III. J Periodontol 86:1116–1125
Steffens JP, Herrera BS, Coimbra LS, Stephens DN, Rossa C Jr, Spolidorio LC, Kantarci A, Van Dyke TE (2014) Testosterone regulates bone response to inflammation. Horm Metab Res 46:193–200
Steffens JP, Coimbra LS, Rossa C Jr, Kantarci A, Van Dyke TE, Spolidorio LC (2015) Androgen receptors and experimental bone loss - an in vivo and in vitro study. Bone 81:683–690
Nazar Majeed Z, Philip K, Alabsi AM, Pushparajan S, Swaminathan D (2016) Identification of gingival crevicular fluid sampling, analytical methods, and oral biomarkers for the diagnosis and monitoring of periodontal diseases: a systematic review. Dis Markers 2016:1804727
O'Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43:38
Socransky SS, Smith C, Martin L, Paster BJ, Dewhirst FE, Levin AE (1994) "Checkerboard" DNA-DNA hybridization. Biotechniques 17:788–792
Casarin RCV, Del Peloso RE, Mariano FS, Nociti FH Jr, Casati MZ, Gonçalves RB Levels of Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, inflammatory cytokines and species-specific immunoglobulin G in generalized aggressive and chronic periodontitis. J Periodontal Res 45:635–642
Duarte PM, de Mendonca AC, Maximo MB, Santos VR, Bastos MF, Nociti FH (2009) Effect of anti-infective mechanical therapy on clinical parameters and cytokine levels in human peri-implant diseases. J Periodontol 80:234–243
Mariotti A, Mawhinney M (2013) Endocrinology of sex steroid hormones and cell dynamics in the periodontium. Periodontol 2000 61:69–88
de Paiva Goncalves V, Ortega AAC, Steffens JP, Spolidorio DMP, Rossa C, Spolidorio LC (2018) Long-term testosterone depletion attenuates inflammatory bone resorption in the ligature-induced periodontal disease model. J Periodontol 89:466–475
Mogi M, Otogoto J, Ota N, Inagaki H, Minami M, Kojima K (1999) Interleukin 1 beta, interleukin 6, beta 2-microglobulin, and transforming growth factor-alpha in gingival crevicular fluid from human periodontal disease. Arch Oral Biol 44:535–539
Rawlinson A, Dalati MH, Rahman S, Walsh TF, Fairclough AL (2000) Interleukin-1 and IL-1 receptor antagonist in gingival crevicular fluid. J Clin Periodontol 27:738–743
Graves DT, Oates T, Garlet GP (2011) Review of osteoimmunology and the host response in endodontic and periodontal lesions. J Oral Microbiol 3. https://doi.org/10.3402/jom.v3i0.5304
Thunell DH, Tymkiw KD, Johnson GK, Joly S, Burnell KK, Cavanaugh JE, Brogden KA, Guthmiller JM (2010) A multiplex immunoassay demonstrates reductions in gingival crevicular fluid cytokines following initial periodontal therapy. J Periodontal Res 45:148–152
Lamster IB, Oshrain RL, Gordon JM (1986) Enzyme activity in human gingival crevicular fluid: considerations in data reporting based on analysis of individual crevicular sites. J Clin Periodontol 13:799–804
Nakashima K, Demeurisse C, Cimasoni G (1994) The recovery efficiency of various materials for sampling enzymes and polymorphonuclear leukocytes from gingival crevices. J Clin Periodontol 21:479–483
Ataoglu H, Alptekin NO, Haliloglu S, Gursel M, Ataoglu T, Serpek B, Durmus E (2002) Interleukin-1beta, tumor necrosis factor-alpha levels and neutrophil elastase activity in peri-implant crevicular fluid. Clin Oral Implants Res 13:470–476
Lages EJP, Costa FO, Cortelli SC, Cortelli JR, Cota LOM, Cyrino RM, Lages BEM, Nobre-Franco GC, Brito JAR, Gomez RS Alcohol consumption and periodontitis: qualification of periodontal pathogens and cytokines. J Periodontol 86:1058–1068
Acknowledgments
We are thankful to Mr. Gabriel Guidio Guarenghi and Ms. Taize Franciele Massignani Figueredo for their technical support.
Funding
This study was partially supported by the Coordination for the Improvement of Higher Education Personnel (CAPES, Brasília, DF, Brazil). SVSCW was a recipient of a CAPES scholarship and JDPC was a beneficiary of a scholarship from the Araucária Foundation for Scientific and Technological Development Support of the State of Paraná (Curitiba, PR, Brazil).
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to conception and design of the study. SVSCW, HMV, TBCC, and JDPC worked on the acquisition and analysis of data. LCS, DMPS, MF, GSS, and JPS supervised all steps and worked on the analysis and interpretation of data. SVSCW, HMV, and JPS drafted the work and the other authors critically revised for intellectual content. All authors approved the final version and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
SVSCW declares that she has no conflict of interest. HMV declares that he has no conflict of interest. TBCC declares that she has no conflict of interest. JDPC declares that he has no conflict of interest. LCS declares that he has no conflict of interest. DMPS declares that she has no conflict of interest. MF declares that she has no conflict of interest. GMSS declares that she has no conflict of interest. JPS declares that he has no conflict of interest.
Ethical approval
All procedures were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
von Stein Cubas Warnavin, S., Valenga, H.M., Costa, T.B.C. et al. Periodontal clinical status, microbial profile, and expression of interleukin-1β in men under androgenic anabolic steroids abuse. Clin Oral Invest 25, 3567–3575 (2021). https://doi.org/10.1007/s00784-020-03679-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03679-6