Abstract
Objectives
This animal study was conducted to evaluate the osteocyte index in the peri-implant bone around immediately restored implants under static lateral overload.
Material and methods
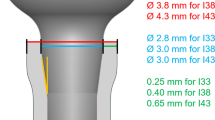
Seven mongrel dogs received three implants on each side of the mandible. Forty-two implants were distributed into three groups (14 implants per group); each animal received two implants connected to a 4.5-mm opened expansion device (experimental group); in the other mandible side, two implants were connected into an expansion device without activation (control group); one implant each side of the mandible was left submerged (unload group). After 4 months under daily mechanical and chemical plaque control, the animals were euthanized; dental implants and surrounding bone were removed and processed to obtain thin ground sections. Histomorphometry was used to evaluate the osteocyte index in the peri-implant bone contact to implant.
Results
A higher, statistically significant mean number of osteocytes × 10−5 μm2 (54.74 ± 23.91) was found in the control group compared with the test group (22.57 ± 22.55) (p = 0.0221). The correlation between percentage of bone-implant contact and osteocyte index for submerged implants was not statistically significant (p = 0.2667), whereas the value for immediately loaded implants was statistically significant (p = 0.0480).
Conclusion
The lower number of osteocytes in the peri-implant bone around overloaded implants could be related to the need for functional adaptation of the bone tissue to overloading and to the hypothesized involvement of the osteocytes in the maintenance of the bone matrix in the control group.
Clinical relevance
Osteocytes play a pivotal role in bone adaptation to mechanical loading, and the osteocyte network has been regarded as being the main mechanosensory mechanism.
Graphical Abstract





Similar content being viewed by others
References
Insua A, Monje A, Wang HL, Miron RJ (2017) Basis of bone metabolism around dental implants during osseointegration and peri-implant bone loss. J Biomed Mater Res A 105(7):2075–2089. https://doi.org/10.1002/jbm.a.36060
Shah FA, Thomsen P, Palmquist A (2018) A review of the impact of implant biomaterials on osteocytes. J Dent Res 97(9):977–986. https://doi.org/10.1177/0022034518778033
Barros RR, Degidi M, Novaes AB, Piattelli A, Shibli JA, Iezzi G (2009) Osteocyte density in the peri-implant bone of immediately loaded and submerged dental implants. J Periodontol 80(3):499–504. https://doi.org/10.1902/jop.2009.080484
Reijnders CM, Bravenboer N, Holzmann PJ, Bhoelan F, Blankenstein MA, Lips P (2007) In vivo mechanical loading modulates insulin-like growth factor binding protein-2 gene expression in rat osteocytes. Calcif Tissue Int 80(2):137–143. https://doi.org/10.1007/s00223-006-0077-4
Shibli JA, Mangano C, D'avila S, Piattelli A, Pecora GE, Mangano F, Onuma T, Cardoso LA, Ferrari DS, Aguiar KC, Iezzi G (2010) Influence of direct laser fabrication implant topography on type IV bone: a histomorphometric study in humans. J Biomed Mater Res A 93(2):607–614
Shiflett LA, Tiede-Lewis LM, Xie Y, Lu Y, Ray EC, Dallas SL (2019) Collagen dynamics during the process of osteocyte embedding and mineralization. Front Cell Dev Biol 7:178
McCutcheon S, Majeska RJ, Spray DC, Schaffler MB, Vazquez M (2020) Apoptotic osteocytes induce RANKL production in bystanders via purinergic signaling and activation of pannexin channels. J Bone Miner Res 35(5):966–977. https://doi.org/10.1002/jbmr.3954
Siddiqui JA, Partridge NC (2016) Physiological bone remodeling: systemic regulation and growth factor involvement. Physiology (Bethesda) 31(3):233–245
Bertolini MM, Del Bel Cury AA, Pizzoloto L, Acapa IRH, Shibli JA, Bordin D (2019) Does traumatic occlusal forces lead to peri-implant bone loss? A systematic review. Braz Oral Res 33(suppl 1):e069. https://doi.org/10.1590/1807-3107bor-2019.vol33.0069
Xiao W, Wang Y, Pacios S, Li S, Graves DT (2016) Cellular and molecular aspects of bone remodeling. Front Oral Biol 18:9–16
Jepsen S, Caton JG, Albandar JM, Bissada NF, Bouchard P, Cortellini P, Demirel K, de Sanctis M, Ercoli C, Fan J, Geurs NC, Hughes FJ, Jin L, Kantarci A, Lalla E, Madianos PN, Matthews D, McGuire MK, Mills MP, Preshaw PM, Reynolds MA, Sculean A, Susin C, West NX, Yamazaki K (2018) Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89(Suppl 1):S237–S248. https://doi.org/10.1002/JPER.17-0733
Ferrari DS, Piattelli A, Iezzi G, Faveri M, Rodrigues JA, Shibli JÁ (2015) Effect of lateral static load on immediately restored implants: histologic and radiographic evaluation in dogs. Clin Oral Implants Res 26(4):e51–e56. https://doi.org/10.1111/clr.12331
Cesaretti G, Lang NP, Viganò P, Bengazi F, Apaza Alccayhuaman KA, Botticelli D (2018) Immediate and delayed loading of fixed dental prostheses supported by single or two splinted implants: a histomorphometric study in dogs. J Oral Rehabil 45(4):308–316. https://doi.org/10.1111/joor.12612
Heitz-Mayfield LJ, Schmid B, Weigel C, Gerber S, Bosshardt DD, Jonsson J, Lang NP, Jonsson J (2004) Does excessive occlusal load affect osseointegration? An experimental study in the dog. Clin Oral Implants Res 15(3):259–268. https://doi.org/10.1111/j.1600-0501.2004.01019.x
Isidor F (1997) Histological evaluation of peri-implant bone at implants subjected to occlusal overload or plaque accumulation. Clin Oral Implants Res 8(1):1–9. https://doi.org/10.1111/j.1600-0501.1997.tb00001.x
Isidor F (1996) Loss of osseointegration caused by occlusal load of oral implants. A clinical and radiographic study in monkeys. Clin Oral Implants Res 7(2):143–152. https://doi.org/10.1034/j.1600-0501.1996.070208.x
Lima LA, Bosshardt DD, Chambrone L, Araújo MG, Lang NP (2019) Excessive occlusal load on chemically modified and moderately rough titanium implants restored with cantilever reconstructions. An experimental study in dogs. Clin Oral Implants Res 30(11):1142–1154. https://doi.org/10.1111/clr.13539
Bonewald LF, Johnson ML (2008) Osteocytes, mechanosensing and Wnt signaling. Bone. 42(4):606–615. https://doi.org/10.1016/j.bone.2007.12.224
Duyck J, Vandamme K, Geris L, van Oosterwyck H, de Cooman M, Vandersloten J, Puers R, Naert I (2006) The influence of micro-motion on the tissue differentiation around immediately loaded cylindrical turned titanium implants. Arch Oral Biol 51(1):1–9. https://doi.org/10.1016/j.archoralbio.2005.04.003
Vashishth D, Verborgt O, Divine G, Schaffler MB, Fyhrie DP (2000) Decline in osteocyte lacunar density in human cortical bone is associated with accumulation of microcracks with age. Bone. 26(4):375–380. https://doi.org/10.1016/S8756-3282(00)00236-2
Vashishth D, Gibson G, Kimura J, Schaffler MB, Fyhrie DP (2002) Determination of bone volume by osteocyte population. Anat Rec 267(4):292–295. https://doi.org/10.1002/ar.10114
Repp F, Kollmannsberger P, Roschger A, Kerschnitzki M, Berzlanovich A, Gruber GM, Roschger P, Wagermaier W, Weinkamer R (2017) Spatial heterogeneity in the canalicular density of the osteocyte network in human osteons. Bone Rep 6:101–108. Published 2017 Mar 15. https://doi.org/10.1016/j.bonr.2017.03.001
Adachi T, Aonuma Y, Tanaka M, Hojo M, Takano-Yamamoto T, Kamioka H (2009) Calcium response in single osteocytes to locally applied mechanical stimulus: differences in cell process and cell body. J Biomech 42(12):1989–1995. https://doi.org/10.1016/j.jbiomech.2009.04.034
Wang K, Le L, Chun BM et al (2019) A novel osteogenic cell line that differentiates into GFP-tagged osteocytes and forms mineral with a bone-like lacunocanalicular structure. J Bone Miner Res 34(6):979–995. https://doi.org/10.1002/jbmr.3720
Mullender MG, Tan SD, Vico L, Alexandre C, Klein-Nulend J (2005) Differences in osteocyte density and bone histomorphometry between men and women and between healthy and osteoporotic subjects. Calcif Tissue Int 77(5):291–296. https://doi.org/10.1007/s00223-005-0043-6
Lynch ME, van der Meulen MCH (2012) Mechanical properties of bone tissue. In: Çehreli M (ed) Biomechanics of dental implants. Handbook for researchers. Nova Science Publishers, Inc, New York, pp 1–20
Vandamme K, Naert I, Duyck J (2012) Animal experimental findings on the effect of mechanical load on peri-implant tissue differentiation and adaptation. In: Çehreli M (ed) Biomechanics of dental implants. Handbook for researchers. Nova Science Publishers, Inc, New York, pp 97–126
Traini T, Neugebauer J, Thams U, Zöller JE, Caputi S, Piattelli A (2009) Peri-implant bone organization under immediate loading conditions: collagen fiber orientation and mineral density analyses in the minipig model. Clin Implant Dent Relat Res 11(1):41–51. https://doi.org/10.1111/j.1708-8208.2008.00086.x
Gotfredsen K, Berglundh T, Lindhe J (2001) Bone reactions adjacent to titanium implants subjected to static load. A study in the dog (I). Clin Oral Implants Res 12(1):1–8
Berglundh T, Abrahamsson I, Lindhe J (2005) Bone reactions to longstanding functional load at implants: an experimental study in dogs. J Clin Periodontol 32(9):925–932
Puterman I, Kan JY, Rungcharassaeng K, Oyama K, Morimoto T, Lozada J (2012) Biological adaptation to misfits of immediately loaded fixed prostheses following computer-guided surgery. J Prosthodont 21(3):185–190
Jemt T, Lekholm U, Johansson CB (2000) Bone response to implant-supported frameworks with differing degrees of misfit preload: in vivo study in rabbits. Clin Implant Dent Relat Res 2(3):129–137. https://doi.org/10.1111/j.1708-8208.2000.tb00003.x
Pozzi A, Agliardi E, Tallarico M, Barlattani A (2012) Clinical and radiological outcomes of two implants with different prosthetic interfaces and neck configurations: randomized, controlled, split-mouth clinical trial. Clin Implant Dent Relat Res. https://doi.org/10.1111/j.1708-8208.2012.00465
Freitas-Júnior AC, Rocha EP, Bonfante EA et al (2012) Biomechanical evaluation of internal and external hexagon platform switched implant-abutment connections: an in vitro laboratory and three-dimensional finite element analysis. Dent Mater 28(10):218–228
Author information
Authors and Affiliations
Contributions
C. D. C, D. B, A. P, G. I, A.N., and J.A.S wrote the draft, conducted the experiment, collected data, and wrote the manuscript. J.A.S was the leader responsible for the conception and quality standards of the manuscript. All authors have approved the final version of this document.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international guidelines for the care and use of animals were complied with according to the Institutional Animal Care Guidelines of the University of Guarulhos and Veterinary School of University of Guarulhos, Guarulhos, SP, Brazil.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Calais, C.D., Bordin, D., Piattelli, A. et al. Lateral static overload on immediately restored implants decreases the osteocyte index in peri-implant bone: a secondary analysis of a pre-clinical study in dogs. Clin Oral Invest 25, 3297–3303 (2021). https://doi.org/10.1007/s00784-020-03662-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03662-1