Abstract
Objectives
To evaluate the mRNA expression levels of cytokines interferon-γ, tumour necrosis factor-α, interleukin IL-1β, IL-10, and the chemokine CCL2/MCP-1, CCL4, and CXCR4 in the periapical interstitial fluid from root canal infections before and after bacterial load reduction in patients undergoing haematopoietic stem cell transplantation (HSCT).
Materials and methods
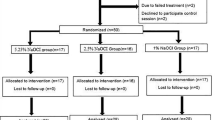
The case group was composed of 10 patients undergoing HSCT, and our control group included 10 healthy patients. Clinical samples were taken from teeth with pulp necrosis. Three paper points were placed in the RCS and maintained for 2 min for microbial evaluation before cleaning and shaping procedures. After cleaning and drying the canal, three paper points were introduced into the root canal, passing passively through the root apex (2 mm) into the periapical tissues for 1 min. Samples were collected immediately after root canal cleaning and 7 days later (restrained root canal bacterial load) to characterize gene expression using real-time PCR.
Results
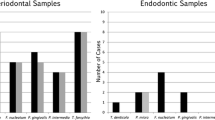
The results showed significantly reduction in the microbial load on day 7. An increased expression level of TNF-α and IFN-γ on day 7 in control and case groups was observed (p < 0.05). The mRNA levels of IL-1β and IL-10 in the pre-HSCT group increased in the samples from day 7 (p < 0.05). The chemokine CCL-2/MCP-1 was not detected in pre-HSCT group. Chemokine receptor CXCR4 levels increased in samples obtained from the day 7 in the control group (p < 0.05).
Conclusions
Individuals undergoing HSTC presented similar cytokine and chemokine mRNA expression compared with healthy individuals. However, it was observed the total absence of mRNA MCP-1/CCL2 expression in those individuals undergoing HSCT.
Clinical relevance
Patients undergoing HSCT are at higher risk of infection. No study has analysed the periapical immune responses to root canal infections in HSCT individuals.



Similar content being viewed by others
References
Haverman TM, Raber-Durlacher JE, Rademacher WM, Vokurka S, Epstein JB, Huisman C et al (2015) Oral complications in hematopoietic stem cell recipients: the role of inflammation. Mediat Inflamm 2014:378281
Forman SJ, Blume KG, Thomas ED (1999) Hematopoietic cell transplantation: Blackwell Science
de Brito LC, Teles FR, Teles RP, Totola AH, Vieira LQ, Sobrinho AP (2012) T-lymphocyte and cytokine expression in human inflammatory periapical lesions. J Endod 38:481–485
Bambirra W Jr, Maciel KF, Thebit MM, de Brito LCN, Vieira LQ, Sobrinho AP (2015) Assessment of apical expression of alpha-2 integrin, heat shock protein, and proinflammatory and immunoregulatory cytokines in response to endodontic infection. J Endod 41:1085–1090
Graves DT, Oates T, Garlet GP (2011) Review of osteoimmunology and the host response in endodontic and periodontal lesions. J Oral Microbiol 3
Romagnani S (2000) T-cell subsets (Th1 versus Th2). Ann Allergy Asthma Immunol 85:9–18
Sallusto F, Mackay CR, Lanzavecchia A (2000) The role of chemokine receptors in primary, effector, and memory immune responses. Annu Rev Immunol 18:593–620
Bryant VL, Slade CA (2015) Chemokines, their receptors and human disease: the good, the bad and the itchy. Immunol Cell Biol 93:364–371
Sviland L, Pearson AD, Green MA, Baker BD, Eastham EJ, Reid MM et al (1991) Immunopathology of early graft-versus-host disease--a prospective study of skin, rectum, and peripheral blood in allogeneic and autologous bone marrow transplant recipients. Transplantation 52:1029–1036
Siqueira JF, Alves FRF, Rôças IN (2011) Pyrosequencing analysis of the apical root canal microbiota. J Endod 37:1499–1503
Tavares WL, de Brito LC, Henriques LC, Teles FR, Teles RP, Vieira LQ et al (2012) Effects of calcium hydroxide on cytokine expression in endodontic infections. J Endod 38:1368–1371
Tavares WL, de Brito LC, Henriques LC, Oliveira RR, Maciel KF, Vieira LQ et al (2013) The impact of chlorhexidine-based endodontic treatment on periapical cytokine expression in teeth. J Endod 39:889–892
Henriques LC, de Brito LC, Tavares WL, Vieira LQ, Ribeiro Sobrinho AP (2011) Cytokine analysis in lesions refractory to endodontic treatment. J Endod 37:1659–1662
Barbosa Silva MJ, Vieira LQ, Sobrinho AP (2008) The effects of mineral trioxide aggregates on cytokine production by mouse pulp tissue. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:e70–e76
Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc 3:1101–1108
Greinix HT, Nachbaur D, Krieger O, Eibl M, Knobl P, Kalhs P et al (2002) Factors affecting long-term outcome after allogeneic haematopoietic stem cell transplantation for acute myelogenous leukaemia: a retrospective study of 172 adult patients reported to the Austrian stem cell transplantation registry. Br J Haematol 117:914–923
Fabricius L, Dahlen G, Holm SE, Moller AJ (1982) Influence of combinations of oral bacteria on periapical tissues of monkeys. Scand J Dent Res 90:200–206
Sundqvist GK, Eckerbom MI, Larsson AP, Sjogren UT (1979) Capacity of anaerobic bacteria from necrotic dental pulps to induce purulent infections. Infect Immun 25:685–693
Bakhshayesh M, Soleimani M, Mehdizadeh M, Katebi M (2012) Effects of TGF-beta and b-FGF on the potential of peripheral blood-borne stem cells and bone marrow-derived stem cells in wound healing in a murine model. Inflammation 35:138–142
Takeichi O, Saito I, Tsurumachi T, Moro I, Saito T (1996) Expression of inflammatory cytokine genes in vivo by human alveolar bone-derived polymorphonuclear leukocytes isolated from chronically inflamed sites of bone resorption. Calcif Tissue Int 58:244–248
Bradley JR (2008) TNF-mediated inflammatory disease. J Pathol 214:149–160
Wajant H, Pfizenmaier K, Scheurich P (2003) Tumor necrosis factor signaling. Cell Death Differ 10:45–65
Kwan Tat S, Padrines M, Theoleyre S, Heymann D, Fortun Y (2004) IL-6, RANKL, TNF-alpha/IL-1: interrelations in bone resorption pathophysiology. Cytokine Growth Factor Rev 15:49–60
Colic M, Lukic A, Vucevic D, Milosavljevic P, Majstorovic I, Marjanovic M et al (2006) Correlation between phenotypic characteristics of mononuclear cells isolated from human periapical lesions and their in vitro production of Th1 and Th2 cytokines. Arch Oral Biol 51:1120–1130
Braga-Diniz JM, Espaladori MC, Souza E, Silva ME, Brito LCN, Vieira LQ, Ribeiro Sobrinho AP (2019) Immunological profile of teeth with inflammatory periapical disease from chronic liver disease patients. J Endod 52:149–157
Maia LM, Espaladori MC, Diniz JMB, Tavares WLF, de Brito LCN, Vieira LQ, Sobrinho APR (2020) Clinical endodontic procedures modulate periapical cytokine and chemokine gene expressions. Clin Oral Investig. https://doi.org/10.1007/s00784-020-03247-y
de Brito LC, Teles FR, Teles RP, Nogueira PM, Vieira LQ, Ribeiro Sobrinho AP (2015) Immunological profile of periapical endodontic infections from HIV- and HIV+ patients. Int Endod J 48:533–541
Yamasaki M, Kumazawa M, Kohsaka T, Nakamura H (1994) Effect of methotrexate-induced neutropenia on rat periapical lesion. Oral Surg Oral Med Oral Pathol 77:655–661
Fouad AF (1997) IL-1 alpha and TNF-alpha expression in early periapical lesions of normal and immunodeficient mice. J Dent Res 76:1548–1554
Nair PN (2004) Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med 15:348–381
Stashenko P, Wang CY, Tani-Ishii N, Yu SM (1994) Pathogenesis of induced rat periapical lesions. Oral Surg Oral Med Oral Pathol 78:494–502
Ferreira SB, Tavares WL, Rosa MA, Brito LC, Vieira LQ, Martelli HJ et al (2016) Sickle cell anemia in Brazil: personal, medical and endodontic patterns. Braz Oral Res 30:01
Morsani JM, Aminoshariae A, Han YW, Montagnese TA, Mickel A (2011) Genetic predisposition to persistent apical periodontitis. J Endod 37:455–459
Silva TA, Garlet GP, Lara VS, Martins W Jr, Silva JS, Cunha FQ (2005) Differential expression of chemokines and chemokine receptors in inflammatory periapical diseases. Oral Microbiol Immunol 20:310–316
Kim MS, Day CJ, Selinger CI, Magno CL, Stephens SR, Morrison NA (2006) MCP-1-induced human osteoclast-like cells are tartrate-resistant acid phosphatase, NFATc1, and calcitonin receptor-positive but require receptor activator of NFkappaB ligand for bone resorption. J Biol Chem 281:1274–1285
Graves DT, Jiang Y, Valente AJ (1999) Regulated expression of MCP-1 by osteoblastic cells in vitro and in vivo. Histol Histopathol 14:1347–1354
Yano S, Yanagawa H, Nishioka Y, Mukaida N, Matsushima K, Sone S (1996) T helper 2 cytokines differently regulate monocyte chemoattractant protein-1 production by human peripheral blood monocytes and alveolar macophages. J Immunol 157:2660–2665
Olszyna DP, De Jonge E, Dekkers PE, van Deventer SJ, van der Poll T (2000) Interleukin 10 inhibits the release of CC chemokines during human endotoxemia. J Infect Dis 181:613–620
Cui S, Gao Y, Zhang L, Wang Y, Zhang L, Liu P, Liu L, Chen J (2017) Combined use of serum MCP-1/IL-10 ratio and uterine artery Doppler index significantly improves the prediction of preeclampsia. Clin Chim Acta 473:228–236
Low QE, Drugea IA, Duffner LA, Quinn DG, Cook DN, Rollins BJ et al (2001) Wound healing in MIP-1alpha(−/−) and MCP-1(−/−) mice. Am J Pathol 159:457–463
Saini V, Marchese A, Majetschak M (2010) CXC chemokine receptor 4 is a cell surface receptor for extracellular ubiquitin. J Biol Chem 285:15566–15576
Majetschak M (2011) Extracellular ubiquitin: immune modulator and endogenous opponent of damage-associated molecular pattern molecules. J Leukoc Biol 89:205–219
Eskdale J, Kube D, Tesch H, Gallagher G (1997) Mapping of the human IL-10 gene and further characterization of the 5’flanking sequence. Immunogenetics 46:120–128
Bazzoni F, Tamassia N, Rossato M, Cassatella MA (2010) Understanding the molecular mechanisms of the multifaceted IL-10-mediated anti-inflammatory response: lessons from neutrophils. Eur J Immunol 40:2360–2368
Sasaki H, Okamatsu Y, Kawai T, Kent R, Taubman M, Stashenko P (2004) The interleukin-10 knockout mouse is highly susceptible to Porphyromonas gingivalis-induced alveolar bone loss. J Periodontal Res 39:432–441
Acknowledgements
The authors also wish to thank the post-graduate programme at the School of Dentistry of UFMG. LQV and APRS are CNPq fellows.
Funding
The work was supported by the Fundação de Amparo a Pesquisa do Estado de Minas Gerais (FAPEMIG), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (the Research Ethics Committee of the Federal University of Minas Gerais-CAAE: 54829414.7.0000.5149) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Braga Diniz, J.M., Espaladori, M.C., e Souza Silva, M.E. et al. Immunological profile of periapical endodontic infection in patients undergoing haematopoietic transplantation. Clin Oral Invest 25, 1403–1410 (2021). https://doi.org/10.1007/s00784-020-03448-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03448-5