Abstract
Objectives
The aim of this study was to test the fracture load of ceramic and composite three-unit full-contour fixed dental prostheses (FDPs) fabricated with additive and subtractive computer-aided design (CAD)/computer-aided manufacturing (CAM) technology.
Materials and methods
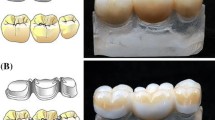
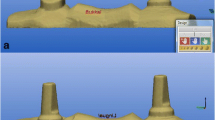
A newly developed alveolar socket replica model for a three-unit FDP replacing one molar was used in this study. Five CAD/CAM materials were used for fabrication of three-unit FDPs (each n = 12). The subtractive CAD/CAM fabrication method was used for groups BC (BRILLIANT Crios), TC (Telio CAD), EX (e.max CAD), and TZ (inCoris TZI C), and the additive method was used for group 3D (els 3D resin even stronger). FDPs were adhesively seated to the abutment dies (PANAVIA V5 system). Thermomechanical loading was performed prior to fracture testing with a universal testing machine. The data for maximum fracture load values was analyzed with one-way ANOVA and post hoc Scheffé test (α = 0.05).
Results
All FDPs survived the thermomechanical loading test. Statistically significant differences were found for the fracture load of three-unit FDPs fabricated from different CAD/CAM materials (p < 0.05). The highest mean fracture load was found for group TZ (2099.5 ± 382.1 N). Group 3D showed the lowest mean fracture load (928.9 ± 193.8 N). Group BC performed statistically significantly differently from group 3D with a mean fracture load of 1494.8 ± 214.5 N (p < 0.05).
Conclusions
Particle-filled composite resin CAD/CAM materials showed fracture load values within the range of ceramic materials with a specific indication of use for three-unit FDPs.
Clinical relevance
Particle filled composite CAD/CAM materials may offer new treatment possibilities for the CAD/CAM workflow.

Similar content being viewed by others
References
Yamashita J, Wang Q, Dechow PC (2006) Biomechanical effects of fixed partial denture therapy on strain patterns of the mandible. J Prosthet Dent 95:55–62
Walton TR (2015) An up-to-15-year comparison of the survival and complication burden of three-unit tooth-supported fixed dental prostheses and implant-supported single crowns. Int J Oral Maxillofac Implants 30:851–861
Poggio CE, Ercoli C, Rispoli K, Maiorana C, Esposito M (2017) Metal-free materials for fixed prosthodontic restorations. Cochrane Database Syst Rev (12):Cd009606
Kerschbaum T, Haastert B, Marinello CP (1996) Risk of debonding in three-unit resin-bonded fixed partial dentures. J Prosthet Dent 75:248–253
De Backer H, Van Maele G, De Moor N, Van den Berghe L (2006) Single-tooth replacement: is a 3-unit fixed partial denture still an option? A 20-year retrospective study. Int J Prosthodont 19:567–573
Kern M, Sasse M, Wolfart S (2012) Ten-year outcome of three-unit fixed dental prostheses made from monolithic lithium disilicate ceramic. J Am Dent Assoc 143:234–240
Pelaez J, Cogolludo PG, Serrano B, Lozano JF, Suarez MJ (2012) A prospective evaluation of zirconia posterior fixed dental prostheses: three-year clinical results. J Prosthet Dent 107:373–379
Reich S, Endres L, Weber C, Wiedhahn K, Neumann P, Schneider O, Rafai N, Wolfart S (2014) Three-unit CAD/CAM-generated lithium disilicate FDPs after a mean observation time of 46 months. Clin Oral Investig 18:2171–2178
Yang Y, Yu J, Gao J, Guo J, Li L, Zhao Y, Zhan S (2016) Clinical outcomes of different types of tooth-supported bilayer lithium disilicate all-ceramic restorations after functioning up to 5 years: a retrospective study. J Dent 51:56–61
Wolfart S, Eschbach S, Scherrer S, Kern M (2009) Clinical outcome of three-unit lithium-disilicate glass-ceramic fixed dental prostheses: up to 8 years results. Dent Mater 25:e63–e71
Land MF, Hopp CD (2010) Survival rates of all-ceramic systems differ by clinical indication and fabrication method. J Evid Based Dent Pract 10:37–38
Beuer F, Steff B, Naumann M, Sorensen JA (2008) Load-bearing capacity of all-ceramic three-unit fixed partial dentures with different computer-aided design (CAD)/computer-aided manufacturing (CAM) fabricated framework materials. Eur J Oral Sci 116:381–386
Ruse ND, Sadoun MJ (2014) Resin-composite blocks for dental CAD/CAM applications. J Dent Res 93:1232–1234
Wiegand A, Stucki L, Hoffmann R, Attin T, Stawarczyk B (2015) Repairability of CAD/CAM high-density PMMA- and composite-based polymers. Clin Oral Investig 19:2007–2013
Pfeilschifter M, Preis V, Behr M, Rosentritt M (2018) Edge strength of CAD/CAM materials. J Dent 74:95–100
Zimmermann M, Mehl A, Reich S (2013) New CAD/CAM materials and blocks for chairside procedures. Int J Comput Dent 16:173–181
Giordano R (2006) Materials for chairside CAD/CAM-produced restorations. J Am Dent Assoc 137 Suppl:14s–21s
Zimmermann M, Ender A, Egli G, Özcan M, Mehl A (2018) Fracture load of CAD/CAM-fabricated and 3D-printed composite crowns as a function of material thickness. Clin Oral Investig 23:2777–2784. https://doi.org/10.1007/s00784-018-2717-2
Rosentritt M, Behr M, Lang R, Handel G (2004) Flexural properties of prosthetic provisional polymers. Eur J Prosthodont Restor Dent 12:75–79
Edelhoff D, Schraml D, Eichberger M, Stawarczyk B (2016) Comparison of fracture loads of CAD/CAM and conventionally fabricated temporary fixed dental prostheses after different aging regimens. Int J Comput Dent 19:101–112
Behr M, Rosentritt M, Handel G (2003) Fiber-reinforced composite crowns and FPDs: a clinical report. Int J Prosthodont 16:239–243
Shi L, Fok AS (2009) Structural optimization of the fibre-reinforced composite substructure in a three-unit dental bridge. Dent Mater 25:791–801
Erkmen E, Meric G, Kurt A, Tunc Y, Eser A (2011) Biomechanical comparison of implant retained fixed partial dentures with fiber reinforced composite versus conventional metal frameworks: a 3D FEA study. J Mech Behav Biomed Mater 4:107–116
Keilig L, Stark H, Bourauel C (2016) Does the material stiffness of novel high-performance polymers for fixed partial dentures influence their biomechanical behavior? Int J Prosthodont 30:595–597
Krejci I, Reich T, Lutz F, Albertoni M (1990) An in vitro test procedure for evaluating dental restoration systems. 1. A computer-controlled mastication simulator. Schweiz Monatsschr Zahnmed 100:953–960
Tortopidis D, Lyons MF, Baxendale RH, Gilmour WH (1998) The variability of bite force measurement between sessions, in different positions within the dental arch. J Oral Rehabil 25:681–686
Lyons MF, Cadden SW, Baxendale RH, Yemm R (1996) Twitch interpolation in the assessment of the maximum force-generating capacity of the jaw-closing muscles in man. Arch Oral Biol 41:1161–1168
Özcan M, Jonasch M (2018) Effect of cyclic fatigue tests on aging and their translational implications for survival of all-ceramic tooth-borne single crowns and fixed dental prostheses. J Prosthodont 27:364–375
Stawarczyk B, Ender A, Trottmann A, Özcan M, Fischer J, Hämmerle CH (2012) Load-bearing capacity of CAD/CAM milled polymeric three-unit fixed dental prostheses: effect of aging regimens. Clin Oral Investig 16:1669–1677
Blackburn C, Rask H, Awada A (2018) Mechanical properties of resin-ceramic CAD-CAM materials after accelerated aging. J Prosthet Dent 119:954–958
Plengsombut K, Brewer JD, Monaco EA Jr, Davis EL (2009) Effect of two connector designs on the fracture resistance of all-ceramic core materials for fixed dental prostheses. J Prosthet Dent 101:166–173
Oh W, Gotzen N, Anusavice KJ (2002) Influence of connector design on fracture probability of ceramic fixed-partial dentures. J Dent Res 81:623–627
Vult von Steyern P, Kokubo Y, Nilner K (2005) Use of abutment-teeth vs. dental implants to support all-ceramic fixed partial dentures: an in-vitro study on fracture strength. Swed Dent J 29:53–60
Wimmer T, Ender A, Roos M, Stawarczyk B (2013) Fracture load of milled polymeric fixed dental prostheses as a function of connector cross-sectional areas. J Prosthet Dent 110:288–295
Choi JW, Kim SY, Bae JH, Bae EB, Huh JB (2017) In vitro study of the fracture resistance of monolithic lithium disilicate, monolithic zirconia, and lithium disilicate pressed on zirconia for three-unit fixed dental prostheses. J Adv Prosthodont 9:244–251
Rosentritt M, Plein T, Kolbeck C, Behr M, Handel G (2000) In vitro fracture force and marginal adaptation of ceramic crowns fixed on natural and artificial teeth. Int J Prosthodont 13:387–391
Guess PC, Schultheis S, Wolkewitz M, Zhang Y, Strub JR (2013) Influence of preparation design and ceramic thicknesses on fracture resistance and failure modes of premolar partial coverage restorations. J Prosthet Dent 110:264–273
Wimmer T, Erdelt KJ, Eichberger M, Roos M, Edelhoff D, Stawarzak B (2014) Influence of abutment model materials on the fracture loads of three-unit fixed dental prostheses. Dent Mater J 33:717–724
Rosentritt M, Behr M, Gebhard R, Handel G (2006) Influence of stress simulation parameters on the fracture strength of all-ceramic fixed-partial dentures. Dent Mater 22:176–182
Kinney JH, Marshall SJ, Marshall GW (2003) The mechanical properties of human dentin: a critical review and re-evaluation of the dental literature. Crit Rev Oral Biol Med 14:13–29
Ho SP, Kurylo MP, Fong TK, Lee SS, Wagner HD, Ryder MI, Marshall GW (2010) The biomechanical characteristics of the bone-periodontal ligament-cementum complex. Biomaterials 31(25):6635–6646
Scherrer SS, de Rijk WG, Belser UC, Meyer JM (1994) Effect of cement film thickness on the fracture resistance of a machinable glass-ceramic. Dent Mater 10:172–177
Wimmer T, Erdelt KJ, Raith S, Schneider JM, Stawarczyk B, Beuer F (2014) Effects of differing thickness and mechanical properties of cement on the stress levels and distributions in a three-unit zirconia fixed prosthesis by FEA. J Prosthodont 23:358–366
Reymus M, Roos M, Eichberger M, Edelhoff D, Hickel R, Stawarczyk B (2019) Bonding to new CAD/CAM resin composites: influence of air abrasion and conditioning agents as pretreatment strategy. Clin Oral Investig 23:529–538
Mormann WH, Stawarczyk B, Ender A, Sener B, Attin T, Mehl A (2013) Wear characteristics of current aesthetic dental restorative CAD/CAM materials: two-body wear, gloss retention, roughness and Martens hardness. J Mech Behav Biomed Mater 20:113–125
Funding
The work was supported by the Division of Computerized Restorative Dentistry, Center of Dental Medicine, University of Zurich, which was in part financially supported by Saremco Dental AG and Coltène AG to conduct the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Disclaimer
Both companies had no influence in the study design, nor in the collection, analysis, or interpretation of the data, nor in writing or submitting the publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zimmermann, M., Ender, A., Attin, T. et al. Fracture load of three-unit full-contour fixed dental prostheses fabricated with subtractive and additive CAD/CAM technology. Clin Oral Invest 24, 1035–1042 (2020). https://doi.org/10.1007/s00784-019-03000-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03000-0