Abstract
Objectives
This study aims to determine the effectiveness of a messaging app (WeChat) in improving patients’ compliance and reducing the duration of orthodontic treatment (DOT).
Materials and methods
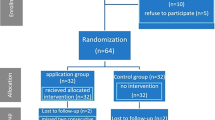
A randomized controlled trial was performed in a dental hospital and a clinic from August 2012 to May 2015. Orthodontic patients were included at the beginning of treatment. Patients with multiphase treatment or braceless technique were excluded. Participants were randomized to WeChat group (received regular reminders and educational messages) or control group (received conventional management) and were followed up until the treatment was completed. Primary outcome measure was DOT. Others were late and failed attendance, bracket bond failure, and oral hygiene condition.
Results
One hundred twelve patients in each group participated and completed the trial. DOT in WeChat group were 7.3 weeks shorter (P = 0.007). There were less failed attendance (3.1 vs. 10.9 %, P < 0.001), late attendance (20.1 vs. 29.9 %, P < 0.001), and bracket bond failure (11.8 vs. 16.1 %, P < 0.001) in WeChat group than control. There was no difference in orthodontic plaque index nor modified gingivitis index between the two groups before and after treatment. Number of failed attendances was identified as an independent factor affecting DOT (P = 0.004; HR = 0.89, 95 % CI 0.84 to 0.95).
Conclusions
The intervention with WeChat is effective in reducing the treatment duration and bracket bond failure, and improving the attendance in orthodontic patients.
Clinical relevance
DOT can be reduced by improving patient’s compliance. The messaging app is useful for outpatient education and management.




Similar content being viewed by others
References
Skidmore KJ, Brook KJ, Thomson WM, Harding WJ (2006) Factors influencing treatment time in orthodontic patients. Am J Orthod Dentofacial Orthop 129 (2):230–238. doi:http://dx.doi.org/10.1016/j.ajodo.2005.10.003
Palomares NB, Celeste RK, Oliveira BHd, Miguel JAM (2012) How does orthodontic treatment affect young adults’ oral health-related quality of life? Am J Orthod Dentofacial Orthop 141 (6):751–758. doi:http://dx.doi.org/10.1016/j.ajodo.2012.01.015
Shia GJ (1986) Treatment overruns. J Clin Orthod 20(9):602–604
Turbill EA, Richmond S, Wright JL (2001) The time-factor in orthodontics: what influences the duration of treatments in national health service practices? Community Dent Oral Epidemiol 29(1):62–72
Mavreas D, Athanasiou AE (2008) Factors affecting the duration of orthodontic treatment: a systematic review. Eur J Orthod 30(4):386–395. doi:10.1093/ejo/cjn018
Beckwith FR, Ackerman Jr RJ, Cobb CM, Tira DE (1999) An evaluation of factors affecting duration of orthodontic treatment. Am J Orthod Dentofac Orthop 115(4):439–447
Robb SI, Sadowsky C, Schneider BJ, BeGole EA (1998) Effectiveness and duration of orthodontic treatment in adults and adolescents. Am J Orthod Dentofacial Orthop 114 (4):383–386. doi:http://dx.doi.org/10.1016/S0889-5406(98)70182–9
Ma W, Xu T-M (2009) An evaluation of factors influencing orthodontic treatment duration. J Orthod 16(3):147–150. doi:10.3760/cma.j.issn.1674-5760.2009.03.007
Loke S, Tan S (2012) Factors influencing duration of orthodontic treatment: a 12-year retrospective study. Malays Dent J 34(2):16–30
de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R (2012) Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev 12:CD007459. doi:10.1002/14651858.CD007459.pub2
Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X (2008) Interventions for enhancing medication adherence. Cochrane Database Syst Rev 2:CD000011. doi:10.1002/14651858.CD000011.pub3
Logan AG, McIsaac WJ, Tisler A, Irvine MJ, Saunders A, Dunai A, Rizo CA, Feig DS, Hamill M, Trudel M, Cafazzo JA (2007) Mobile phone-based remote patient monitoring system for management of hypertension in diabetic patients. Am J Hypertens 20(9):942–948. doi:10.1016/j.amjhyper.2007.03.020
Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, Jack W, Habyarimana J, Sadatsafavi M, Najafzadeh M, Marra CA, Estambale B, Ngugi E, Ball TB, Thabane L, Gelmon LJ, Kimani J, Ackers M, Plummer FA (2010) Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet 376(9755):1838–1845. doi:10.1016/S0140-6736(10)61997-6
Reekie D, Devlin H (1998) Preventing failed appointments in general dental practice: a comparison of reminder methods. Br Dent J 185(9):472–474. doi:10.1038/sj.bdj.4809840
Can S, Macfarlane T, O’Brien KD (2003) The use of postal reminders to reduce non-attendance at an orthodontic clinic: a randomised controlled trial. Br Dent J 195(4):199–201 discussion 196. doi:10.1038/sj.bdj.4810443
Thomas D (2004) Postal reminders can improve attendance at orthodontic clinics. Evid Based Dent 5(1):14. doi:10.1038/sj.ebd.6400244
Prasad S, Anand R (2012) Use of mobile telephone short message service as a reminder: the effect on patient attendance. Int Dent J 62(1):21–26. doi:10.1111/j.1875-595X.2011.00081.x
Roth JP, Kula Jr TJ, Glaros A, Kula K (2004) Effect of a computer-generated telephone reminder system on appointment attendance. Semin Orthod 10 (3):190–193. doi:http://dx.doi.org/10.1053/j.sodo.2004.05.001
Nelson TM, Berg JH, Bell JF, Leggott PJ, Seminario AL (2011) Assessing the effectiveness of text messages as appointment reminders in a pediatric dental setting. J Am Dent Assoc 142(4):397–405
Brent Bowen T, Rinchuse DJ, Zullo T, DeMaria ME (2015) The influence of text messaging on oral hygiene effectiveness. Angle Orthod 85(4):543–548. doi:10.2319/071514-495.1
Eppright M, Shroff B, Best AM, Barcoma E, Lindauer SJ (2014) Influence of active reminders on oral hygiene compliance in orthodontic patients. Angle Orthod 84(2):208–213. doi:10.2319/062813-481.1
Jejurikar H, Nene S, Kalia A, Gupta G, Mirdehghan N (2014) Does text messaging reminder help in the orthodontic compliance of patients to maintain their oral hygiene. Oral Hyg Health 2(5):152
Hashemian TS, Kritz-Silverstein D, Baker R (2015) Text2Floss: the feasibility and acceptability of a text messaging intervention to improve oral health behavior and knowledge. J Public Health Dent 75(1):34–41. doi:10.1111/jphd.12068
Sharma R, Hebbal M, Ankola AV, Murugabupathy V (2011) Mobile-phone text messaging (SMS) for providing oral health education to mothers of preschool children in Belgaum city. J Telemed Telecare 17(8):432–436. doi:10.1258/jtt.2011.110416
Distribution of WeChat users in China as of January 2015, by age. http://www.statista.com/statistics/387658/wechat-china-user-age/. Accessed 21 June 2015
Wikipedia contributors (2015) WeChat. Wikipedia, The Free Encyclopedia. https://en.wikipedia.org/w/index.php?title=WeChat&oldid=675897795. Accessed 25 July 2015
Tencent (2015) Tencent Announces 2015 Second Quarter and Interim Results. http://www.tencent.com/en-us/content/ir/news/2015/attachments/20150812.pdf. Accessed 12 August 2015
Xiang T (2015) WeChat Reaches 1.1B Registered Accounts, with 440 M Regular Users. http://technode.com/2015/01/22/wechat-reaches-1-1b-registered-accounts-440m-mau/. Accessed 25 July 2015
Tencent (2015) WeChat - Features. http://www.wechat.com/en/features.html. Accessed 25 July 2015
Tencent (2015) What is WeChat Official Account Admin Platform? https://admin.wechat.com/cgi-bin/readtemplate?t=news/en_faq_tmpl&type=info&lang=en_US. Accessed 1 Aug 2015
Zotti F, Dalessandri D, Salgarello S, Piancino M, Bonetti S, Visconti L, Paganelli C (2015) Usefulness of an app in improving oral hygiene compliance in adolescent orthodontic patients. Angle Orthod. doi:10.2319/010915-19.1
Paschos E, Bucher K, Huth KC, Crispin A, Wichelhaus A, Dietl T (2014) Is there a need for orthodontic plaque indices?–diagnostic accuracy of four plaque indices. Clin Oral Investig 18(4):1351–1358. doi:10.1007/s00784-013-1076-2
Beberhold K, Sachse-Kulp A, Schwestka-Polly R, Hornecker E, Ziebolz D (2012) The orthodontic plaque index: an oral hygiene index for patients with multibracket appliances. Orthodontics (Chic) 13(1):94–99
Lobene RR (1986) Discussion: current status of indices for measuring gingivitis. J Clin Periodontol 13(5):381–382. doi:10.1111/j.1600-051X.1986.tb01478.x
Rebelo MAB, ACad Q (2011) Gingival indices: state of art. In: Panagakos FS (ed) Gingival diseases - their aetiology. Prevention and Treatment. InTech, Rijeka, pp. 41–54
Bos A, Hoogstraten J, Prahl-Andersen B (2005) Failed appointments in an orthodontic clinic. Am J Orthod Dentofac Orthop 127(3):355–357. doi:10.1016/j.ajodo.2004.11.014
Richardson A (1998) Failed appointments in an academic orthodontic clinic. Br Dent J 184(12):612–615. doi:10.1038/sj.bdj.4809709
Trenouth MJ (2003) Do failed appointments lead to discontinuation of orthodontic treatment? Angle Orthod 73(1):51–55. doi:10.1043/0003-3219(2003)073<0051:DFALTD>2.0.CO;2
Murdock A, Rodgers C, Lindsay H, Tham TC (2002) Why do patients not keep their appointments? Prospective study in a gastroenterology outpatient clinic. J R Soc Med 95(6):284–286
AlSadhan SA (2013) Frequency of missed and cancelled appointments in King Saud University orthodontic clinic. King Saud Univ J Dental Sci 4 (2):77–80. doi:http://dx.doi.org/10.1016/j.ksujds.2013.04.001
Neal RD, Hussain-Gambles M, Allgar VL, Lawlor DA, Dempsey O (2005) Reasons for and consequences of missed appointments in general practice in the UK: questionnaire survey and prospective review of medical records. BMC Fam Pract 6:47. doi:10.1186/1471-2296-6-47
Al-Wahadni A, Al Hamad KQ, Al-Tarawneh A (2006) Foreign body ingestion and aspiration in dentistry: a review of the literature and reports of three cases. Dent Update 33(9):561–562 564–566, 569–570
Petracci E, Farella M, Galeone C, Albano A, Ferraroni M, Decarli A (2009) Survival analysis with clustered observations of orthodontic brackets. Stat Med 28(28):3483–3491. doi:10.1002/sim.3641
Ahangar Atashi MH, Shahamfar M (2013) Long-term evaluation of clinical performance of direct-bonded brackets: an epidemiologic survey. J Contemp Dent Pract 14(4):738–742
Sukhia HR, Sukhia RH, Mahar A (2011) Bracket De-bonding & breakage prevalence in orthodontic patients. Pak Oral Dent J 31(1):71–75
Hwang D-H, Yun H-K, Hwang T-Y (2014) Knowledge and Self Care behaviors of orthodontic patients using clear aligner. J Korean Soc Dent Hyg 14(4):539–545
Jones H, Edwards L, Vallis TM, Ruggiero L, Rossi SR, Rossi JS, Greene G, Prochaska JO, Zinman B, Diabetes Stages of Change S (2003) Changes in diabetes self-care behaviors make a difference in glycemic control: the diabetes stages of change (DiSC) study. Diabetes Care 26(3):732–737
Strömberg A, Martensson J, Fridlund B, Levin LA, Karlsson JE, Dahlstrom U (2003) Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: results from a prospective, randomised trial. Eur Heart J 24(11):1014–1023
Keyserling TC, Samuel-Hodge CD, Ammerman AS, Ainsworth BE, Henriquez-Roldan CF, Elasy TA, Skelly AH, Johnston LF, Bangdiwala SI (2002) A randomized trial of an intervention to improve self-care behaviors of African-American women with type 2 diabetes: impact on physical activity. Diabetes Care 25(9):1576–1583
Inglis SC, Clark RA, McAlister FA, Stewart S, Cleland JG (2011) Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: abridged Cochrane review. Eur J Heart Fail 13(9):1028–1040. doi:10.1093/eurjhf/hfr039
Lorig KR, Holman H (2003) Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 26(1):1–7
Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R, Car J (2013) Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev 12:CD007458. doi:10.1002/14651858.CD007458.pub3
Acknowledgments
The authors wish to thank Hai He for programming and maintaining the relating scripts and Li Ye, Lin Luo, and Ya-Xin Chen for contacting the participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Ethics Committee of State Key Laboratory of Oral Diseases, West China Stomatology Hospital, Chengdu, China, and was conducted in compliance with the Declaration of Helsinki. Written informed consent was obtained from the patients or their guardians prior to the study.
Conflicts of interests
The authors declare that they have no conflict of interest.
Funding
The authors declared that there were no financial support from any external source regarding the current study.
Rights and permissions
About this article
Cite this article
Li, X., Xu, ZR., Tang, N. et al. Effect of intervention using a messaging app on compliance and duration of treatment in orthodontic patients. Clin Oral Invest 20, 1849–1859 (2016). https://doi.org/10.1007/s00784-015-1662-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1662-6