Abstract
Chagas disease, caused by the protozoa Trypanosoma cruzi, continues to be a serious public health problem in Latin America, worsened by the limitations in its detection. Given the importance of developing new diagnostic methods for this disease, the present review aimed to verify the number of publications dedicated to research on peptides that demonstrate their usefulness in serodiagnosis. To this end, a bibliographic survey was conducted on the PubMed platform using the keyword “peptide” or “epitope” combined with “Chagas disease” or “Trypanosoma cruzi”; “diagno*” or “serodiagnosis” or “immunodiagnosis”, without period restriction. An increasing number of publications on studies employing peptides in ELISA and rapid tests assays was verified, which confirms the expansion of research in this field. It is possible to observe that many of the peptides tested so far originate from proteins widely used in the diagnosis of Chagas, and many of them are part of commercial tests developed. In this sense, as expected, promising results were obtained for several peptides when tested in ELISA, as many of them exhibited sensitivity and specificity values above 90%. Furthermore, some peptides have been tested in several studies, confirming their diagnostic potential. Despite the promising results observed, it is possible to emphasize the need for extensive testing of peptides, using different serological panels, in order to confirm their potential. The importance of producing an effective assay capable of detecting the clinical stages of the disease, as well as new immunogenic antigens that enable new serological diagnostic tools for Chagas disease, is evident.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chagas disease (CD), a neglected tropical disease mainly associated with poverty, is caused by the hemoflagellate protozoan Trypanosoma cruzi (Chagas 1909). Parasite transmission can occur through several forms, including vectorial, congenital, oral, blood transfusion, and organ transplants (Bern et al. 2019). Of the 21 countries where CD is endemic, 17 managed to interrupt vector transmission in households throughout the countries, or in part of their national territories (PAHO/WHO 2023). However, effective monitoring of protozoan transmission is complex due to the zoonotic T. cruzi cycle (Shikanai-Yasuda and Carvalho 2012). The disease can cause severe visceral damage, involving damage to the heart (Nunes et al. 2018) and nervous system, as well as in the gastrointestinal tract (De Salazar et al. 2022; Forsyth et al. 2021; Rassi et al. 2010).
Although most cases are concentrated in Latin America, there is a notable increase in cases in non-endemic countries in North America, Europe and the Western Pacific regions, making CD a global public health problem, with great social impact (Lidani et al. 2019; Gómez-Ochoa et al. 2022). Some circumstances involved in the expansion of CD cases are related to the intensification of migratory movements, often motivated by social inequalities (Avaria et al. 2022; Marin-neto et al. 2023). Furthermore, changes in climatic and environmental factors favored the transmission of the parasite, as this directly influences its life cycle and geographic distribution (Medone et al., 2015). Furthermore, CD represents a major threat to public health worldwide as there are no adequate drugs for treatment or vaccines. Currently, the global amount spent on infected individuals is estimated at US$ 24 to 73 billion, with an annual value of US$ 4,660/person (Ferreira et al. 2022; Mucci et al. 2017; Lee et al. 2013). Despite these expenses, the population still faces many challenges regarding access to the healthcare system and the lack of subsidies to cope with the disease (Suárez et al. 2022). Currently, the disease affects 6 to 8 million people and causes 10,000 deaths per year, primarily in Latin American countries (WHO 2023). Among the countries reporting CD cases, Argentina, Bolivia, Brazil, Colombia, and Mexico are the ones with the highest prevalence (Medeiros et al. 2022). In Brazil, which has the third highest incidence rate in Latin America, it is estimated that there are approximately one million people infected with T. cruzi, representing one of the four main causes of death from infectious and parasitic diseases in the country (Brasil 2022).
The knowledge about T. cruzi life cycle and disease pathogenesis allowed the disease to be divided into an acute and a chronic phase (Suárez et al. 2022; Coura 2013; Segovia et al. 1916; Chagas 1909). The acute phase is characterized by a high parasitemia, occurrence and nonspecific symptoms where it is also possible to visualize parasites in the peripheral blood. The most appropriate methods for diagnosing the disease at this phase are direct and indirect parasitological tests, accompanied by serological tests (PAHO/WHO 2019). At this stage, diagnostic methods are still very time-consuming, demonstrating the importance of developing a differential serological test (SESPA 2023). However, indirect tests applied in the acute phase have low sensitivity and depend entirely on professional training, ending up not being a practical strategy. Furthermore, most cases go unnoticed due to the lack of specific symptoms and the fact that many individuals have little access to information (Schijman et al. 2022). Importantly, if CD can be identified early, the individual has a better chance of having good therapeutic responses and perhaps a satisfactory clinical evolution before the protozoan triggers irreversible complications and eventually becomes fatal (PAHO/WHO 2023).
The chronic phase can be symptomatic or asymptomatic, which will determine the strategies and diagnostic tests to be used (Schijman et al. 2022). Chronic individuals may present cardiovascular and/or gastrointestinal tract, and nervous system changes at different stages, which are the leading causes of death from the disease (Forsyth et al. 2021; Ledezma et al. 2020). The level of parasitemia in this phase decreases considerably, rendering the use of microscopic diagnosis an unreliable diagnostic method (Suárez et al. 2022). Serological tests are more often used as a diagnostic tool to achieve greater sensitivity and specificity (Balouz et al. 2017). Three conventional types of serological tests are approved by the WHO: (i) the enzyme-linked immunosorbent assay (ELISA); (ii) indirect immunofluorescence assay (IIF); and (iii) indirect hemagglutination assay (IHA) (Abras et al. 2022; PAHO/WHO 2019). The effectiveness of these available tests may vary, especially due to the different antigens applied and diagnostic confirmation for the chronic phase, following the guidelines of the Pan American Health Organization and the Centers for Disease Control (CDC), requires a positive result in at least two different tests and, in case of disagreement, a third test must be incorporated (PAHO/WHO 2019). Although serological tests are considered the gold standard for the diagnosis of chronic CD (PAHO/WHO 2019), the need to confirm the disease by at least two tests involves great effort in manufacturing reagents and is, therefore, expensive (Forsyth et al. 2021). It is of fundamental importance to incorporate an adequate diagnosis with high sensitivity and specificity to assist in surveillance actions aimed at preventing new cases (Santos et al. 2020).
Determining new biological markers that can provide preliminary recognition, as well as disease screening, is, thus, very useful (Mucci et al. 2017). The use of peptides has been reported in many studies as a resource for CD diagnosis, in addition to diagnosing other infectious diseases (Castiglione et al. 2022; Falconi-Agapito et al. 2022; Serena et al. 2022; Lorenzo et al. 2021; Li et al. 2020). Peptides consist of short portions of amino acids that have signaling capacity and essential biomolecules for various biological processes with high biomolecular recognition and high binding affinity for a wide range of specific targets (Apostolopoulos et al. 2021). Due to the potential of using peptides in CD diagnosis, in addition to the great interest of the diagnostic industry in the development and application of peptides in diagnostic kits, the focus of this review is a discussion on the studies that used peptides applied in ELISA assays and rapid tests as a tool for CD diagnosis.
Methodology
The search for was carried out using the PubMed database, including all papers published to April/2024. The descriptors used were: ((trypanosoma cruzi [Title/Abstract]) AND (imunodiagnosis[Title/Abstract])) AND (peptide[Title/Abstract]); ((trypanosoma cruzi [Title/Abstract]) AND (serodiagnosis[Title/Abstract])) AND (peptide[Title/Abstract]); ((trypanosoma cruzi[Title/Abstract]) AND (diagno*[Title/Abstract])) AND (peptide[Title/Abstract]); ((chagas disease [Title/Abstract]) AND (diagno*[Title/Abstract])) AND (peptide[Title/Abstract]); ((chagas disease [Title/Abstract]) AND (imunodiagnosis[Title/Abstract])) AND (peptide[Title/Abstract]); and ((chagas disease [Title/Abstract]) AND (serodiagnosis[Title/Abstract])) AND (peptide[Title/Abstract]). The selected articles were screened using inclusion and exclusion criteria, reviewed by two different readers. Animal articles, bibliographical reviews, case studies, epidemiological reviews, molecular and serological diagnoses of other diseases, editorials, duplicate articles, and articles related to other subjects were excluded. Only those articles employing ELISA or rapid test assays using peptides for CD diagnosis were included, regardless of whether there was a comparison with commercial tests or whether there was more than one test.
Peptides and their advantages as a diagnostic tool
Amino acids and peptides were mentioned for the first time in the nineteenth century (Vickery and Schmidt 1931; Hansen 2015). As a result, German chemists Hermann Emil Fischer and Franz Hofmeister developed an important study where they introduced several concepts about peptides and polypeptides (Fourneau and Fischer 1901; Wieland and Bodanszky 1991). Currently, peptides have applications in various health areas, such as diagnosis, vaccines, and therapy (Liu et al. 2022; Al-Azzam et al. 2020; Fisher et al. 2019; Link et al. 2017), and can be obtained through chemical synthesis and enzymatic hydrolysis (Akbarian et al. 2022). In addition, the use of peptides requires prior investigation that needs a global genomic and proteomic analysis of organisms (Pandey et al. 2021; Al-Azzam et al. 2020). To this end, different tactics have been developed to identify specific amino acid sequences within molecules of interest, including the phage display methodology (Zhang et al. 2022; Lechner et al. 2019; Piggott and Karuso 2016; Rangel et al. 2012) and bioinformatics analyses (Pandey et al. 2021).
Among the various applications, the use of peptides has shown great potential for disease diagnosis due to their sensitivity and specificity for different targets (Al-Azzam et al. 2020), offering more advantages when compared to the native antigen (Joshi et al. 2013; Saravanan et al. 2004). The use of peptides is important in clinical diagnosis because they are difficult to undergo variations, and can be easily manipulated, stored, and produced on a large scale. Peptides can be applied in several detection methods, such as lateral flow devices, and microarray or immunoenzymatic assay (ELISA), the latter being the most adopted diagnostic tool (Pandey et al. 2021). The post-pandemic effects of COVID-19, had repercussions on the need to develop new technologies for the mass production of effective diagnostic tools (Safiabadi Tali et al. 2021). Therefore, different peptides were tested and shown to be reactive with the serum of infected individuals (Cortés-Sarabia et al. 2022), reinforcing the importance of these molecules in the field of diagnostics. Furthermore, the use of peptides in immunodiagnosis has already shown promising results in numerous infectious diseases, such as strongyloidiasis, infectious bronchitis, blue tongue, and AIDS (Jackwood and Hilt 1995; Gonzalez et al. 1997; Feliciano et al. 2014; Saxena et al. 2012).
In fact, it is expected that the global peptide-based diagnostics market will grow by 9.6% from 2022 to 2027, with predictions of reaching a value of USD 11.4 billion (GME 2023). The use of peptides has been increasingly proposed to replace the customary methods that use recombinant proteins (Pandey et al. 2021). With this in mind, short peptides, containing more than eight amino acids, have several advantages when used in the detection of specific antibodies, as they facilitate synthesis, biodegradability, and biocompatibility, in addition to offering stability and economy, considering manufacturing costs are greater depending on the size of the amino acid sequence (Apostolopoulos et al. 2021; Brown et al. 1997). Therefore, use of peptides has proven to be very advantageous in detecting diseases and can significantly contribute to the management of healthcare systems and patient monitoring.
Peptide-based ELISA assays
ELISA was developed in 1971 by scientists Eva Engvall and Peter Perlmann (Engvall and Perlmann 1971), with the intention of validating the presence of molecules through antigen–antibody interaction. This discovery led to the technique being improved and gave rise to different types of ELISA that are now widely used in peptide and protein research, given that it is an extremely effective test (Aydin 2015; Engvall 2010). This method has been widely used in the investigation of new techniques to diagnose CD and with good results. At the moment, there are 20 studies in the literature using the peptide technique as a probable serological marker capable of replacing traditional methods, and the following topics summarize the results of each one.
A study published by Burns et al. (1992) was the first to use a peptide for CD diagnosis. The authors reported a repetitive peptide within an immunodominant T. cruzi protein. This peptide was obtained through chemical synthesis and its reactivity with positive serum samples was tested in an ELISA assay. For this purpose, 129 positive serum samples were used, in addition to 32 serum samples from healthy individuals as negative control. Results showed that synthetic TcD was recognized by 96.7% of the CD serum samples. Furthermore, only 3.3% of sera from non-Chagas individuals were reactive with the peptide. In addition, synthetic TcD was not identified by any sera from individuals with leishmaniasis. Moreover, the performance of the synthetic peptide was compared with that of a recombinant protein, where the synthetic peptide showed a comparable capacity to be recognized by positive serum samples, as well as displaying improved specificity.
Subsequently, Peralta et al. (1994) tested the mixture of two synthetic peptides from T. cruzi, called TcD, previously tested by Burns et al. (1992), and PEP2, obtained through chemical synthesis. The peptides were analyzed using a panel with 179 samples from infected individuals residing in a CD endemic area, as well as 81 serum samples from healthy individuals used as a negative control. Serum samples from individuals with other infectious diseases that might show cross-reaction with T. cruzi antigens were also used. When peptides were tested individually, the TcD and PEP2 sensitivity values were 93% and 91%, respectively. A mixture of both was evaluated and a sensitivity greater than 99% was observed. They also evaluated commercial tests IHA and IFA, using crude extract of T. cruzi, and obtained specificities of 99%, when using IHA, and 94%, when applying IFA.
Aznar et al. (1995) evaluated the diagnostic capacity of peptide R-13, corresponding to the C-terminal sequence of a T. cruzi ribosomal P protein, which was obtained through chemical synthesis. Serum from 161 Chagas individuals, 207 blood bank samples, and 20 serum samples from non-Chagas diseases were used to access peptide reactivity. Results indicated that 86% of congenital and 60% of chronic serum samples recognized R-13. Furthermore, all acute sera showed anti-T. cruzi IgM antibodies. However, R-13 was not recognized by serum samples from asymptomatic Chagas individuals or individuals with digestive symptoms. Moreover, 49% of serum samples from blood donors showed reactivity with R-13.
Later, Houghton et al. (1999) described the diagnostic use of two synthetic peptides, 2/D/E and TcLo1.2, which were obtained through chemical synthesis. To evaluate their reactivity, 240 positive samples from different geographic sources and 149 serum samples from healthy individuals were used. Results showed that the 2/D/E peptide demonstrated a sensitivity of 99.6% and a specificity of 9.33%. In relation to the TcLo1.2 peptide, a greater reactivity was observed with enhanced specificity for T. cruzi. A comparison was made between the specificities of the peptide and of T. cruzi lysate, where the TcLo1.2 peptide demonstrated a high degree of specificity.
Continuing the studies with 2/D/E-2 peptide, Betonico et al. (1999) evaluated its diagnostic capacity using 40 positive and 107 negative serum samples. Moreover, serum samples from non-Chagas individuals were also used to verify cross-reactions. The synthetic peptide was recognized by all serum samples from individuals with acute infection. However, when analyzing serum samples from individuals with chronic infection, only 12.9% of the serum samples reacted with the 2/D/E peptide. In addition, serum samples from healthy individuals and from non-Chagas diseases did not recognize the 2/D/E peptide. Furthermore, the synthetic peptide performance was compared to the diagnostic performance of the alkaline extract, in which the synthetic peptide showed reduced sensitivity with improved specificity.
Later, Gironès et al. (2001) tested the reactivity of two peptides, isolated from a previous study, and evaluated their potential as CD biomarkers. The peptides, called R3 and S1, were obtained by chemical synthesis and are derived from the dominant autoantigen (Cha) and an acute phase immunogenic antigen, respectively. Reactivity of the peptides was evaluated using a panel of 79 sera from infected individuals and 10 sera healthy individuals. Serum samples from unrelated illnesses were also used. The R3 peptide results revealed sensitivity of 92.4% and specificity of 100%. In relation to S1, the results obtained low recognition of antibody titers for this peptide. The reactivity was similar to other commercial serological tests that used T. cruzi extracts. It was also observed that anti-R3 antibody levels increased as the disease progressed and decreased significantly when individuals were on treatment.
Thomas et al. (2001) analyzed the immunological response of the KMP1 protein, during the CD infectious process. To better understand the regions involved in the recognition of this protein, seven peptides, designated 12,636, 12,637, 12,638, 12,639, 12,640, 12,641, and 12,642, were developed by chemical synthesis and their diagnostic performance was tested using 20 serum samples from infected individuals and 10 negative controls. The results indicated that only peptides 12,638 and 12,642 were able to recognize CD serum samples. However, sensitivity and specificity values were not provided.
In the study developed by Hernández-Marin et al. (2003), an evaluation of the reactivity of three synthetic peptides from T. cruzi. Peptides p17 (R-COOH), p17 (RCONH2) and p18, originated from antigenic regions of the parasite, were tested in ELISA and compared with a natural antigen. Then, peptides were tested using 20 positive serum samples and 20 serum samples from healthy individuals. Results showed that all peptides presented 100% of sensitivity. Furthermore, all peptides have 100% specificity when compared to natural antigens.
Afterwards, Hernández-Marin et al. (2006) tested the reactivity of synthetic peptides that can be used to identify antibodies in Chagas individuals. Two peptides, P1 and P2, each of which contained immunodominant repeat B cell epitopes from T. cruzi, were chemically synthesized. They were evaluated using 82 positive serum samples, including Colombian and Brazilian samples, and 44 Chagas-negative serum samples. The results indicated that P1 recognized 69% of the positive samples from Colombia and 86% of the positive samples from Brazil. Regarding the P2 results, 49% of the positive samples from Colombia and 89% of the positive samples from Brazil recognized P2.
Camussone et al. (2009) performed a rational selection of antigenic peptides with a diagnostic potential for CD. In their work, peptides designated RP1, RP2, and RP5 were tested alone or in combination. To access the peptides’ reactivity, 32 samples from infected individuals and 32 Chagas-negative serum samples were used. The results showed that all peptides were recognized by the positive serum samples. Moreover, peptides mixtures showed a greater discrimination limit as compared to the results when peptides were analyzed alone. However, the peptides’ performance was lower as compared to the diagnostic performance of multiepitope protein which were constructed using these same peptides.
Next, Thomas et al. (2012) tested the reactivity of five peptides exposed in a TcCA-2 antigen of T. cruzi in sera from symptomatic and asymptomatic Chagas-positive individuals. The peptides, designated 3972, 6303, 3973, 3963, and 6173, were synthesized using a simultaneous solid phase multiple peptide method. Their reactivity was analyzed through an ELISA using a panel of 97 positive sera and 30 negative sera. The results showed that peptides 3972, 6303, and 3973 demonstrated 90% sensitivity. Subsequently, they tested the IgG reactivity against only the 3973 peptide, which demonstrated a specificity greater than 98%.
Later, Longhi et al. (2012) evaluated the diagnostic capacity of different peptides, referred to as P013, R13, JL18, JL19, and P0b. Peptide R13 was derived from the C-terminal 13 amino acids of TcP2b, while P013 and P0b were derived from the C-terminal region of the TcP0 protein. Peptide JL18 and JL19 were derived from the T. cruzi recombinant JL9 protein. In their study, 228 positive serum samples and 108 serum from individuals without infection were used. Among the tested peptides, P013 showed high specificity. However, it also presented low sensitivity. Moreover, the peptides’ performance was generally lower as compared to the diagnostic performance of T. cruzi lysate and JL7 protein.
Mendes et al. (2013) performed a genomic screening with the aim of recognizing B cell epitopes and pointing out new serotyping targets. The immunoscreening of 150 high-scoring peptides resulted in the identification of 36 new epitopes and four peptides were chemically synthesized, referred to as C6_30_cons, A6_30_col, Peptide B2_30_y, and Peptide B9_30_cl. Afterward, the peptides were validated using serum samples from 10 Chagas individuals, 56 samples from individuals infected by untyped parasites, and 24 serum samples from healthy individuals. Among the tested peptides, A6_30_col showed the best diagnostic performance, with 100% sensitivity and 91.9% specificity. Peptide C6_30_cons also showed a promising capacity for detecting CD, with 95.8% sensitivity and 88.5% specificity.
Next, Bottino et al. (2013) performed an analysis to map the epitopes of proteins already characterized and known to be highly antigenic, namely the cytoplasmic repetitive antigen (CRA) and flagellar repetitive antigen (FRA). A library was created with serum from Chagas individuals, and based on the observed reactivity, three peptides were identified and synthesized in a solid phase, CRA-1, CRA-2, and FRA-1 epitopes. Thirty-one samples from infected individuals and 12 negative samples were used to evaluate the peptides’ diagnostic performance. Serum samples from leishmaniasis-infected individuals were also used to access cross-reactions. CRA-1 and CRA-2 peptides showed 100% sensitivity and specificity, while FRA-1 presented 91.6 sensitivity and 60% specificity.
Later, Bhattacharyya et al. (2014) made a comparison of the genetic diversity of T. cruzi to form synthetic peptides based on previously described T. cruzi TSSA lineage-specific amino acid sequences. Five peptides, designated TSSApep-I, TSSApep-II/V/VI, TSSApep-III, TSSApep-IV, andTSSApep-V/VI, were chemically synthesized. Serum samples from 186 infected individuals and 31 serum samples from healthy individuals were used. Among the tested peptides, TSSApep-II/V/VI demonstrated greater recognition by serological samples from individuals from different geographic regions.
Balouz et al. (2015) prepared a mapping to identify motifs within a T. cruzi surface antigen. The identified peptide, p36-50, was obtained through chemical synthesis. In order to access its diagnostic performance, 70 serum samples from infected individuals and 38 serum samples from healthy individuals were used. Although sensitivity and specificity values were not provided, the results showed that p36-50 was recognized by the positive samples, with a similar diagnostic performance as compared to a recombinant protein that was also tested in the study.
Next, Mucci et al. (2017) developed a proof-of-principle multiplex diagnostic kit using different validated peptides. More than 2,000 candidate peptides have been identified using a T. cruzi/Chagas HD peptide microarray. After analysis, 28 peptides were chemically synthesized and further tested in an ELISA assay. For this purpose, serum samples from 62 infected individuals were used, along with 16 serum samples from healthy individuals used as a negative control. Initial tests showed sensitivity and specificity values of all peptides, ranging from 3.23 to 91.98% and 93.8 to 100%, respectively. The best-performing peptides, designated pc1, pc2, pc3, p6, p7, p13, and p24, were used to form a new multiepitope recombinant protein, which showed improved sensitivity and specificity values.
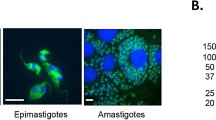
Elisei et al. (2018) used bioinformatics analyses to select three B cell epitopes to be used as antigens for ELISA assays. These peptides, referred to as peptide 1, peptide 2, and peptide 3, were chemically synthesized and tested with 53 sera from Chagas-positive individuals. Additionally, 25 serum samples from healthy individuals were used as a negative control, along with 45 serum samples from individuals with leishmaniasis that were used to access cross-reactions. Among the tested antigens, peptide 2 showed the best diagnostic performance with 100% sensitivity and 97.14% specificity. Peptide 1 showed sensitivity and specificity values of 60.38% and 100%, respectively. Regarding peptide 3 results, a 72.86% of sensitivity was observed, with specitivity value determined as 67.14%. In addition, peptide 2 and peptide 3 were combined to form Mix II, which showed 100% sensitivity and specificity. When compared with laboratory tests IHA, IFA and ELISA, peptide 2 showed a greater diagnostic performance.
Ruiz-Marvéz et al. (2020) performed a B epitope prediction to investigate the possible linear epitopes of the Tc964 protein. After bioinformatics analyses, two peptides, TcNV and TcKP, were obtained using chemical synthesis and their reactivity was tested by ELISA using 63 serum samples from Chagas-positive individuals at different disease stages and six serum samples from negative individuals. Both peptides were able to detect infected individuals in all the stages tested, whether symptomatic or asymptomatic. Moreover, when comparing specificity with two different recombinant proteins, named rTc964 and rLm964, peptides showed a similar specificity value performance in relation to rTc964, where wasn’t observed reactivity with serum samples from active cutaneous leishmaniasis and cured cutaneous leishmaniasis.
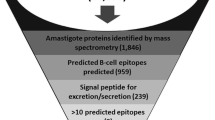
Finally, Majeau et al. (2024) identified protein sequences present in the T. cruzi genome that are useful for diagnosis. Sequences evaluated correspond to 14 genomes from the main parasite’s lineages, and the selected proteins were ordered in peptide microarrays. Subsequently, the peptides were grouped into mixtures containing 6 to 22 peptides, and tested using an ELISA assay, compared with the commercial Chagastest ELISA test. A second ELISA was performed to evaluate the reactivity of the best peptide mixture. Serological panel included samples from different geographic regions, totalizing 64 positive samples and 51 negative samples. Mixtures 12 and 14 demonstrated the best results, with 65% sensitivity and 100% specificity, while Chagatest showed a 45% sensitivity and 100% specificity. In the second assay, peptide mixture 14 had 72.7% sensitivity and 87.5% specificity.
Peptide-base Point-of-care (POCT) assays
Point-of-care (POCT) is a diagnostic strategy developed for rapid and accurate detection of diseases, capable of identifying the presence or absence of a particular antigen. (Goble and Rocafort 2017). Although this diagnostic tool has already been used for more than a decade for other diseases, such as HIV, syphilis, and hepatitis B and C, researchers have shown interest in expanding this technological innovation to include other diseases since the COVID-19 pandemic reinforced the importance of this assay (Brasil 2022; Nichols 2021). Two articles using peptides in this platform for CD diagnosis were found in the literature, in which the authors attempted to revolutionize their research by reconciling the optimization of clinical practice with the rapid delivery of a diagnosis.
A study by Bhattacharyya et al. (2018) was the first to test peptides in a POCT assay. In their work, the peptide TSSApep-II/V/VI, which had been previously tested by Bhattacharyya et al. (2014), was adapted into a new lateral flow immunochromatographic rapid diagnostic test (RDT) called Chagas Sero K-SeT RDT. To access serological reactivity, a panel composed of 336 serum samples from infected individuals and 58 serum samples from healthy individuals was used. Among the positive serum samples derived from paired maternal and cord blood tested, Chagas Sero K-SeT RDT detected 89 (89/131) infected individuals with 100% concordance between maternal and cord blood. Regarding serum samples derived from adult chronic infection, it detected 52.5% (21/40) of individuals without evidence of cardiomyopathy and 74.1% (60/81) of individuals with cardiomyopathy. Moreover, Chagas Sero K-SeT RDT showed reactivity with only 7 (7/65) serum samples among the Peruvian samples. Finally, this test showed a specificity \of 96.5%.
Continuing the above-cited studies with POCT, Murphy et al. (2019) evaluated the Chagas Sero K-SeT RDT using serum samples from the Chaco region of northern Argentina. A total of 393 positive samples were tested, in which the seroprevalence of Chagas Sero K‑SeT RDT was 69.5%. Moreover, Chagas Sero K-SeT RDT performed better when compared to TSSApep-based ELISA, given that Chagas Sero K-SeT RDT detected 61% of the positive cases, while only 34% of the cases were detected using TSSApep-based ELISA. Table 1 summarizes the main points of the above-cited studies.
Discussion
Although a number of CD diagnostic tools have been developed, most endemic regions are still affected by the underdiagnosis of T. cruzi infection (Suárez et al. 2022). In fact, endemic and non-endemic countries find it difficult to incorporate new technologies and have to rely on inefficient strategies, mainly due to monetary restrictions (Abras et al. 2022). Considering the different specifications approved in the current preparation of diagnostic kits, peptide-based antigens represent a viable alternative (Bhattacharyya et al. 2018; Murphy et al. 2019). The use of peptides for diagnostics offers some advantages over the use of recombinant proteins, given that recombinant proteins may trigger more false-positive results due to the larger size, in addition of having the possibility of misfolding and poor conformation of the protein, which can impact negatively in diagnostics tests (Pandey et al. 2021). Moreover, a standardized diagnosis could be more easily achieved using peptides considering batch variation is more unusual when working with peptides as compared to recombinant proteins. Furthermore, recombinant proteins usually require a living organism as an expression system, contrasting with methods of obtaining peptides that normally do not require living organisms for their production (Francis and Page 2010). As such, the identification and validation of short peptides as possible antigenic targets in the serological diagnosis of CD has attracted the attention of many scientists.
Researchers have made efforts to screen promising new peptides for CD diagnosis. The data presented in the studies described above indicate that many peptides tested were promising for the CD diagnosis, as they indicated sensitivity and specificity greater than 90%. It is known that antigens from totally inactive parasites can cross-react with antigens from other protozoans, such as Leishmania spp., which is one of the main causes of cross-reaction in serological tests (Schijman et al. 2022). Studies, such as those developed by Aznar et al. (1995), Betonico et al. (1999), Hernández-Marin et al. (2003) and Elisei et al. (2018), demonstrated that the use of peptides can reduce the occurrence of cross-reactivity, maintaining the percentage of reliable positive and negative results. Although many results were favorable, it cannot yet be inferred which of these peptides has the best diagnostic performance, due to several reasons, such as the different sample panels used, different concentrations of peptides and different diagnostic protocols.
Among the studies described above, the majority used a serological panel composed of serum from individuals in the chronic phase, detecting the presence of IgG class antibodies. In fact, only four studies included serum samples from individuals in both the acute and chronic phase, detecting the presence of IgM and IgG, respectively.
Therefore, more studies are still needed to investigate the diagnostic performance of the different peptides, using characterized serum samples from both the acute and chronic phase. Based on the dynamics of parasitemia and sera antibodies (Fig. 1), the reality of serological tests for Chagas currently shows that, in addition to the need to perform more than one test to diagnose chronic infection, there is still a major bottleneck in diagnosing the disease in the acute phase. The lack of an accurate serological diagnosis in the acute phase of CD highlights a major problem, since the identification of T. cruzi through direct and indirect parasitological methods is more laborious, in addition to the social vulnerability of some individuals making it impossible to diagnose. In this sense, it is clear that it is still necessary the development of a single biomarker capable of diagnose the infected individual in both phases of the disease.
Dynamics of parasitemia and sera antibodies, which are the basis for detecting the parasite or its DNA, as well as antibodies, during acute and chronic Trypanosoma cruzi infection. During acute infection, parasitemia is high, allowing for direct examination- and PCR-based diagnosis. Antibody-based methods detecting mostly IgM are also used. Acute phase is the best window for diagnosis for increased treatment efficacy. At the chronic stage, low grade parasitemia does not allow for direct examination, and PCR-based methods are variable in sensitivity. Antibody-based specific IgG serology is widely used. All testes are laboratory-based, with no point-of-care tests currently available. No tests for disease prognosis are currently available
It should be noted that many reasons can interfere with the sensitivities of the tests, mainly in relation to the selection of antigens with better immunoreactivity, and the ability to generate less interference in the tests (Ferreira et al. 1991), where the similarity of epitopes that exist between diferente species, such as Leishmania spp and T. cruzi (Granjon et al. 2016; Ferreira et al. 2001), can negatively impact in diagnostic accuracy. In this sense, the search for epitopes capable of presenting high sensitivity and specificity is extremely importante. In that regard, it is possible to observe that most of the above-mentioned peptides come only from commonly used proteins, such as MAP, SAPA, CRA, FRA, TSSA, B13 and TcD, of which many of them composes commercial kits for the disease, such as Chagas ELISA IgG + IgM® (Vircell®, Granada, Spain) and IgG-ELISA® (NovaTec Immunodiagnostica GmbH; Dietzenbach, Germany). In this sense, since many peptides are derived from proteins already widely used, their excellent diagnostic performance was already expected. However, further studies using the same serological panel are needed to evaluate the performance of the peptides and their source proteins. Moreover, it is known that the amino acid sequence of MAP and FRA, for example, presents 40% and 70% similarity with L. infantum, as well as 52% and 63% similarity with L. braziliensis, respectively (Hernández et al. 2010). This similarity between species can be a possible explanation for some unsatisfactory results presented using some peptides, such as FRA-1 and 6173 peptides. especially regarding specificity values.
It is evident that most peptides have different amino acid sequences, except TcD, P1, P2, pc3, RP5 and 3973, which share the same sequences or present some small variation. This reflects the effectiveness of these peptides, since these sequences resulted in high sensitivity and specificity values, even with different serological panels employed in serological tests, confirming their potential as an antigenic marker. Furthermore, peptides that show good results motivated the development of commercial tests, such as BioElisa Chagas (Biokit, Barcelona, Spain), which uses recombinant antigen composed of TcD, TcE, PEP2 and TCLi1-2, achieving 98% sensitivity and 100% specificity (Duarte et al. 2014; Houghton et al. 1999), and Chagas Sero K-SeT, which employed the peptide TSSApep-II/V/VI (Murphy et al. 2021).
When developing diagnostic tests, the genetic variability of T. cruzi must be taken into account, a factor that interferes with the accuracy of the results, highlighting the importance of studies that evaluate the antigenic structures of this parasite (Mendes et al. 2013). The broad parasite genetic lineage in different geographic areas can directly interfere with the diagnostic performance, which may negatively impact the sensitivity of the tests. Despite that, most serological tests developed to date does not focus on the use of markers that are genetically conserved among the most diverse strains. In fact, biomarkers originating from highly conserved proteins can provide excellent results, being promising candidates for the development of a universal diagnosis (Majeau et al. 2024). Indeed, the investigation of conserved peptide portions is essential for the incorporation of antigens able to be recognized by antibodies produced against different parasite strains (Rodríguez-Bejarano et al. 2021; Reis-Cunha et al. 2014; Mendes et al. 2013). The genetic variability of each tested population must also be taken into account since lifestyle, nutritional and immunological status, and previous disease history, are important factors for the progression of the disease in the infected individual, which can impact directly in the diagnosis (Magalhães et al. 2022). In fact, the study developed by Bhattacharyya et al. (2018) showed that positive serum samples from different geographical areas recognized differently the peptides under study, impacting the diagnostic performance of each. This reinforces the need to expand the study population in future studies.
In addition, a more accurate prediction and selection of epitopes to be incorporate in diagnostic kits is of great relevance, as it can enable the manufacture of more specific reagents, capable of discriminating the clinical phase of the disease (Balouz et al. 2017). The characterization of immunodominant epitopes contributes to the epidemiological search for each genetic lineage of the parasite, favoring the development of control and prevention strategies, as well as the production of more sensitive diagnoses (Suárez et al. 2022). In fact, studies that provide a more in-depth characterization of epitopes, as well as broad testing in different populations, are essential for better guidance in the development of new biomarkers for diagnosis (Ricci et al. 2023).
Diagnostic techniques can exhibit inaccessible conditions, especially in remote areas where laboratories are precarious, with few resources, and the lack of trained professionals. Therefore, rapid diagnostic test development would overcome this hindrance, considering this assay does not require equipment to be set up to carry it out, thus reducing operating costs and providing faster results. Health agents could diagnose individuals in remote locations, enabling a better prognosis of the infection. There are still many limitations in obtaining an accurate CD serological diagnosis, suggesting some measures could be implemented, such as manufacturing low-cost reagents, obtaining new biomarkers, and developing rapid tests. Furthermore, improved ELISA techniques would allow more accurate diagnoses to be made, reducing the number of tests and giving more people access to an early and accurate diagnosis. Having better access to an accurate CD diagnosis could help control the disease.
This review brings together information on the use of peptides in serological diagnosis in infected individuals. Most studies were efficient and demonstrated promising peptides capable of providing an optimized, high-throughput differential diagnosis. Therefore, the use of peptides in serological tests has been increasingly used to improve T. cruzi identification and disease monitoring.
Data availability
Not applicable.
References
Abras A, Ballart C, Fernández-Arévalo A, Pinazo MJ, Gascón J, Muñoz C, Gállego M (2022) Worldwide Control and management of chagas disease in a new era of globalization: a close look at congenital trypanosoma cruzi infection. Clin Microbiol Rev 35(2):E00152-E221. https://doi.org/10.1128/2fcmr.00152-21
Akbarian M, Khani A, Eghbalpour S, Uversky VN (2022) Bioactive peptides: synthesis, sources, applications, and proposed mechanisms of action. Int J Mol Sci 23(3):1445. https://doi.org/10.3390/Ijms23031445
Al-Azzam S, Ding Y, Liu J, Pandya P, Ting JP, Afshar S (2020) Peptides to combat viral infectious diseases. Peptides 134:170402. https://doi.org/10.1016/2fj.Peptides.2020.170402
Apostolopoulos V, Bojarska J, Chai TT, Elnagdy S, Kaczmarek K, Matsoukas J, New R, Parang K, Lopez OP, Parhiz H, Perera CO, Pickholz M, Remko M, Saviano M, Skwarczynski M, Tang Y, Wolf WM, Yoshiya T, Zabrocki J, Zielenkiewicz P, Alkhazindar M, Barriga V, Kelaidonis K, Sarasia EM, Toth I (2021) A global review on short peptides: frontiers and perspectives. Molecules 26(2):430. https://doi.org/10.3390/2fmolecules26020430
Avaria A, Ventura-Garcia L, Sanmartino M, Van der LC (2022). Population movements, borders, and Chagas disease. Memórias do Instituto Oswaldo Cruz 117:e210151. https://doi.org/10.1590/2F0074-02760210151
Aydin S (2015) A short history, principles, and types of elisa, and our laboratory experience with peptide/protein analyses using elisa. peptides, festschrift to highlight the career of Abba. J Kastin A Founding Editor, Research Educ Peptide Field 72:4–15. https://doi.org/10.1016/J.Peptides.2015.04.012
Aznar C, Lopez-Bergami P, Brandariz S, Mariette C, Liegeard P, Alves Md, Barreiro EL, Carrasco R, Lafon S, Kaplan D (1995) Prevalence of anti-R-13 antibodies in human trypanosoma cruzi infection. Fems Immunol Med Microbiol 12(3–4):231–238. https://doi.org/10.1016/J.Peptides.2015.04.012
Balouz V, Agüero F, Buscaglia CA (2017) Chagas disease diagnostic applications: present knowledge and future steps. Adv Parasitol 97:1–45. https://doi.org/10.1016/2fbs.Apar.2016.10.001
Balouz V, Cámara M de LM, Cánepa GE, Carmona SJ, Volcovich R, Gonzalez N, Altcheh J, Agüero F, Buscaglia CA (2015) Mapping antigenic motifs in the trypomastigote small surface antigen from trypanosoma cruzi. Clin Vaccine Immunol 22(3):304–312. https://doi.org/10.1128/cvi.00684-14
Bern C, Messenger LA, Whitman JD, Maguire JH (2019) Chagas disease In The United States: a public health approach. Clin Microbiol Rev 33(1):E00023-19, 27. https://doi.org/10.1128/2fcmr.00023-19
Betônico GN, Miranda EO, Silva DA, Houghton R, Reed SG, Campos-Neto A, Mineo JR (1999) Evaluation of a synthetic tripeptide as antigen for detection of Igm and Igg antibodies to trypanosoma cruzi in serum samples from patients with chagas disease or viral diseases. Trans R Soc Trop Med Hyg 93(6):603–606. https://doi.org/10.1016/S0035-9203(99)90064-0
Bhattacharyya T, Messenger LA, Bern C, Mertens P, Gilleman Q, Zeippen N, Bremer Hinckel BC, Murphy N, Gilman RH, Miles MA, Chagas Working Group In Bolivia And Peru (2018) Severity of chagasic cardiomyopathy is associated with response to a novel rapid diagnostic test for trypanosoma cruzi Tcii/V/Vi. Clin Infect Dis Off Publ Infect Dis Soc Am 67(4):519–524. https://doi.org/10.1093/Cid/Ciy121
Bhattacharyya T, Falconar AK, Luquetti AO, Costales JA, Grijalva MJ, Lewis MD, Messenger LA, Tran TT, Ramirez JD, Guhl F, Carrasco HJ, Diosque P, Garcia L, Litvinov SV, Miles MA (2014) Development of peptide-based lineage-specific serology for chronic chagas disease: geographical and clinical distribution of epitope recognition. PLoS Negl Trop Dis 8(5):E2892. https://doi.org/10.1371/2fjournal.Pntd.0002892
Bottino CG, Gomes LP, Pereira JB, Coura JR, Provance DW, De-Simone SG (2013) Chagas disease-specific antigens: characterization of epitopes in Cra/Fra by synthetic peptide mapping and evaluation by elisa-peptide assay. BMC Infect Dis 13:568. https://doi.org/10.1186/1471-2334-13-568
Brasil (2022) Ministério da Saúde Chagas disease. https://www.Gov.Br/Saude/Pt-Br/Assuntos/Saude-De-A-A-Z/D/Doenca-De-Chagas/Doenca-De-Chagas. Accessed 21 Sep 2023
Brown L, Westby M, Souberbielle BE, Szawlowski PW, Kemp G, Hay P, Dalgleish AG (1997) Optimisation of a peptide-based indirect elisa for the detection of antibody in the serum of HIV-1 seropositive patients. J Immunol Methods 200(1–2):79–88. https://doi.org/10.1016/S0022-1759(96)00192-5
Burns JM, Shreffler WG, Rosman DE, Sleath PR, March CJ, Reed SG (1992) identification and synthesis of a major conserved antigenic epitope of trypanosoma Cruzi. Proc Natl Acad Sci USA 89(4):1239–1243. https://doi.org/10.1073/Pnas.89.4.1239
Camussone C, Gonzalez V, Belluzo MS, Pujato N, Ribone ME, Lagier CM, Marcipar IS (2009) Comparison of recombinant trypanosoma cruzi peptide mixtures versus multiepitope chimeric proteins as sensitizing antigens for immunodiagnosis. Clin Vaccine Immunol CVI 16(6):899–905. https://doi.org/10.1128/Cvi.00005-09
Castiglione V, Aimo A, Vergaro G, Saccaro L, Passino C, Emdin M (2022) Biomarkers for the diagnosis and management of heart failure. Heart Fail Rev 27(2):625–643. https://doi.org/10.1007/S10741-021-10105-W
Chagas C (1909) Nova Tripanozomiaze Humana: Estudos Sobre A Morfolojia E O Ciclo Evolutivo Do Schizotrypanum Cruzi N. Gen., N. Sp., Ajente Etiolojico De Nova Entidade Morbida Do Homem. Mem Inst Oswaldo Cruz 1:159–218. https://doi.org/10.1590/S0074-02761909000200008
Cortés-Sarabia K, Luna-Pineda VM, Rodríguez-Ruiz HA, Leyva-Vázquez MA, Hernández-Sotelo D, Beltrán-Anaya FO, Vences-Velázquez A, Del Moral-Hernández O, Illades-Aguiar B (2022) Utility of in silico-identified-peptides in spike-s1 domain and nucleocapsid of Sars-Cov-2 for antibody detection in covid-19 patients and antibody production. Sci Rep 12:15057. https://doi.org/10.1038/2fs41598-022-18517-W
Coura JR (2013) The discovery of chagas disease (1908–1909): great successes and certain misunderstandings and challenges. Rev Soc Bras Med Trop 46:389–390. https://doi.org/10.1590/0037-8682-0143-2013
De Salazar PM, Sosa-Estani S, Salvador F, Sulleiro E, Sánchez-Montalvá A, Ribeiro I, Molina I, Co B (2022) Human trypanosoma cruzi chronic infection leads to individual level steady-state parasitemia: implications for drug-trial optimization in chagas disease. PLoS Negl Trop Dis 16(11):E0010828. https://doi.org/10.1371/2fjournal.Pntd.0010828
Duarte LF, Flórez O, Rincón G, González CI (2014) Comparison of seven diagnostic tests to detect Trypanosoma cruzi infection in patients in chronic phase of Chagas disease. Colomb Med 2014(45):61–66
Elisei RMT, Matos CS, Carvalho AMRS, Chaves AT, Medeiros FAC, Barbosa R, Marcelino AP, Dos Santos EK, Coelho EAF, Duarte MC, De Oliveira Mendes TA, Da Costa Rocha MO, Menezes-Souza D (2018) Immunogenomic screening approach to identify new antigens for the serological diagnosis of chronic chagas’ disease. Appl Microbiol Biotechnol 102(14):6069–6080. https://doi.org/10.1007/S00253-018-8992-7
Engvall E (2010) The Elisa, Enzyme-linked immunosorbent assay. Clin Chem 56(2):319–320. https://doi.org/10.1373/Clinchem.2009.127803
Engvall E, Perlmann P (1971) Enzyme-linked immunosorbent assay (Elisa). Quant Assay Immunoglob g Immunochem 8(9):871–874. https://doi.org/10.1016/0019-2791(71)90454-X
Falconi-Agapito F, Kerkhof K, Merino X, Bakokimi D, Torres F, Van Esbroeck M, Talledo M, Ariën KK (2022) Peptide biomarkers for the diagnosis of dengue infection. Front Immunol 13:793882. https://doi.org/10.3389/2ffimmu.2022.793882
Feliciano ND, Da, Santos F De AA, Fujimura PT, Gonzaga HT, Goulart LR, Costa-Cruz JM RV (2014) Bacteriophage-fused peptides for serodiagnosis of human strongyloidiasis. PLoS Negl Trop Dis 8(5):E2792. https://doi.org/10.1371/2fjournal.Pntd.0002792
Ferreira AW, Belem ZR, Moura MEG, Camargo ME (1991) Aspectos da padronização de testes sorológicos para a doença de Chagas: um teste imunoenzimático para a triagem de doadores de sangue. Rev Inst Med Trop Sao Paulo 33(2):123–128. https://doi.org/10.1590/S0036-46651991000200006
Ferreira AW, Belem ZR, Lemos EA, Reed SG, Campos-Neto A (2001) Enzyme-linked immunosorbent assay for serological diagnosis of Chagas’ disease employing a Trypanosoma cruzi recombinant antigen that consists of four different peptides. J Clin Microbiol 39(12):4390–4395. https://doi.org/10.1128/2FJCM.39.12.4390-4395.2001
Ferreira RR, Waghabi MC, Bailly S, Feige JJ, Hasslocher-Moreno AM, Saraiva RM, Araujo-Jorge TC (2022) The search for biomarkers and treatments in chagas disease: insights from Tgf-beta studies and immunogenetics. Front Cell Infect Microbiol 11:767576. https://doi.org/10.3389/2ffcimb.2021.767576
Fisher E, Pavlenko K, Vlasov A, Ramenskaya G (2019) Peptide-based therapeutics for oncology. Pharm Med 33(1):9–20. https://doi.org/10.1007/S40290-018-0261-7
Forsyth CJ, Manne-Goehler J, Bern C, Whitman J, Hochberg NS, Edwards M, Marcus R, Beatty NL, Castro-Sesquen YE, Coyle C, Stigler Granados P, Hamer D, Maguire JH, Gilman RH, Meymandi S (2021) Recommendations for screening and diagnosis of chagas disease in the United States. J Infect Dis 225(9):1601–1610. https://doi.org/10.1093/2finfdis/2fjiab513
Fourneau E, Fischer E (1901) Über einige derivate des glykocolls. Ber 34:2868–2877. https://doi.org/10.1002/Cber.190103402249
Francis DM, Page R (2010) Strategies to optimize protein expression in E. Coli. Curr Protoc Prot Sci 61(1):5241–52429. https://doi.org/10.1002/2f0471140864.Ps0524s61
GME (2023) Artificial Intelligence Market Size And Share Report. Available at: https://www.grandviewresearch.com/industry-analysis/artificial-intelligence-ai-market. Accessed 30 Sep 2023
Gironès N, Rodríguez CI, Basso B, Bellon JM, Resino S, Muñoz-Fernández MA, Gea S, Moretti E, Fresno M (2001) Antibodies to an epitope from the cha human autoantigen are markers of chagas’ disease. Clin Diagn Lab Immunol 8(6):1039–1043. https://doi.org/10.1128/Cdli.8.6.1039-1043.2001
Goble JA, Rocafort PT (2017) Point-of-care testing. J Pharm Pract 30(2):229–237. https://doi.org/10.1177/0897190015587696
Gómez-Ochoa AS, Rojas LZ, Echeverría LE, Muka T, Franco OH (2022) Global, regional, and national trends of chagas disease from 1990 to 2019: comprehensive analysis of the global burden of disease study. Glob Heart 17(1):59. https://doi.org/10.5334/2Fgh.1150
Gonzalez L, Boyle RW, Zhang M, Castillo J, Whittier S, Della-Latta P, Clarke LM, George JR, Fang X, Wang JG, Hosein B, Wang CY (1997). Synthetic-peptide-based enzyme-linked immunosorbent assay for screening human serum or plasma for antibodies to human immunodeficiency virus type 1 and type 2. Clin Diagn Lab Immunol 4(5):598–603. https://doi.org/10.1128/cdli.4.5.598-603.1997
Granjon E, Dichtel-Danjoy ML, Saba E, Sabino E, Campos De Oliveira L, Zrein M (2016) Development of a novel multiplex immunoassay multi-cruzi for the serological confirmation of chagas disease. PLoS Negl Trop Dis 10(4):e0004596. https://doi.org/10.1371/2Fjournal.pntd.0004596
Hansen S (2015) Die Entdeckung Der Proteinogenen Aminosauren De 1805 Em Paris A 1935 Em Illinois. https://web.Archive.Org/Web/20171201232937, https://www.Arginium.De/Wp-Content/Uploads/2015/12/Entdeckung-Der-Aminos%C3%A4uren.Pdf
Hernández P, Heimann M, Riera C, Solano M, Santalla J, Luquetti AO, Beck E (2010) Highly effective serodiagnosis for Chagas’ disease. Clin Vaccine Immunol 17(10):1598–1604. https://doi.org/10.1128/cvi.00489-08
Hernández-Marin M, Hernández SI, Ramos MG, Pozo PL (2006) Chimeric synthetic peptides as antigens for detection of antibodies to Trypanosoma cruzi. Biochem Biophys Res Commun 339(1):89–92. https://doi.org/10.1016/j.bbrc.2005.11.001
Hernández-Marin M, Almenares-Guash P, Martínez-Ortiz C, Gómez-Cordero I, Melchor-Rodríguez A (2003) Immunologysynthetic peptides of trypanosoma cruzi for the immunodiagnostic of chagas' disease. Bioquimia 28(1):2–7
Houghton RL, Benson DR, Reynolds LD, Mcneill PD, Sleath PR, Lodes MJ, Skeiky YA, Leiby DA, Badaro R, Reed SG (1999) A multi-epitope synthetic peptide and recombinant protein for the detection of antibodies to trypanosoma cruzi in radioimmunoprecipitation-confirmed and consensus-positive sera. J Infect Dis 179(5):1226–1234. https://doi.org/10.1086/314723
Jackwood MW, Hilt DA (1995) Production and immunogenicity of multiple antigenic peptide (Map) constructs derived from the S1 glycoprotein of infectious bronchitis virus (Ibv). Adv Exp Med Biol 380:213–219. https://doi.org/10.1007/978-1-4615-1899-0_35
Joshi VG, Dighe VD, Thakuria D, Malik YS, Kumar S (2013) Multiple antigenic peptide (map): a synthetic peptide dendrimer for diagnostic, antiviral and vaccine strategies for emerging and re-emerging viral diseases. Indian J Virol 24(3):312–320. https://doi.org/10.1007/2fs13337-013-0162-Z
Lechner J, Hartkopf F, Hiort P, Nitsche A, Grossegesse M, Doellinger J, Renard BY, Muth T (2019) Purple: a computational workflow for strategic selection of peptides for viral diagnostics using ms-based targeted proteomics. Viruses 11(6):536. https://doi.org/10.3390/2fv11060536
Ledezma AP, Blandon R, Schijman AG, Benatar A, Saldaña A, Osuna A (2020) Mixed infections by different trypanosoma cruzi discrete typing units among chagas disease patients in an endemic community in panama. Plos One 15(11):E0241921. https://doi.org/10.1371/2fjournal.Pone.0241921
Lee BY, Bacon KM, Bottazzi ME, Hotez PJ (2013) Global economic burden of chagas disease: a computational simulation model. Lancet Infect Dis 13(4):342–348. https://doi.org/10.1016/2fs1473-3099(13)70002-1
Li R, Ma Y, Li J, Zhou P, Zheng F, Liu Q, Gao W (2020) Application of toxoplasma gondii Gra15 peptides in diagnosis and serotyping. Microbial Pathogen 143:104168. https://doi.org/10.1016/J.Micpath.2020.104168
Lidani KCF, Andrade FA, Bavia L, Damasceno FS, Beltrame MH, Messias-Reason IJ, Sandri TL (2019) Chagas disease: from discovery to a worldwide health problem. Front Public Health 7:166. https://doi.org/10.3389/fpubh.2019.00166
Link JS, Alban SM, Soccol CR, Pereira GVM, Thomaz Soccol V (2017) Synthetic peptides as potential antigens for cutaneous leishmaniosis diagnosis. J Immunol Res 2017:5871043. https://doi.org/10.1155/2f2017/2f5871043
Liu YF, Powrie J, Arif S, Yang JHM, Williams E, Khatri L, Joshi M, Lhuillier L, Fountoulakis N, Smith E, Beam C, Lorenc A, Peakman M, Tree T (2022) Immune and metabolic effects of antigen-specific immunotherapy using multiple Β-cell peptides in type 1 diabetes. Diabetes 71(4):722–732. https://doi.org/10.2337/Db21-0728
Longhi SA, Brandariz SB, Lafon SO, Niborski LL, Luquetti AO, Schijman AG, Levin MJ, Gómez KA (2012) Evaluation of in-house elisa using trypanosoma cruzi lysate and recombinant antigens for diagnosis of chagas disease and discrimination of its clinical forms. Am J Trop Med Hyg 87(2):267–271. https://doi.org/10.4269/Ajtmh.2012.11-0533
Lorenzo MA, Pachón D, Maier A, Bermúdez H, Losada S, Toledo M, Pujol FH, Alarcón De Noya B, Noya O, Serrano ML (2021) Immunoinformatics and pepscan strategies on the path of a peptide-based serological diagnosis of covid19. J Immunol Methods 495:113071. https://doi.org/10.1016/2fj.Jim.2021.113071
Magalhães LMD, Gollob KJ, Zingales B, Dutra WO (2022) Pathogen diversity, immunity, and the fate of infections: lessons learned from trypanosoma cruzi human-host interactions. Lancet Microbe 3(9):E711–E722. https://doi.org/10.1016/S2666-5247(21)00265-2
Majeau A, Dumonteil E, Herrera C (2024) Identification of highly conserved Trypanosoma cruzi antigens for the development of a universal serological diagnostic assay. Emerg Microb Infect 13(1):2315964. https://doi.org/10.1080/22221751.2024.2315964
Marin-Neto JA, Rassi A, Oliveira GMM, Correia LCL, Ramos AN, Luquetti AO, Hasslocher-Moreno A M, De Sousa AS, De Paola AAV, Sousa ACS, Ribeiro ALP, Correia D, De Souza D Do SM, Cunha-Neto E, Ramires FJA, Bacal F, Nunes M Do CP, Martinelli M, Scanavacca MI, Saraiva RM, De Oliveira WA, Lorga-Filho AM, Guimarães A De JB De A, Braga ALL, De Oliveira AS, Sarabanda AVL, Pinto AY Das N, Do Carmo AAL, Schmidt A, Da Costa AR., Ianni BM, Markman B, Rochitte CE, Macêdo CT, Mady C, Chevillard C, Virgens CMB Das, De Castro CN, Britto CFDP De C, Pisani C, Rassi D Do C, Sobral DC, De Almeida DR, Bocchi EA, Mesquita ET, Mendes F De SNS, Gondim FTP, Da Silva GMS, Peixoto G De L, De Lima GG, Veloso HH, Moreira HT, Lopes HB, Pinto IMF, Ferreira JMBB, Nunes JPS, Barreto-Filho JAS, Saraiva JFK, Lannes-Vieira J, Oliveira JLM, Armaganijan LV, Martins LC, Sangenis LHC, Barbosa MPT, Almeida-Santos MA, Simões MV, Yasuda MAS, Moreira M Da CV, Higuchi M De L, Monteiro MR De CC, Mediano MFF, Lima MM, De Oliveira MT, Romano MMD, De Araujo NNSL, Medeiros P De TJ, Alves RV, Teixeira RA, Pedrosa RC, Aras R, Torres RM, Povoa RM Dos S, Rassi S G, Alves SMM, Tavares SB Do N, Palmeira SL, Da Silva TL, Rodrigues T Da R, Madrini V, Brant VM Da C, Dutra WO, Dias JCP (2023) Diretriz Da Sbc Sobre Diagnóstico E Tratamento De Pacientes Com Cardiomiopatia Da Doença De Chagas—2023. Arquivos Brasileiros De Cardiologia 120(6):E20230269. https://doi.org/10.36660/2fabc.20230269
Medeiros C De A, Silva MB De A, De Oliveira ALS, Alves SMM, Barros M Das ND Da S, Cavalcanti M Da GA De M, Oliveira GM De A, Carrazzone C De FV, De Oliveira WA, De Medeiros ZM (2022) Mapping The Morbidity And Mortality Of Chagas Disease In An Endemic Area In Brazil. Revista Do Instituto De Medicina Tropical De São Paulo 64:E5, [S.D.] https://doi.org/10.1590/S1678-9946202264005
Medone P, Ceccarelli S, Parham PE, Figuera A, Rabinovich JE (2015). The impact of climate change on the geographical distribution of two vectors of Chagas disease: implications for the force of infection. Philos Trans R Soc Lond B Biol Sci 370(1665):20130560. https://doi.org/10.1098/2Frstb.2013.0560
Mendes TA, De O, Reis Cunha JL, De Almeida LR, Gf RL, Lemos LD, Dos Santos ARR, Da Câmara ACJ, Da GLM, C, Bern C, Gilman RH, Fujiwara RT, Gazzinelli RT, Bartholomeu DC (2013) Identification of strain-specific b-cell epitopes in trypanosoma cruzi using genome-scale epitope prediction and high-throughput immunoscreening with peptide arrays. PLoS Negl Trop Dis 7(10):E2524. https://doi.org/10.1371/Journal.Pntd.0002524
Mucci J, Carmona SJ, Volcovich R, Altcheh J, Bracamonte E, Marco JD, Nielsen M, Buscaglia CA, Agüero F (2017) Next-generation elisa diagnostic assay for chagas disease based on the combination of short peptidic epitopes. PLoS Negl Trop Dis 11(10):E0005972. https://doi.org/10.1371/2fjournal.Pntd.0005972
Murphy N, Macchiaverna NP, Victoria Cardinal M, Bhattacharyya T, Mertens P, Zeippen N, Gustin Y, Gilleman Q, Gürtler RE, Miles MA (2019) Lineage-specific rapid diagnostic tests can resolve trypanosoma cruzi Tcii/V/Vi ecological and epidemiological associations in the argentine chaco. Parasit Vectors 12(1):424. https://doi.org/10.1186/S13071-019-3681-7
Murphy N, Cardinal MV, Bhattacharyya T, Enriquez GF, Macchiaverna NP, Alvedro A, Freilij H, Martinez de Salazar P, Molina I, Mertens P, Gilleman Q, Gürtler RE, Miles MA (2021) Assessing antibody decline after chemotherapy of early chronic Chagas disease patients. Parasit Vectors 14(1):543. https://doi.org/10.1186/2Fs13071-021-05040-6
Nichols JH (2021) Utilizing point-of-care testing to optimize patient care. Ejifcc 32(2):140–144
Nunes MCP, Beaton A, Acquatella H, Bern C, Bolger AF, Echeverría LE, Dutra WO, Gascon J, Morillo CA, Oliveira-Filho J, Ribeiro ALP, Marin-Neto JA, Fever AHAR, Young EAKDCOTCOCDIT, Nursing COCAS, Council S (2018) Chagas cardiomyopathy: an update of current clinical knowledge and management: a scientific statement from the American Heart Association. Circulation 138(12):E169–E209. https://doi.org/10.1161/Cir.0000000000000599
Paho/Who (2019) Guidelines for the Diagnosis and Treatment of Chagas Diseases. https://iris.paho.org/bitstream/handle/10665.2/49653/9789275120439_eng.pdf
Paho/Who (2023) Less Than 10% Of Those Infected With Chagas Disease Receive Timely Diagnosis And Treatment. https://www.paho.org/en/news/13-4-2023-less-10-people-chagas-receive-diagnosis
Pandey S, Malviya G, Chottova Dvorakova M (2021) Role of peptides in diagnostics. Int J Mol Sci 22(16):8828. https://doi.org/10.3390/2fijms22168828
Peralta JM, Teixeira MG, Shreffler WG, Pereira JB, Burns JM, Sleath PR, Reed SG (1994) Serodiagnosis of chagas’ disease by enzyme-linked immunosorbent assay using two synthetic peptides as antigens. J Clin Microbiol 32(4):971–974. https://doi.org/10.1128/Jcm.32.4.971-974.1994
Piggott AM, Karuso P (2016) Identifying the cellular targets of natural products using T7 phage display. Nat Prod Rep 33(5):626–636. https://doi.org/10.1039/C5np00128e
Rangel R, Guzman-Rojas L, Le Roux LG, Staquicini FI, Hosoya H, Barbu EM, Ozawa MG, Nie J, Jr KD, Langley RR, Sage EH, Koivunen E, Gelovani JG, Lobb RR, Sidman RL, Pasqualini R, Arap W (2012) Combinatorial targeting and discovery of ligand-receptors in organelles of mammalian cells. Nat Commun 3:788. https://doi.org/10.1038/2fncomms1773
Rassi A, Rassi A, Ja M-N (2010) Chagas disease. Lancet (London, England) 375(9723):1388–1402. https://doi.org/10.1016/S0140-6736(10)60061-X
Reis-Cunha JL, Mendes TADO, De Almeida Lourdes R, Ribeiro DRDS, Machado-De-Avila RA, De Oliveira Tavares M, Lemos DS, Câmara ACJ, Olórtegui CC, De Lana M, Da Cunha Galvão LM, Fujiwara RT, Bartholomeu DC (2014) Genome-Wide Screening And Identification Of New Trypanosoma Cruzi Antigens With Potential Application For Chronic Chagas Disease Diagnosis. Plos One 9(9):E106304. https://doi.org/10.1371/journal.pone.0106304
Ricci AD, Bracco L, Salas-Sarduy E, Ramsey JM, Nolan MS, Lynn MK, Altcheh J, Ballering GE, Torrico F, Kesper N, Villar JC, Marcipar IS, Marco JD, Agüero F (2023). The Trypanosoma cruzi Antigen and Epitope Atlas: antibody specificities in Chagas disease patients across the Americas. Nat Commun 14(1):1850. https://doi.org/10.1038/s41467-023-37522-9
Rodríguez-Bejarano OH, Avendaño C, Patarroyo MA (2021) Mechanisms associated with trypanosoma cruzi host target cell adhesion. Recogn Int Life 11(6):534. https://doi.org/10.3390/Life11060534
Ruiz-Márvez E, Ramírez CA, Rodríguez ER, Flórez MM, Delgado G, Guzmán F, Gómez-Puertas P, Requena JM, Puerta CJ (2020) Molecular characterization of Tc964, a novel antigenic protein from trypanosoma cruzi. Int J Mol Sci 21(7):2432. https://doi.org/10.3390/Ijms21072432
Safiabadi Tali SH, Leblanc JJ, Sadiq Z, Oyewunmi OD, Camargo C, Nikpour B, Armanfard N, Sagan SM, Jahanshahi-Anbuhi S (2021) Tools and techniques for severe acute respiratory syndrome coronavirus 2 (Sars-Cov-2)/covid-19 detection. Clin Microbiol Rev 34(3):E00228-E320. https://doi.org/10.1128/2fcmr.00228-20
Santos EF, Silva ÂAO, Leony LM, Freitas NEM, Daltro RT, Regis-Silva CG, Del-Rei RP, Souza WV, Ostermayer AL, Costa VM, Silva RA, Ramos AN, Sousa AS, Gomes YM, Santos FLN (2020) Acute chagas disease in brazil from 2001 to 2018: a nationwide spatiotemporal analysis. PLoS Negl Trop Dis 14(8):E0008445. https://doi.org/10.1371/2fjournal.Pntd.0008445
Saravanan P, Satishkumar KJM, Rasool TJ (2004) Detection of infectious bursal disease virus by elisa using an antipeptide antibody raised against Vp3 region. Acta Virol 48(1):39–45
Saxena VK, Deb R, Shrivastava S, Kantaraja C, Kumar A, Kumar S (2012) Functionalizing gold nanoparticles with bluetongue virus multiple peptide antigens utilizing gold-thiol interaction: a novel approach to develop pen side test. Res Vet Sci 93(3):1531–1536. https://doi.org/10.1016/J.Rvsc.2012.04.013
Schijman AG, Alonso-Padilla J, Longhi SA, Picado A (2022) Parasitological, serological and molecular diagnosis of acute and chronic chagas disease: from field to laboratory. Memórias Do Instituto Oswaldo Cruz 117:E200444. https://doi.org/10.1590/0074-02760200444
Serena NN, Boschero RA, Hospinal-Santiani M, Pacce VD, Costa JMDV, Magalhães FBD, Wiedmar C, Alban SM, Soccol CR, Thomaz-Soccol V (2022) High-performance immune diagnosis of tuberculosis: use of phage display and synthetic peptide in an optimized experimental design. J Immunol Methods 503:113242. https://doi.org/10.1016/J.Jim.2022.113242
Sespa (2023) Sespa Alerts the Population to Prevent Chagas Disease. http://www.Saude.Pa.Gov.Br/Sespa-Alerta-Populacao-Para-Prevencao-Da-Doenca-De-Chagas/. Accessed 9 Sep 2023
Shikanai-Yasuda MA, Carvalho NB (2012) Oral transmission of chagas disease. Clin Infect Dis 54(6):845–852. https://doi.org/10.1093/Cid/Cir956
Suárez C, Nolder D, García-Mingo A, Moore DAJ, Chiodini PL (2022) Diagnosis and clinical management of chagas disease: an increasing challenge in non-endemic areas. Res Rep Trop Med 13:25–40. https://doi.org/10.2147/2frrtm.S278135
Thomas MC, Fernández-Villegas A, Carrilero B, Marañón C, Saura D, Noya O, Segovia M, Alarcón DE, Noya B, Alonso C, López MC (2012) Characterization of an immunodominant antigenic epitope from trypanosoma cruzi as a biomarker of chronic chagas’ disease pathology. Clin Vaccine Immunol CVI 19(2):167–173. https://doi.org/10.1128/2fcvi.05566-11
Thomas MC, Longobardo MV, Carmelo E, Marañón C, Planelles L, Patarroyo ME, Alonso C, López MC (2001) Mapping of the antigenic determinants of the T. Cruzi Kinetoplastid Membrane Protein-11. identification of a linear epitope specifically recognized by human chagasic sera. Clin Exp Immunol 123(3):465–471. https://doi.org/10.1046/2fj.1365-2249.2001.01478.X
Vickery HB, Schmidt CLA (1931) The history of the discovery of the amino acids. Chem Rev 9(2):169–318. https://doi.org/10.1021/Cr60033a001
Who | World Health Organization (2023) Chagas disease (also known as American trypanosomiasis). https://www.who.int/news-room/fact-sheets/detail/chagas-disease-(american-trypanosomiasis)
Wieland T, Bodanszky M (1991) The world of peptides: a brief history of peptide chemistry. https://doi.org/10.1007/978-3-642-75850-8
Zhang X, Zhang X, Gao H, Qing G (2022) Phage display derived peptides for alzheimer’s disease therapy and diagnosis. Theranostics 12(5):2041–2062. https://doi.org/10.7150/2fthno.68636
Acknowledgments
The authors would thanks to CNPq, CAPES (code 001), FAPEMIG (APQ-02704-23, BPD-00647-22, RED-00067-23, RED-00193-23), UFSJ, UFMG and UCSM. EAFC, RCG, WOD and ASG thanks to CNPQ for their PQ/DT Fellowship. ASG and RCG thank to the Nacional Institute of Science and Technology on Industrial Biotechnology (INCT-BI) and the Nacional Institute of Science and Technology on Tropical Diseases (INCT-DT), Brazil, respectively. We are grateful to Randall Johnson to english revision of our manuscript.
Author information
Authors and Affiliations
Contributions
Anna Julia Ribeiro, Kamila Alves Silva, Lucas Da Silva Lopes, Carlos Ananias Aparecido Resende, Carolina Alves Petit Couto1, Isadora Braga Gandra, Isabela Amorim Gonçalves Pereira, Isabelle Caroline Dos Santos Barcelos, Sabrina Paula Pereira1, Sandra Rodrigues Xavier wrote the manuscript. Grasiele de Sousa Viera Tavares, Juliana Martins Machado and Mariana Campos Da Paz, revised and re-edited the manuscript Miguel Angel Chávez-Fumagalli, Eduardo Antonio Ferraz Coelho, Rodolfo Cordeiro Giunchetti, Ana Thereza Chaves, Walderez Ornelas Dutra, Ana Alice Maia Gonçalves1 And Alexsandro Sobreira Galdino conceptualiazed the rational of mini review article, supervised the students, write the article and revised and re-edited the manuscript Walderez Ornelas Dutra prepared the Figures Anna Julia Ribeiro prepared the Tables All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Handling editor: J. Gonzalez-Lopez.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ribeiro, A.J., Silva, K.A., Lopes, L.S. et al. The use of peptides for immunodiagnosis of human Chagas disease. Amino Acids 56, 35 (2024). https://doi.org/10.1007/s00726-024-03394-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00726-024-03394-6