Abstract
The utility for electron paramagentic resonance (EPR or ESR)-based radiation biodosimetry has received increasing recognition concerning its potential to assist in guiding the clinical management of medical countermeasures in individuals unwantedly exposed to injurious levels of ionizing radiation. Similar to any of the standard physical dosimetric methods currently employed for screening clinically significant radiation exposures, the EPR-based in vivo dosimetry approach would serve to complement and extend clinical assessments (e.g., blood analyses, cytogenetics, etc.), specifically to more accurately assign the extent of ionizing radiation exposure that individuals might have received. In the case of EPR biodosimetry of biological samples such as nails, teeth, and bones, the method has the capability of providing information on the physical dose at several specific bodily sites and perhaps additonal information on the homogeneity of the exposure as well as its overall magnitude. This information on radiation dose and distribution would be of significant value in providing medical management to given individuals at health risk due to radiation exposure. As these measurements provide information solely on physical measures of the radiation dose and not on the potential biological impact of a particular dose, they are complementary, albeit supplemental, to the array of currently available biologically based biodosimetry and clinical findings. In aggregate, these physical and biological measures of radiation exposure levels (dose) would most certainly provide additional, useful information for the effective medical management of radiation exposed individuals.
Similar content being viewed by others
1 Introduction
Radiological and nuclear accidents or malicious actions can lead to large amounts of potentially toxic ionizing radiation (IR) and radioactive materials being introduced into the environment [1]. Examples of such accidents are the Chernobyl accident in USSR which occurred on 26th April 1986, and the Fukushima Daiichi nuclear power plant accident in Japan that occurred on 11th March 2011 [2,3,4]. In addition, there are a large number of radiological accidents in the past that have exposed significant numbers of people [5,6,7]. Considerable effort has been employed for the development of measures to counteract the impact of such radiation, with recent significant progress in this field being made as of late. The effective deployment of these countermeasures would be greatly facilitated by the availability of methods to identify those at risk of having received significant radiation exposures. This requires methods that can specifically indicate the amount of radiation each person in a given exposure area has been subjected to. This could most effectively be done by assaying the degree of radiation-induced responses within persons suspected to have been exposed.
In this article, we summarize briefly the current state of radiation countermeasures and then assess the nature of biodosimetric techniques that could provide the information needed to utilize these countermeasures most effectively with an emphasis on in vivo EPR biodosimetry techniques.
2 Radiation Injury and Sub-syndromes for Organ System/Tissue Damage
The biological effects of IR have been grouped into two types: direct effects and indirect effects. Direct effects of IR occur when highly energetic physical–chemical intermediates react directly with the molecules of interest. The more important of these biological targets are DNA and related genomic molecules. DNA single-strand breaks, double-strand breaks, cross links, and several types of base damage are examples of the most important direct effects of IR. IR also interacts with free or bound intracellular water molecules to produce free radicals or reactive oxygen species that can diffuse into and then damage vital target biomolecules. This effect of IR is called indirect action of irradiation, and this mechanism is estimated to be responsible for two-thirds of the biological injury caused by high energy photons. It also appears that some significant component of the biological damage is associated with IR-elicited free radicals and associated oxidative processes of vital, targeted proteins and lipids [8]. Another potentially important indirect, but distinct mechanism is through free radicals generated by inflammatory cascades [9].
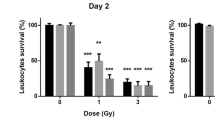
The clinical development of the IR-associated pathological syndromes that follow the above-mentioned IR-elicited molecular events depends on the extent of tissue-absorbed radiation dose, the rate and duration of exposure, the quality of radiation, and the distribution of the dose within the body. Exposure to a high dose of total-body or partial-body IR during a relatively short exposure window (i.e., at a high dose rate) leads to acute radiation syndrome (ARS). In addition to acute effects, there are other delayed or chronic type effects of irradiation [10]. ARS has been categorized into several related, but clinically distinct, sub-syndromes that arise following distinct, but overlapping ranges of exposures. These ARS sub-syndromes include: the hematopoietic ARS (H-ARS), elicited by IR doses in the range of ~ 1–6 Gy; the gastrointestinal ARS (GI-ARS), elicited by IR doses generally greater than 6 Gy; and the neurovascular sub-syndrome following very high IR doses, generally in excess of 10 Gy [11]. It should be noted that the neurovascular syndrome is considered generally to be clinically unmanageable, i.e., untreatable, and death occurs within 24–48 h of irradiation [12]. However, individuals exposed to lower doses of IR that manifest either H-ARS or GI-ARS are expected to benefit fully from therapeutic interventions with currently available, ‘state of clinical art’ medicinals (Table 1). As only H-ARS and GI-ARS have been considered to be treatable syndromes, they have received most of the attention for the research and development of radiation medical countermeasures.
3 Radiation Countermeasures
The effectiveness of currently available medicinals used to counter the detrimental health effects of IR is generally dependent on the timing of the treatment relative to exposure. Based on the timing of treatments, there are three broad categories to be considered: first, agents administered prior to exposure, i.e., given prophylactically, are intended to prevent injury; second, agents administered shortly after exposure, but prior to or at the early stages of injury development are intended to ‘mitigate’ injury and to lessen down-stream pathological effects; and third, agents given during the post-exposure period when injuries are fully manifested are considered ‘therapeutics’ [13]. Conceptually, all of these exposure categories and associated treatment options might be positively affected by access to individualized exposure assessments. However, in practice, it is only the second category, the early post-exposure period, where significant medical benefit might be gained via additional exposure information and, in turn, on the options of specific injury-mitigating agents that might be used clinically. The latter statement reflects the current ‘state of affairs’ of the areas of research, development, and fielding of new pharmaceuticals destined for countering unwanted radiological/nuclear exposure contingencies.
The statement below is a very brief synopsis of the different types and categories of pharmaceutical agents that are currently in play as medical countermeasures for unwanted radiation exposures and the subsequent injuries/diseases they foster. Several groups of agents are under investigation as countermeasures for ARS and have been recently reviewed [10, 14,15,16]. It needs to be pointed out, however, that this listing of drugs under development may not be as comprehensive as one would like due to the limited accessibility to recent incoming data about investigations conducted with such agents. This difficulty is a result of pharmaceutical firms with vested interests in safeguarding marketable agents for financial interest. Confidentiality and the ‘Intellectual Property’ rights of pharmaceutical companies and government agencies also limit accessibility. Nevertheless, a listing along with a brief overview of current R&D statuses of the more prominent of these agents are provided below.
3.1 FDA-Approved H-ARS Countermeasures
Only four medical radiation countermeasures including Neupogen, Neulasta, Leukine, and Nplate have been approved for H-ARS by the U.S. Food and Drug Administration (FDA) for human use, and all four agents are radiomitigators for post-exposure use [17,18,19,20,21,22,23,24,25]. The first three agents are available in the Strategic National Stockpile/vendor managed inventory [26, 27]. In general, there is no FDA-approved agent for use as a radioprotector for ARS. Furthermore, there is no agent approved by the FDA for the GI-ARS sub-syndrome. A large number of radiation countermeasures are at various stages of development and a few of them may get approved in due course of time (Table 1) [10, 16]. Although research and development of radiation countermeasures are usually intended for specific indications, i.e., for specific ARS sub-syndromes, there is recent discussion to use a ‘systems biology approach’ for R&D of new injury-countering medicinals. Such approaches include vascular injury/sepsis, ischemia/reperfusion, coagulopathy, cell death, and inflammation [28]. Despite its novelty, the latter approach has yet to yield safe and effective products with full regulatory approval.
3.2 Countermeasures for ARS with FDA Investigational New Drug (IND) Status
There are nine agents (AEOL 10,150, CLT-008, BIO 300, Entolimod, HemaMax, Neumune, OrbeShield, PLX-R18, and Recilib) that have US FDA IND status [16]. Some of these agents are currently moving forward in the regulatory approval process. There may be additional agents with IND that are not known (not reported publically), since the FDA does not make such information public and it is only up to drug sponsors to release such information publicly. There are additional agents that have been shown to have radioprotective efficacy and lack specific INDs for ARS, but have IND status for other indications that are already being evaluated clinically. In theory at least, such agents could possibly be developed and repurposed more readily as radiation countermeasures, as compared to agents developed de novo [29]. In this regard, all four fully FDA-approved countermeasures listed above were in clinical use for related indications prior to their FDA approval as radiomitigators for H-ARS as repurposed agents.
3.3 Countermeasures with FDA Approval for Limited Indications
A select number of agents have been approved by the FDA for limited indications, although they have not been approved specifically for ARS per se. Such agents that are clearly either protective, mitigative, or therapeutic in terms of countering radiation injury certainly include, but are not limited to, amifostine, interleukin-3 (IL-3), IL-11, palifermin, and erythropoietin [30,31,32,33,34]. Amifostine and palifermin fall into the category of ‘radioprotectors,’ while the other three listed cytokines are considered ‘radiomitigators’ due to their post-exposure use. Despite the lack of full regulatory approval, some of these agents have been used ‘off label’ and with largely positive outcomes in attempting to clinically manage radiological accident victims [7].
3.4 ARS Countermeasures Under Advanced Development
Advanced development of radiation medical countermeasures denotes the use of large animal models for evaluation and pharmacological scaling of the drug dose for humans. There are several radiation countermeasures that have demonstrated efficacy in both small and large animal models, but have not achieved IND status yet. Some of these agents include, but are not limited to γ-tocotrienol (GT3) [35], B-190 (Indralin) [36], recombinant thrombopoietin (rTPO) [37], daniplestim and Mpl ligand [38], leridistim (GM-CSF/IL-3 fusion protein) [39], PEGylated leridistim [40], myelopoietin (chimeric IL-3 and G-CSF receptor agonist) [41], promegapoietin-1a (chimeric IL-3 and Mpl-L receptor agonist) [42], and synthokine (synthetic cytokine/SC-55494) [43].
3.5 Other Promising Agents Under Development
There are a large number of agents being investigated for efficacy using small animal models. These agents are classified based on various classification criteria. The ‘Anti-oxidants and free radical scavengers’ group is one important group, represented by δ-tocotrienol, δ-tocopherol succinate, α-tocopherol succinate, superoxide dismutase, 3, 3'-diindolylmethane, oltipraz, pentoxifylline, tetrahydrobiopterin, PrC-210, Deinococcus Mn2+-decapeptide, ascorbic acid, cerium oxide (CeO2) nanoparticles, N-acetyl cysteine (NAC), and metformin [44,45,46,47,48,49,50,51,52,53,54,55].
‘Cytokines, chemokines, growth factors and hormones’ grouping is another important category. Several cytokines, chemokines, and growth factors mitigate radiation-induced tissue injury and accelerate tissue recovery after radiation exposure. Inhibitors of pro-inflammatory cytokines are known to reduce radiation-induced late tissue injury and fibrosis. Some cytokines and growth factors, either FDA-approved or at advanced stages of development, are discussed above. Additional agents are transforming growth factor (TGF), thrombopoietin (TPO) and related agents (eltrombopag/Promacta, ALXN4100TPO), megakaryocyte growth factor, fibroblast growth factor, epidermal growth factor (EGF), pleiotrophin, somatostatin analog (SOM230), insulin-like growth factor 1 (IGF-1), and CDX-301 [23, 56,57,58,59,60,61,62,63,64,65].
‘Inhibitors of various pathways’ grouping is yet another category. Agents belonging to this group of promising, protective drugs are generally inhibitors of several signaling pathways, especially those signaling pathways tied to radiation-induced cell death. Representative of this class or group are the angiotensin-converting enzyme (ACE) inhibitors, e.g., captopril; the phosphoinisitide-3 kinase (PI3K) inhibitors, e.g., LY294002; the histone deacetylase (HDAC) inhibitors, e.g., phenylbutyrate; the heat shock hydroxy-3-methylglutaryl-coenzyme-A (HMG-CoA) reductase inhibitors that include the statins; cyclin-dependent kinase inhibitors such as PD 0,332,991; prolyl hydroxylase inhibitors, e.g., dimethyloxallyl glycine (DMOG); and the glycogen synthase kinase-3 (GSK-3) inhibitors such as SB216763 and CHIR99021 [66,67,68,69,70,71,72,73,74].
Additional Radioprotective, Mitigative, and Therapeutic Agents. There are several other protein molecules that have demonstrated radioprotective or radiomitigative potential including R-spondin1 (Rspo1) and TP508 (rusalatide acetate, Chrysalin). In addition, there are other agents such as lipopolypeptides of mycoplasma origin (CBLB612 and CBLB613), lysophosphatidic acid receptor agonists, anti-ceramide antibody, fluoroquinolones, 7, 8-diacetoxy-4-methylthiocoumarin (DAMTC), and JP4-039 that have not previously been discussed [75,76,77,78,79,80,81,82].
Cellular Therapeutic Agents. Stem and progenitor cells have been shown to have the capacity to repair injured tissues, as well as a demonstrated capacity to secrete several protective/reparative cytokines and chemokines. The secreted cytokines promote tissue healing by stimulating both the repair and the regeneration of injured cells via an indirect cytokine/chemokine network. There are several types of cellular agents under investigations including mesenchymal stem cells, bone marrow stromal cells, mobilized stem cells, and early progenitors [83,84,85,86,87].
Plant Products. Several plant products alleviate the injurious effects of acute IR exposure, as demonstrated by a large number of investigations in various animal models using largely endpoints that measure either improved rates of survival or improved functions of specific organ systems. Some of these agents are Sea buckthorn (Hippophae rhamnoides—Hippophae) pulp, polyphenols, lycopene, resveratrol, caffeine, curcumin, and Ginkgo biloba extract [88,89,90,91,92,93,94,95].
4 Role of Biodosimetry for the Use of Radiation Countermeasures
The choice of ‘if and when’ to administer a given countermeasure is a complex matter because of logistics, timing, and the nature of the exposure. Because all medicinals pose some risk, there needs to be a commensurate benefit to justify their use. For there to be benefit from the use of a medical countermeasure for unwanted IR exposure, their use should be predicated upon ‘prior knowledge’ before they are administered. This primary ‘prior knowledge’ refers to not only the nature and condition of a potential or actual IR exposure, but also of its timing relative to the individual who would receive the countering medicinal. Biodosimetry could well provide this information that would be exceedingly useful in terms of the initial triage of individuals that might have been exposed unwantedly to IR following a given radiological/nuclear event. There are other types of information from biodosimetry demonstrating the extent of injury to organs and tissues, and potential variables in the properties of given biodosimetric assays that would likely impact not only the triage process itself, but more importantly, the ‘down-stream’ decisions related to medical treatment options.
Because some of the countermeasures under development are designed for specific organ systems, it would be of value if the biodosimetric assay could provide information on IR-dose distribution of the body or to specific organs at risk [96]. The validity of the results coming from a biodosimetric assay relative to time is another important factor in the decision-making about using countermeasures. This ‘timing’ of the administration of the countermeasure will vary most certainly with both the IR event itself, as well as with the accompanying logistics [97, 98]. Some biodosimetric techniques are not valid for a period of time after exposure and some have decreased validity over time. The potential for the presence of concomitant physical injuries and/or severe stress is another important factor that can affect the decision of deploying a countermeasure, because the assay may be confounded by the concomitant injury and/or the effectiveness of the countermeasure may be impacted.
For those countermeasures designed to treat H-ARS, it would be valuable to know if the exposure was uniform or not. If the IR exposure was non-uniform, it might indicate that selective, vital tissues/organ systems were spared; e.g., the sparing of bone marrow and, in turn, sparing of hematopoietic function. For subjects exposed to non-uniform IR doses with only estimated moderate or lower average doses, this might result in the postponement of the use of countermeasures. Therefore, a biodosimetric assay that could provide this information (regarding IR-dose distribution) would be especially valuable for the rational use and administration of given countermeasures aimed at specific organ systems. In part, this may already be possible with some of the currently available biodosimetric tools; e.g., in vivo EPR dosimetry and the use of nail and tooth samples to assess doses at different regions of the body, or perhaps employing quantitative, real-time molecular assessments of organ-specific genomic or proteomic changes induced by IR exposures [96, 99].
There are two principal types of biodosimetry: those based on physical–chemical changes elicited by IR within tissues, and those based on the biological responses to those IR-induced physical–chemical changes. They have different, but complementary characteristics. The physical–chemical changes occur immediately after irradiation and may persist for weeks (nails) or indefinitely (bones and teeth). They are usually not affected by the dose rate of IR, but rather provide information largely on the accumulated IR dose. They are unlikely to be affected by concomitant injury or prior physiological or pathological events that have occurred in the individual, and are potentially measurable immediately in the vicinity of the incident. They only report the dose at the site of the body where the IR exposure occurs and do not reflect the biological impact or its variation on the individual. They have some dependency on linear energy transfer. The biological response-based biodosimeters have the essential, added feature of reflecting the extent of biological damage associated with the IR exposure event. However, because they are biologically based, they tend to vary over time; the response sequence generally starts with a variable, post-exposure latency, followed by a period of increase, and then a period of decay as the biological indicator response is deactivated. Because these ‘bioindicators’ reflect the biology of the individual, they have the potential to vary among individuals in their time course and magnitude. They also have the potential to be impacted by concomitant injuries including stress.
5 Electron Paramagnetic Resonance (EPR) Dosimetry
In vitro EPR dosimetry, primarily using teeth, has been employed for the last 5 decades [100, 101]. In vitro tooth dosimetry is based on measuring the abundance of radiation-induced radicals entrapped in hydroxyapatite crystals within calcium components of enamel extracted from isolated teeth. Hydroxyapatite crystals contain carbonate impurities, which are transformed into stable CO2− radicals upon exposure to radiation [102]. The amount of CO2− radicals increase with an increase in absorbed dose, and can be easily detected, measured, and correlated to the absorbed dose of radiation. EPR dosimetry works well with highly mineralized materials that contain an abundance of calcium. EPR dosimetry, which is based on the use of concentrated extracted enamel, can offer approximations of the absorbed dose in 0.5 Gy increments in the range from 1 Gy to more than 10 Gy [103, 104]. The lowest limit of detection, as well as the accuracy, may improve with the advancements in the resonator and also with the algorithm for acquiring and calculating the dose absorbed. In vitro EPR measurements with nail clippings have also been utilized in several accidents involving a few individuals. While the in vitro EPR assays have been useful in the timely analysis of radiation accidents involving only a few people, they are, however, not practical at this point in time for the purpose of guiding countermeasures. On the other hand, the long stability of the EPR signal in materials present in the surrounding area of an incidence, tooth enamel, and nails make this technique exceedingly useful for dose reconstruction. This is largely due to the fact that dose reconstruction can be accomplished long after a radiological event, from a few months to years [102, 105, 106]. Dose reconstructions using EPR spectroscopy have been accomplished in the case of atomic bomb survivors of Nagasaki and Hiroshima, inhabitants affected by the Chernobyl accident, Southern Ural region survivors of accidents in the Soviet Union, and radiation workers [107, 108]. Although a significant proportion of studies involving human exposures have been conducted using extracted teeth and EPR dosimetry, comparable dosimetric research has also been devoted to wildlife within given regions of exposure, e.g., wildlife in areas surrounding Chernobyl [109].
Focusing on the unmet needs related to basic triage procedures and for subsequent application of given medical countermeasures, the in vivo nail dosimetry (as opposed to either in vitro or in vivo tooth/enamel-based dosimetry) approach seems most valuable [96, 99], and therefore, we describe it here in more detail, especially as it relates to the potential of the technology to guide the application of any/all post-IR exposure medical procedures. However, as promising as in vivo tooth dosimetry might be, especially for the initial triage for large-scale radiation events, the dosimetric technique is limited, because it provides a dose measurement of a single site on the body (i.e., at the mouth/head). By contrast, the less-developed and tested in vivo nail dosimetry assay procedure might ultimately prove to be useful by providing additional IR-dose estimates for multiple, distant body sites. Due to the lower EPR signals in irradiated nails compared to teeth, in vivo nail dosimetry has been developed to take the measurements at a higher frequency than is used for the in vivo analyses of teeth (9.5 GHz for nails versus 1.2 GHz for tooth) [99, 101, 110]. Nevertheless, it would appear that the ‘in vivo EPR biodosimetry of nails’ assay has a number of characteristic features that would be valuable for biodosimetry when there is a significant potential for non-homogeneous exposures. Specifically, in early preliminary results, in vivo EPR of nails was shown to have the potential for having sufficient sensitivity to provide information on radiation dose levels at four distinct anatomical sites. The EPR measurements require only a short time, currently less than 5 min, with the potential to obtain the data simultaneously at four separate locations. These measurements, even if the exact positions of the hands and feet at the time of irradiation may have some uncertainty, could provide information useful in guiding triage decisions when homogeneity of exposure is an important consideration in determining whether to use the countermeasure. However, the utility of the in vivo EPR/nail dosimetry assay is clearly limited in providing information on the dose to specific organs. Such dose estimates could come, no doubt, from the application of advanced biological response assays that are currently in play; e.g., real-time, high-throughput measures of IR-responsive biomolecules, such as blood plasma levels of Ftl3 ligand for estimates of bone marrow injury, or of selective metabolites such as citrulline or oxysterols, as measures of GI tissue damage or liver damage, respectively [111,112,113].
There are many key factors that need to be considered before in vivo EPR could be operationalized and some important caveats in its use. First, while in concept the results to date appear promising, there are many practical aspects remaining to be finalized. Most importantly, these include determination of the limits of dose resolution and the construction of a deployable instrument that could take the simultaneous measurements quickly while being operated by non-expert operators. There is also a need to establish the way in which the in vivo EPR/nail technique would be utilized in actual scenarios. Deployment of the system in the field as close as possible in time and location to the actual event for immediate triage would be preferable.
Finally, it is also important to point out what information the in vivo EPR-based biodosimetry measurements convey and what they do not convey; namely, they indicate the total dose at the site of measurement, but they do not reflect the dose rate of exposure, nor do they reflect IR-associated variations in biological effects. In addition, while the EPR dose responses of the nails are similar for all pertinent energies of X and gamma rays, the response to neutrons has not been fully characterized.
6 Concluding Comments
Advances over the last several decades in IR-associated biodosimetric technologies have resulted in both improved basic triage procedures as well as effectiveness of clinical management protocols that necessarily follow radiological/nuclear IR exposure events [114, 115]. These advanced biodosimetry technologies are wide-ranging and encompass systems of newer areas of biological investigation (e.g., studies on genomics, proteomics, metabolomics, and transcriptomics), but are also an extension of older, well-worked, laborious biodosimetry systems (e.g., lymphocyte kinetics) using highly efficient, automated platforms [115]. Continued development of field-deployable EPR technology also falls into this category of ‘significant biodosimetric achievements.’ Clearly, past biodosimetry assessments based on in vivo/vitro EPR/tooth analyses have proven to be of worth and are not only useful, but are essential in terms of ‘IR dose reconstruction’ following significant and unwanted IR exposure events [116]. As highlighted here in this paper, a continued effort to extend and improve this EPR capability using finger/digit nails (as opposed to teeth) from IR exposed subjects shows promise. IR-dose estimates coming from ‘in vivo EPR nail’ dosimetry provide useful information on the total dose and dose distribution rapidly following unwanted IR exposures and with sufficient accuracy to compliment the current array of biodosimetric assays (as indicated above) [117]. As such, we conclude that in vivo EPR nail dosimetry has the characteristics to be a very effective, complementary tool for this purpose. Further and in aggregate, these dosimetric assays serve to facilitate ongoing clinical management procedures, especially as they are related to both the timing and application of potential life-saving, injury-countering medicinals. Finally and most importantly, despite the promise of in vivo EPR-based dosimetry, the optimal use of the dosimetric assessments generated (i.e., information from EPR measurements of nails and teeth) should be done in concert with other information such as biologically based biodosimetry, physical estimates of dose, clinical measurements, and observations, etc. While the potential value of in vivo EPR dosimetry is high, its realization will require additional developments to confirm and improve its dosimetric properties and to then incorporate them into a device that can be readily deployed and operated by non-expert users [96].
References
K. Koarai, Y. Kino, A. Takahashi, T. Suzuki, Y. Shimizu, M. Chiba, K. Osaka, K. Sasaki, T. Fukuda, E. Isogai, H. Yamashiro, T. Oka, T. Sekine, M. Fukumoto, H. Shinoda, Sci Rep 6, 24077 (2016)
T. Ohnishi, Radiat Res 177, 1 (2012)
D. Bard, P. Verger, P. Hubert, Epidemiol Rev 19, 187 (1997)
M. Rahu, Eur J Cancer 39, 295 (2003)
R.E. Goans, E.C. Holloway, M.E. Berger, R.C. Ricks, Health Phys 72, 513 (1997)
G. Reeves, Health Phys 106, 699 (2014)
International Atomic Energy Agency, IAEA publications on radiation response (2014), http://www-pub.iaea.org/books/IAEABooks/Publications_on_Accident_Response. (Accessed 20 Feb 2014)
M.J. Daly, DNA Repair (Amst) 11, 12 (2012)
J.H. Kim, K.A. Jenrow, S.L. Brown, Radiat Oncol J 32, 103 (2014)
V.K. Singh, T.M. Seed, Int J Radiat Biol 93, 851 (2017)
D.G.C. McCann, Am J Clin Med 3, 13 (2006)
Armed Forces Radiobiology Research Institute, Medical Management of Radiological Casualities (Armed Forces Radiobiology Research Institute, Bethesda, MD, USA, 2013)
H.B. Stone, J.E. Moulder, C.N. Coleman, K.K. Ang, M.S. Anscher, M.H. Barcellos-Hoff, W.S. Dynan, J.R. Fike, D.J. Grdina, J.S. Greenberger, M. Hauer-Jensen, R.P. Hill, R.N. Kolesnick, T.J. MacVittie, C. Marks, W.H. McBride, N. Metting, T. Pellmar, M. Purucker, M.E. Robbins, R.H. Schiestl, T.M. Seed, J.E. Tomaszewski, E.L. Travis, P.E. Wallner, M. Wolpert, D. Zaharevitz, Radiat Res 162, 711 (2004)
V.K. Singh, M. Garcia, T.M. Seed, Int J Radiat Biol 93, 870 (2017)
V.K. Singh, B.K. Hanlon, P.T. Santiago, T.M. Seed, Int J Radiat Biol 93, 885 (2017)
V.K. Singh, T.M. Seed, Expert Opin Pharmacother 21, 317 (2020)
A.M. Farese, T.J. MacVittie, Drugs Today (Barc) 51, 537 (2015)
V.K. Singh, T.M. Seed, Drugs Today (Barc) 54, 679 (2018)
R.P. Gale, J.O. Armitage, Blood Rev 1, 100690 (2020)
Y. Zhong, M. Pouliot, A.M. Downey, C. Mockbee, D. Roychowdhury, W. Wierzbicki, S. Authier, Int J Radiat Biol (2020). https://doi.org/10.1080/09553002.2019.1673499 (In press)
K.G. Hankey, A.M. Farese, E.C. Blaauw, A.M. Gibbs, C.P. Smith, B.P. Katz, Y. Tong, K.L. Prado, T.J. MacVittie, Radiat Res 183, 643 (2015)
N.P. Clayton, R.C. Khan-Malek, C.A. Dangler, D. Zhang, A. Ascah, M. Gains, B. Gardner, C. Mockbee, J.M. Keutzer, J. McManus, S. Authier, Radiat. Res. 195, 191 (2020)
K. Wong, P.Y. Chang, M. Fielden, A.M. Downey, D. Bunin, J. Bakke, J. Gahagen, L. Iyer, S. Doshi, W. Wierzbicki, S. Authier, Int J Radiat Biol 96, 155 (2020)
K. Wong, D.I. Bunin, K. Bujold, H.S. Javitz, J. Bakke, J. Gahagen, W. Wierzbicki, D.A. Andreasen, S. Authier, and P.Y. Chang, Annual conference of radiation research society (2020).
V.K. Singh, T.M. Seed, Int J Radiat Biol (2021). https://doi.org/10.1080/09553002.2021.1969054
Centers for Disease Control and Prevention, Strategic National Stockpile (SNS), (2014), http://www.cdc.gov/phpr/stockpile/stockpile.htm. (Accessed 15 Feb 2014)
U.S. Department of Health & Human Services, HHS boosts stockpile of products to treat acute radiation syndrome. (2013). http://www.hhs.gov/news/press/2013pres/09/20130926a.html. (Accessed 12 Feb 2014)
E. Davis, BARDA Industry Day (2020).
A.L. DiCarlo, D.R. Cassatt, W.E. Dowling, J.L. Esker, J.A. Hewitt, O. Selivanova, M.S. Williams, P.W. Price, Radiat Res 190, 659 (2018)
V.K. Singh, T.M. Seed, Expert Opin Drug Saf 18, 1077 (2019)
S. Vadhan-Raj, J.D. Goldberg, M.A. Perales, D.P. Berger, M.R. van den Brink, J Cell Mol Med 17, 1371 (2013)
H.T. Lee, S.W. Park, M. Kim, A. Ham, L.J. Anderson, K.M. Brown, V.D. D’Agati, G.N. Cox, Am J Physiol Renal Physiol 303, F1216 (2012)
Y.F. Cui, H. Yang, Q.L. Luo, B. Dong, X.L. Liu, H. Xu, B.Z. Mao, D.W. Wang, Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 16, 22 (2004)
M. Drouet, N. Grenier, F. Herodin, Eur Cytokine Netw 23, 56 (2012)
V.K. Singh, S. Kulkarni, O.O. Fatanmi, S.Y. Wise, V.L. Newman, P.L. Romaine, H. Hendrickson, J. Gulani, S.P. Ghosh, K.S. Kumar, M. Hauer-Jensen, Radiat Res 185, 285 (2016)
M.V. Vasin, L.F. Semenov, N.N. Suvorov, V.V. Antipov, I.B. Ushakov, L.A. Ilyin, B.A. Lapin, J Radiat Res 55, 1048 (2014)
G. Wagemaker, K.J. Neelis, S.C.C. Hartong, A.W. Wognum, G.R. Thomas, P.J. Fielder, D.L. Eaton, Stem Cells 16(Suppl 2), 127 (1998)
A.M. Farese, T.J. MacVittie, L.B. Lind, W.G. Smith, J.P. McKearn, Stem Cells 16(Suppl 2), 143 (1998)
A.M. Farese, D.B. Casey, W.G. Smith, R.M. Vigneulle, J.P. McKearn, T.J. MacVittie, Stem Cells 19, 522 (2001)
A.M. Farese, D.B. Casey, R.M. Vigneulle, N.R. Siegel, R.F. Finn, J.A. Klover, W.G. Smith, J.P. McKearn, T.J. MacVittie, Stem Cells 19, 514 (2001)
T.J. MacVittie, A.M. Farese, W.G. Smith, C.M. Baum, E. Burton, J.P. McKearn, Blood 95, 837 (2000)
A.M. Farese, W.G. Smith, J.G. Giri, N. Siegel, J.P. McKearn, T.J. MacVittie, Stem Cells 19, 329 (2001)
A.M. Farese, F. Herodin, J.P. McKearn, C. Baum, E. Burton, T.J. MacVittie, Blood 87, 581 (1996)
V.K. Singh, L.A. Beattie, T.M. Seed, J Radiat Res 54, 973 (2013)
M.W. Epperly, J.E. Gretton, C.A. Sikora, M. Jefferson, M. Bernarding, S. Nie, J.S. Greenberger, Radiat Res 160, 568 (2003)
S. Fan, Q. Meng, J. Xu, Y. Jiao, L. Zhao, X. Zhang, F.H. Sarkar, M.L. Brown, A. Dritschilo, E.M. Rosen, Proc Natl Acad Sci USA 110, 18650 (2013)
S.G. Kim, S.Y. Nam, C.W. Kim, Biochem Pharmacol 55, 1585 (1998)
M. Berbee, Q. Fu, S. Garg, S. Kulkarni, K.S. Kumar, M. Hauer-Jensen, Radiat Res 175, 297 (2011)
M. Berbee, Q. Fu, K.S. Kumar, M. Hauer-Jensen, Curr Drug Targets 11, 1366 (2010)
D.D. Peebles, C.M. Soref, R.R. Copp, A.L. Thunberg, W.E. Fahl, Radiat Res 178, 57 (2012)
P. Gupta, M. Gayen, J.T. Smith, E.K. Gaidamakova, V.Y. Matrosova, O. Grichenko, B. Knollmann-Ritschel, M.J. Daly, J.G. Kiang, R.K. Maheshwari, PLoS ONE 11, e0160575 (2016)
T. Sato, M. Kinoshita, T. Yamamoto, M. Ito, T. Nishida, M. Takeuchi, D. Saitoh, S. Seki, Y. Mukai, PLoS ONE 10, e0117020 (2015)
P.T. Xu, B.W. Maidment 3rd., V. Antonic, I.L. Jackson, S. Das, A. Zodda, X. Zhang, S. Seal, Z. Vujaskovic, Radiat Res 185, 516 (2016)
R. Neal, R.H. Matthews, P. Lutz, N. Ercal, Free Radic Biol Med 34, 689 (2003)
R.C. Miller, J.S. Murley, D.J. Grdina, Radiat Res 181, 464 (2014)
E.J. Chung, K. Hudak, J.A. Horton, A. White, B.T. Scroggins, S. Vaswani, D. Citrin, Radiat Res 182, 350 (2014)
M. Satyamitra, L. Cary, D. Dunn, G.P. Holmes-Hampton, L.J. Thomas, S.P. Ghosh, Sci Rep 10, 1757 (2020)
G.S. Howarth, R. Fraser, C.L. Frisby, M.B. Schirmer, E.K. Yeoh, Scand J Gastroenterol 32, 1118 (1997)
Q. Fu, M. Berbee, M. Boerma, J. Wang, H.A. Schmid, M. Hauer-Jensen, Radiat Res 171, 698 (2009)
J. Pejchal, Z. Sinkorova, A. Tichy, A. Kmochova, K. Durisova, K. Kubelkova, M. Pohanka, J. Bures, I. Tacheci, K. Kuca, J. Vavrova, Int J Radiat Biol 91, 703 (2015)
H.A. Himburg, J.R. Harris, T. Ito, P. Daher, J.L. Russell, M. Quarmyne, P.L. Doan, K. Helms, M. Nakamura, E. Fixsen, G. Herradon, T. Reya, N.J. Chao, S. Harroch, J.P. Chute, Cell Rep 2, 964 (2012)
K. Casey-Sawicki, M. Zhang, S. Kim, A. Zhang, S.B. Zhang, Z. Zhang, R. Singh, S. Yang, S. Swarts, S. Vidyasagar, L. Zhang, A. Zhang, P. Okunieff, Health Phys 106, 704 (2014)
M.W. Schuster, R. Beveridge, D. Frei-Lahr, C.N. Abboud, S. Cruickshank, M. Macri, D. Menchaca, J. Holden, E.K. Waller, Exp Hematol 30, 1044 (2002)
C.L. Erickson-Miller, E. Delorme, S.S. Tian, C.B. Hopson, A.J. Landis, E.I. Valoret, T.S. Sellers, J. Rosen, S.G. Miller, J.I. Luengo, K.J. Duffy, J.M. Jenkins, Stem Cells 27, 424 (2009)
M. Satyamitra, E. Lombardini, J. Graves 3rd., C. Mullaney, P. Ney, J. Hunter, K. Johnson, P. Tamburini, Y. Wang, J.P. Springhorn, V. Srinivasan, Radiat Res 175, 746 (2011)
X. Zhao, H. Yang, G. Jiang, M. Ni, Y. Deng, J. Cai, Z. Li, F. Shen, X. Tao, J Radiat Res 55, 257 (2014)
E.A. McCart, Y.H. Lee, J. Jha, O. Mungunsukh, W.B. Rittase, T.A. Summers Jr., J. Muir, R.M. Day, Sci Rep 9, 2198 (2019)
C.M. Taniguchi, Y.R. Miao, A.N. Diep, C. Wu, E.B. Rankin, T.F. Atwood, L. Xing, A.J. Giaccia, Sci Transl Med 6, 236ra64 (2014)
J.S. Lazo, E.R. Sharlow, M.W. Epperly, A. Lira, S. Leimgruber, E.M. Skoda, P. Wipf, J.S. Greenberger, J Pharmacol Exp Ther 347, 669 (2013)
L. Wei, B.J. Leibowitz, X. Wang, M. Epperly, J. Greenberger, L. Zhang, J. Yu, J Clin Invest 126, 4076 (2016)
C.L. Lee, W.E. Lento, K.D. Castle, N.J. Chao, D.G. Kirsch, Radiat Res 181, 445 (2014)
X. Wang, L. Wei, J.M. Cramer, B.J. Leibowitz, C. Judge, M. Epperly, J. Greenberger, F. Wang, L. Li, M.G. Stelzner, J.C. Dunn, M.G. Martin, E. Lagasse, L. Zhang, J. Yu, Sci Rep 5, 8566 (2015)
X. Lu, D. Nurmemet, D.L. Bolduc, T.B. Elliott, J.G. Kiang, Cell Biosci 3, 36 (2013)
A.C. Miller, S. Cohen, M. Stewart, R. Rivas, P. Lison, Radiat Environ Biophys 50, 585 (2011)
V.K. Singh, E.J. Ducey, O.O. Fatanmi, P.K. Singh, D.S. Brown, A. Purmal, V.V. Shakhova, A.V. Gudkov, E. Feinstein, A. Shakhov, Radiat Res 177, 628 (2012)
A.N. Shakhov, V.K. Singh, F. Bone, A. Cheney, Y. Kononov, P. Krasnov, T.K. Bratanova-Toshkova, V.V. Shakhova, J. Young, M.M. Weil, A. Panoskaltsis-Mortari, C.M. Orschell, P.S. Baker, A. Gudkov, E. Feinstein, PLoS ONE 7, e33044 (2012)
R. Patil, E. Szabo, J.I. Fells, A. Balogh, K.G. Lim, Y. Fujiwara, D.D. Norman, S.C. Lee, L. Balazs, F. Thomas, S. Patil, K. Emmons-Thompson, A. Boler, J. Strobos, S.W. McCool, C.R. Yates, J. Stabenow, G.I. Byrne, D.D. Miller, G.J. Tigyi, Chem Biol 22, 206 (2015)
W. Deng, Y. Kimura, V. Gududuru, W. Wu, A. Balogh, E. Szabo, K.E. Thompson, C.R. Yates, L. Balazs, L.R. Johnson, D.D. Miller, J. Strobos, W.S. McCool, G.J. Tigyi, Radiat Res 183, 465 (2015)
K. Kim, J.M. Pollard, A.J. Norris, J.T. McDonald, Y. Sun, E. Micewicz, K. Pettijohn, R. Damoiseaux, K.S. Iwamoto, J.W. Sayre, B.D. Price, R.A. Gatti, W.H. McBride, Clin Cancer Res 15, 7238 (2009)
K. Venkateswaran, A. Shrivastava, P.K. Agrawala, A. Prasad, N. Kalra, P.R. Pandey, K. Manda, H.G. Raj, V.S. Parmar, B.S. Dwarakanath, Sci Rep 6, 37305 (2016)
M.W. Epperly, J.R. Sacher, T. Krainz, X. Zhang, P. Wipf, M. Liang, R. Fisher, S. Li, H. Wang, J.S. Greenberger, In Vivo 31, 39 (2017)
J.A. Rotolo, C.S. Fong, S. Bodo, P.K.B. Nagesh, J. Fuller, T. Sharma, A. Piersigilli, Z. Zhang, Z. Fuks, V.K. Singh, V.K. Kolesnick, JCI Insight 6, e145380 (2021)
S. Saha, P. Bhanja, R. Kabarriti, L. Liu, A.A. Alfieri, C. Guha, PLoS ONE 6, e24072 (2011)
D.J. Prockop, Mol Ther 21, 1116 (2013)
A.S. Abdel-Mageed, A.J. Senagore, D.W. Pietryga, R.H. Connors, T.A. Giambernardi, R.V. Hay, W. Deng, Blood 113, 1201 (2009)
V.K. Singh, D.S. Brown, T.C. Kao, T.M. Seed, Exp Hematol 38, 61 (2010)
H.X. Chen, H. Xiang, W.H. Xu, M. Li, J. Yuan, J. Liu, W.J. Sun, R. Zhang, J. Li, Z.Q. Ren, X.M. Zhang, B. Du, J. Wan, B.Y. Wu, Q. Zeng, K.L. He, C. Yang, Hum Gene Ther 28, 523 (2017)
R. Pathak, S.K. Shah, M. Hauer-Jensen, Int J Radiat Biol 95, 493 (2019)
R. Chawla, R. Arora, S. Singh, R.K. Sagar, R.K. Sharma, R. Kumar, A. Sharma, M.L. Gupta, S. Singh, J. Prasad, H.A. Khan, A. Swaroop, A.K. Sinha, A.K. Gupta, R.P. Tripathi, P.S. Ahuja, J Med Food 10, 101 (2007)
O. Benavente-Garcia, J. Castillo, J. Lorente, M. Alcaraz, J Med Food 5, 125 (2002)
H.N. Saada, R.G. Rezk, N.A. Eltahawy, Phytother Res 24(Suppl 2), S204 (2010)
M. Sabisz, A. Skladanowski, Curr Pharm Biotechnol 9, 325 (2008)
J.L. Ryan, C.E. Heckler, M. Ling, A. Katz, J.P. Williams, A.P. Pentland, G.R. Morrow, Radiat Res 180, 34 (2013)
F.V. DeFeudis, V. Papadopoulos, K. Drieu, Fundam Clin Pharmacol 17, 405 (2003)
B. Farhood, G. Hassanzadeh, P. Amini, D. Shabeeb, A.E. Musa, E. Khodamoradi, M. Mohseni, A. Aliasgharzadeh, H. Moradi, M. Najafi, Antiinflamm Antiallergy Agents Med Chem 19, 413 (2020)
H.M. Swartz, A.B. Flood, V.K. Singh, S.G. Swarts, Health Phys 119, 72 (2020)
H.M. Swarts, B.B. Williams, R.J. Nicolade, E. Demidenko, A.B. Flood, Radiat. Meas. 46, 742 (2011)
A.B. Flood, R.J. Nicolalde, E. Demidenko, B.B. Williams, A. Shapiro, A.L. Wiley Jr., H.M. Swartz, Radiat Meas 46, 916 (2011)
S.G. Swarts, J.W. Sidabras, O. Grinberg, D.S. Tipikin, M.M. Kmiec, S.V. Petryakov, W. Schreiber, V.A. Wood, B.B. Williams, A.B. Flood, H.M. Swartz, Health Phys 115, 140 (2018)
J.M. Brady, N.O. Aarestad, H.M. Swartz, Health Phys 15, 43 (1968)
H.M. Swartz, Radiat Prot Dosimetry 172, 3 (2016)
International Atomic Energy Agency, Use of electron paramagnetic resonance dosimetry with tooth enamel for retrospective dose assessment, TECDOC-1331, (2002), https://www-pub.iaea.org/MTCD/Publications/PDF/te_1331_web.pdf. (Accessed 27 Nov 2002)
P. Fattibene, F. Callens, Appl Radiat Isot 68, 2033 (2010)
A. Romanyukha, F. Trompier, R.A. Reyes, Radiat Environ Biophys 53, 305 (2014)
S. Toyoda, Radiat Meas 37, 341 (2003)
R.F. Khan, W.J. Rink, D.R. Boreham, Appl Radiat Isot 59, 189 (2003)
A. Harshman, T. Johnson, Health Phys 115, 600 (2018)
A.A. Romanyukha, D. Regulla, E. Vasilenko, A. Wieser, Appl Radiat Isot 45, 1195 (1994)
D.A. Bugai, R.D. Waters, S.P. Dzhepo, A.S. Skal’skij, Health Phys 71, 9 (1996)
X. He, J. Gui, T.P. Matthews, B.B. Williams, S.G. Swarts, O. Grinberg, J. Sidabras, D.E. Wilcox, H.M. Swartz, Radiat Meas 46, 882 (2011)
J.M. Bertho, L. Roy, M. Souidi, M. Benderitter, Y. Gueguen, J.J. Lataillade, M. Prat, T. Fagot, T. De Revel, P. Gourmelon, Radiat Res 169, 543 (2008)
J.M. Bertho, L. Roy, Br J Radiol 82, 764 (2009)
J.M. Bertho, L. Roy, M. Souidi, M. Benderitter, E. Bey, R. Racine, T. Fagot, P. Gourmelon, Biomarkers 14, 94 (2009)
E.E. Milner, E.G. Daxon, M.T. Anastasio, J.T. Nesler, R.L. Miller, W.F. Blakely, Health Phys 110, 370 (2016)
M. Sproull, K. Camphausen, Radiat Res 186, 423 (2016)
B.B. Williams, R. Dong, A.B. Flood, O. Grinberg, M. Kmiec, P.N. Lesniewski, T.P. Matthews, R.J. Nicolalde, T. Raynolds, I.K. Salikhov, H.M. Swartz, Radiat Meas 46, 772 (2011)
A. Marciniak, B. Ciesielski, Appl Spect Rev 51, 73 (2016)
Acknowledgements
The opinions or assertions contained herein are the private views of the authors and are not necessarily those of the Uniformed Services University of the Health Sciences or the Department of Defense. The mention of specific therapeutic agents or biodosimetry devices does not constitute endorsement by the U.S. Department of Defense, and trade names are used only for the purpose of clarification. We are thankful to Ms. Alana Carpenter for editing the manuscript. We apologize to those having contributed substantially to the topics discussed herein, but that we were unable to cite due to space constraints.
Funding
The authors gratefully acknowledge the research support from the Armed Forces Radiobiology Research Institute, Uniformed Services University of the Health Sciences as intramural project (AFR-B2-9173) to VKS.
Author information
Authors and Affiliations
Contributions
VKS and TMS drafted the manuscript and reviewed it. All authors have reread and contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
HMS is co-owner of Clin-EPR, LLC, which manufactures and sells clinical EPR instruments for investigational use. The other authors (VKS and TMS) have no relevant affiliations or financial involvement with any organization or entity with financial interests or conflicts with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singh, V.K., Swartz, H.M. & Seed, T.M. Radiation Medical Countermeasures and Use of EPR Biodosimetry to Facilitate Effectiveness of Applied Clinical Procedures. Appl Magn Reson 53, 289–303 (2022). https://doi.org/10.1007/s00723-021-01444-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00723-021-01444-w