Abstract
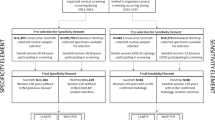
HPV types with high viral load are associated with cervical abnormalities. However, viral load measurements and concordance of HPV loads and viral mRNA have not been demonstrated for all high-risk/possibly high-risk (HR-/pHR-)HPV types in cervical cancer (CxCa). Especially, the biological role of co-infecting HR-/pHR-HPV types with low viral load has not been thoroughly investigated. Using BSGP5+/6+-PCR/MPG genotyping, we analyzed viral loads for all currently defined 51 mucosal HPV types in 74 cervical smears from patients with CxCa and compared this data with HPV DNA and mRNA status in these patients’ corresponding CxCa tissues. All cervical smear/tissue pairs were HPV DNA+. Overall HPV type agreement within pairs was 99% (complete agreement in 50%, partial agreement in 49%, and complete disagreement in 1% of cases). The proportion of multiple HPV types was significantly higher in smears compared to tissues (p<0.0001). High load HPV infections (>1 copy/cell) were found in 88% of HPV DNA+ smears, and were significantly associated with the presence of respective HPV DNA (kappa=0.685, CI: 0.567-0.803), and HPV mRNA (kappa=0.693, CI: 0.566-0.820) in CxCa tissues. In total, 93% (67/72) of high load HR-/pHR-HPV infections identified in smears were also present in corresponding CxCa tissues, and 93% (62/67) of these were HPV mRNA+. On the other hand, 78% (42/54) of low load HR-/pHR-HPV infections identified in smears were not detectable in tissues, including 11 out of 15 low load HPV16 infections. This data demonstrates that the presence of high HPV loads in CxCa smears predicts biologically active HR-/pHR-HPV types in tumor tissues.




Similar content being viewed by others
References
Bernard HU, Burk RD, Chen Z, van Doorslaer K, Hausen H, de Villiers EM (2010) Classification of papillomaviruses (PVs) based on 189 PV types and proposal of taxonomic amendments. Virology 401(1):70–79. doi:10.1016/j.virol.2010.02.002
de Villiers EM (2013) Cross-roads in the classification of papillomaviruses. Virology 445(1–2):2–10. doi:10.1016/j.virol.2013.04.023
IARC (2011) Human papillomaviruses. IARC Monogr Eval Carcinog Risks Hum. Rev Hum Carcinog Part B Biol Agents 100B:1–475
Schiffman M, Clifford G, Buonaguro FM (2009) Classification of weakly carcinogenic human papillomavirus types: addressing the limits of epidemiology at the borderline. Infect Agent Cancer 4:8. doi:10.1186/1750-9378-4-8
Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V, Group WHOIAfRoCMW (2009) A review of human carcinogens—Part B: biological agents. Lancet Oncol 10(4):321–322
Halec G, Alemany L, Lloveras B, Schmitt M, Alejo M, Bosch FX, Tous S, Klaustermeier JE, Guimera N, Grabe N, Lahrmann B, Gissmann L, Quint W, Bosch FX, de Sanjose S, Pawlita M, Retrospective International S, Group HPVTTS (2014) Pathogenic role of the eight probably/possibly carcinogenic HPV types 26, 53, 66, 67, 68, 70, 73 and 82 in cervical cancer. J Pathol 234(4):441–451. doi:10.1002/path.4405
Hampson L, Martin-Hirsch P, Hampson IN (2015) An overview of early investigational drugs for the treatment of human papilloma virus infection and associated dysplasia. Expert Opin Investig Drugs 24(12):1529–1537. doi:10.1517/13543784.2015.1099628
Wright TC Jr, Schiffman M, Solomon D, Cox JT, Garcia F, Goldie S, Hatch K, Noller KL, Roach N, Runowicz C, Saslow D (2004) Interim guidance for the use of human papillomavirus DNA testing as an adjunct to cervical cytology for screening. Obstet Gynecol 103(2):304–309
Verhelst S, Poppe WA, Bogers JJ, Depuydt CE (2016) Serial measurement of type-specific human papillomavirus load enables classification of cervical intraepithelial neoplasia lesions according to occurring human papillomavirus-induced pathway. Eur J Cancer Prev. doi:10.1097/CEJ.0000000000000241
Arbyn M, Benoy I, Simoens C, Bogers J, Beutels P, Depuydt C (2009) Prevaccination distribution of human papillomavirus types in women attending at cervical cancer screening in Belgium. Cancer Epidemiol Biomark Prev 18(1):321–330. doi:10.1158/1055-9965.EPI-08-0510
Snijders PJ, Hogewoning CJ, Hesselink AT, Berkhof J, Voorhorst FJ, Bleeker MC, Meijer CJ (2006) Determination of viral load thresholds in cervical scrapings to rule out CIN 3 in HPV 16, 18, 31 and 33-positive women with normal cytology. Int J Cancer 119(5):1102–1107
Gravitt PE, Kovacic MB, Herrero R, Schiffman M, Bratti C, Hildesheim A, Morales J, Alfaro M, Sherman ME, Wacholder S, Rodriguez AC, Burk RD (2007) High load for most high risk human papillomavirus genotypes is associated with prevalent cervical cancer precursors but only HPV16 load predicts the development of incident disease. Int J Cancer 121(12):2787–2793. doi:10.1002/ijc.23012
Hesselink AT, Berkhof J, Heideman DA, Bulkmans NW, van Tellingen JE, Meijer CJ, Snijders PJ (2009) High-risk human papillomavirus DNA load in a population-based cervical screening cohort in relation to the detection of high-grade cervical intraepithelial neoplasia and cervical cancer. Int J Cancer 124(2):381–386. doi:10.1002/ijc.23940
Schmitt M, Depuydt C, Benoy I, Bogers J, Antoine J, Pawlita M, Arbyn M, on behalf of the Vsg (2013) Viral load of high-risk human papillomaviruses as reliable clinical predictor for the presence of cervical lesions. Cancer Epidemiol Biomarkers Prev. doi:10.1158/1055-9965.EPI-12-1067
Schmitt M, Depuydt C, Benoy I, Bogers J, Antoine J, Arbyn M, Pawlita M, on behalf of the Vsg (2013) Multiple HPV infections with high viral loads are associated with cervical lesions but do not differentiate grades of cervical abnormalities. J Clin Microbiol. doi:10.1128/JCM.00087-13
Dondog B, Clifford GM, Vaccarella S, Waterboer T, Unurjargal D, Avirmed D, Enkhtuya S, Kommoss F, Wentzensen N, Snijders PJ, Meijer CJ, Franceschi S, Pawlita M (2008) Human papillomavirus infection in Ulaanbaatar, Mongolia: a population-based study. Cancer Epidemiol Biomark Prev 17(7):1731–1738. doi:10.1158/1055-9965.EPI-07-2796
Halec G, Schmitt M, Dondog B, Sharkhuu E, Wentzensen N, Gheit T, Tommasino M, Kommoss F, Bosch FX, Franceschi S, Clifford G, Gissmann L, Pawlita M (2013) Biological activity of probable/possible high-risk human papillomavirus types in cervical cancer. Int J Cancer 132(1):63–71. doi:10.1002/ijc.27605
Schmitt M, Dondog B, Waterboer T, Pawlita M, Tommasino M, Gheit T (2010) Abundance of multiple high-risk human papillomavirus (HPV) infections found in cervical cells analyzed by use of an ultrasensitive HPV genotyping assay. J Clin Microbiol 48(1):143–149. doi:10.1128/JCM.00991-09
Schmitt M, Bravo IG, Snijders PJ, Gissmann L, Pawlita M, Waterboer T (2006) Bead-based multiplex genotyping of human papillomaviruses. J Clin Microbiol 44(2):504–512. doi:10.1128/JCM.44.2.504-512.2006
Schmitt M, Dondog B, Waterboer T, Pawlita M (2008) Homogeneous amplification of genital human alpha papillomaviruses by PCR using novel broad-spectrum GP5+ and GP6+ primers. J Clin Microbiol 46(3):1050–1059. doi:10.1128/JCM.02227-07
Schmitt M, Depuydt C, Benoy I, Bogers J, Antoine J, Arbyn M, Pawlita M, on behalf of the VSG (2012) Prevalence and viral load of 51 genital human papillomavirus types and three subtypes. Int J Cancer. doi:10.1002/ijc.27891
Halec G, Holzinger D, Schmitt M, Flechtenmacher C, Dyckhoff G, Lloveras B, Hofler D, Bosch FX, Pawlita M (2013) Biological evidence for a causal role of HPV16 in a small fraction of laryngeal squamous cell carcinoma. Br J Cancer 109(1):172–183. doi:10.1038/bjc.2013.296
Cuschieri K, Wentzensen N (2008) Human papillomavirus mRNA and p16 detection as biomarkers for the improved diagnosis of cervical neoplasia. Cancer Epidemiol Biomark Prev 17(10):2536–2545. doi:10.1158/1055-9965.EPI-08-0306
Gnanamony M, Peedicayil A, Subhashini J, Ram TS, Christopher S, Gravitt P, Abraham P (2009) Human papillomavirus types 16 and 18 mRNA levels and not DNA levels may be associated with advancing stages of cervical cancer. Int J Gynecol Cancer 19(8):1415–1420. doi:10.1111/IGC.0b013e3181b62e05
Origoni M, Cristoforoni P, Carminati G, Stefani C, Costa S, Sandri MT, Mariani L, Preti M (2015) E6/E7 mRNA testing for human papilloma virus-induced high-grade cervical intraepithelial disease (CIN2/CIN3): a promising perspective. Ecancermedicalscience 9:533. doi:10.3332/ecancer.2015.533
Josefsson A, Livak K, Gyllensten U (1999) Detection and quantitation of human papillomavirus by using the fluorescent 5’ exonuclease assay. J Clin Microbiol 37(3):490–496
van Duin M, Snijders PJ, Schrijnemakers HF, Voorhorst FJ, Rozendaal L, Nobbenhuis MA, van den Brule AJ, Verheijen RH, Helmerhorst TJ, Meijer CJ (2002) Human papillomavirus 16 load in normal and abnormal cervical scrapes: an indicator of CIN II/III and viral clearance. Int J Cancer 98(4):590–595
Dalstein V, Riethmuller D, Pretet JL, Le Bail Carval K, Sautiere JL, Carbillet JP, Kantelip B, Schaal JP, Mougin C (2003) Persistence and load of high-risk HPV are predictors for development of high-grade cervical lesions: a longitudinal French cohort study. Int J Cancer 106(3):396–403. doi:10.1002/ijc.11222
Moberg M, Gustavsson I, Wilander E, Gyllensten U (2005) High viral loads of human papillomavirus predict risk of invasive cervical carcinoma. Br J Cancer 92(5):891–894. doi:10.1038/sj.bjc.6602436
Moberg M, Gustavsson I, Gyllensten U (2004) Type-specific associations of human papillomavirus load with risk of developing cervical carcinoma in situ. Int J Cancer 112(5):854–859. doi:10.1002/ijc.20480
Castro FA, Koshiol J, Quint W, Wheeler CM, Gillison ML, Vaughan LM, Kleter B, van Doorn LJ, Chaturvedi AK, Hildesheim A, Schiffman M, Wang SS, Zuna RE, Walker JL, Dunn ST, Wentzensen N (2015) Detection of HPV DNA in paraffin-embedded cervical samples: a comparison of four genotyping methods. BMC Infect Dis 15:544. doi:10.1186/s12879-015-1281-5
De Vuyst H, Chung MH, Baussano I, Mugo NR, Tenet V, van Kemenade FJ, Rana FS, Sakr SR, Meijer CJ, Snijders PJ, Franceschi S (2013) Comparison of HPV DNA testing in cervical exfoliated cells and tissue biopsies among HIV-positive women in Kenya. Int J Cancer 133(6):1441–1446. doi:10.1002/ijc.28131
Dona MG, Ronchetti L, Giuliani M, Carosi M, Rollo F, Congiu M, Mazza D, Pescarmona E, Vocaturo A, Benevolo M (2013) Performance of the linear array HPV genotyping test on paired cytological and formalin-fixed, paraffin-embedded cervical samples. J Mol Diagn 15(3):373–379. doi:10.1016/j.jmoldx.2013.01.002
Jancar N, Kocjan BJ, Poljak M, Bokal EV (2009) Comparison of paired cervical scrape and tumor tissue samples for detection of human papillomaviruses in patients with cervical cancer. Eur J Gynaecol Oncol 30(6):675–678
Gravitt PE, van Doorn LJ, Quint W, Schiffman M, Hildesheim A, Glass AG, Rush BB, Hellman J, Sherman ME, Burk RD, Wang SS (2007) Human papillomavirus (HPV) genotyping using paired exfoliated cervicovaginal cells and paraffin-embedded tissues to highlight difficulties in attributing HPV types to specific lesions. J Clin Microbiol 45(10):3245–3250. doi:10.1128/JCM.00216-07
Broccolo F, Fusetti L, Rosini S, Caraceni D, Zappacosta R, Ciccocioppo L, Matteoli B, Halfon P, Malnati MS, Ceccherini-Nelli L (2013) Comparison of oncogenic HPV type-specific viral DNA load and E6/E7 mRNA detection in cervical samples: results from a multicenter study. J Med Virol 85(3):472–482. doi:10.1002/jmv.23487
Briolat J, Dalstein V, Saunier M, Joseph K, Caudroy S, Pretet JL, Birembaut P, Clavel C (2007) HPV prevalence, viral load and physical state of HPV-16 in cervical smears of patients with different grades of CIN. Int J Cancer 121(10):2198–2204. doi:10.1002/ijc.22959
Depuydt CE, Jonckheere J, Berth M, Salembier GM, Vereecken AJ, Bogers JJ (2015) Serial type-specific human papillomavirus (HPV) load measurement allows differentiation between regressing cervical lesions and serial virion productive transient infections. Cancer Med 4(8):1294–1302. doi:10.1002/cam4.473
Clifford GM, Vaccarella S, Franceschi S, Tenet V, Umulisa MC, Tshomo U, Dondog B, Vorsters A, Tommasino M, Heideman DA, Snijders PJ, Gheit T (2016) Comparison of two widely used human papillomavirus detection and genotyping methods, GP5+/6+-based PCR followed by reverse line blot hybridization and multiplex type-specific E7-based PCR. J Clin Microbiol 54(8):2031–2038. doi:10.1128/JCM.00618-16
Herbert A (2016) Re: HPV testing alone is not as safe as cytology and selective HPV testing. BJOG 123(9):1561–1562. doi:10.1111/1471-0528.14061
Pedersen K, Sorbye SW, Kristiansen IS, Burger EA (2016) Using novel biomarkers to triage young adult women with minor cervical lesions: a cost-effectiveness analysis. BJOG. doi:10.1111/1471-0528.14135
Acknowledgements
We thank Prof. Otoniel Martinez-Maza for his support during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Authors GH, BD, MS, and MP designed and/or performed experiments, analyzed the data, contributed reagents/materials/analysis tools, and wrote the paper.
Corresponding author
Ethics declarations
Disclosure of interests
MP and MS have received research support through cooperation contracts of DKFZ with Roche and Qiagen in the field of development of HPV diagnostics. They are inventors on patents owned by DKFZ in the field of HPV diagnostics. Authors GH and BD have no conflict.
Details of ethics approval
Ethics approvals were obtained as described in detail in Dondog et al., CEPB, 2008, PMID: 23034864. In short: On arrival at the study clinic, all participants read and signed an informed consent form explaining the main research goals, sample collection procedures, potential benefits and harms, and confidentiality of data collected for the study. The informed consent form respected the recommendations of the ethical review committees of the IARC and the Mongolian Health Ministry, which both approved the study.
Funding
Research grants from the Qiagen and Roche were awarded to Drs. Schmitt and Pawlita in the field of HPV diagnostics. These agencies were not involved in data analysis or interpretation.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Halec, G., Dondog, B., Pawlita, M. et al. Concordance of HPV load and HPV mRNA for 16 carcinogenic/possibly carcinogenic HPV types in paired smear/tissue cervical cancer specimens. Arch Virol 162, 3313–3327 (2017). https://doi.org/10.1007/s00705-017-3452-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-017-3452-8