Abstract
Background and objectives
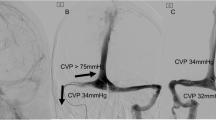
Internal jugular vein (IJV) stenosis is associated with several neurological disorders including idiopathic intracranial hypertension (IIH) and pulsatile tinnitus. In cases of extreme bony compression causing stenosis in the infracondylar region, surgical decompression might be necessary. We aim to examine the safety and efficacy of surgical IJV decompression.
Methods
We retrospectively reviewed patients who received surgical IJV decompression via the extreme lateral infracondylar (ELI) approach between July 2020 and February 2022.
Results
Fourteen patients with IJV stenosis were identified, all with persistent headache and/or tinnitus. Six patients were diagnosed with IIH, three of whom failed previous treatment. Of the eight remaining patients, two failed previous treatment. All underwent surgical IJV decompression via styloidectomy, release of soft tissue, and removal of the C1 transverse process (TP). Follow-up imaging showed significant improvement of IJV stenosis in eleven patients and mild improvement in three. Eight patients had significant improvement in their presenting symptoms, and three had partial improvement. Two patients received IJV stenting after a lack of initial improvement. Two patients experienced cranial nerve paresis, and one developed a superficial wound infection.
Conclusion
The ELI approach for IJV decompression appears to be safe for patients who are not ideal endovascular candidates due to bony anatomy. Confirming long-term efficacy in relieving debilitating clinical symptoms requires longer follow-up and a larger patient cohort. Carefully selected patients with symptomatic bony IJV compression for whom there are no effective medical or endovascular options may benefit from surgical IJV decompression.



Similar content being viewed by others
Data Availability
Data is available by request to the corresponding author.
Abbreviations
- CTV:
-
Computed tomography venogram
- DSA:
-
Digital subtraction venography
- ELI:
-
Extreme lateral infracondylar
- IIH:
-
Idiopathic intracranial hypertension
- IJV:
-
Internal jugular vein
- MRI:
-
Magnetic resonance imaging
- TP:
-
Transverse process
References
Bai C, Wang Z, Guan J, Jin K, Ding Y, Ji X et al (2020) Clinical characteristics and neuroimaging findings in eagle syndrome induced internal jugular vein stenosis. Ann Trans Med 8(4):97. https://doi.org/10.21037/atm.2019.12.93
Bateman GA (2008) Arterial inflow and venous outflow in idiopathic intracranial hypertension associated with venous outflow stenoses. J Clin Neurosci 15(4):402–408. https://doi.org/10.1016/j.jocn.2007.03.018
Ceylan A, Köybasioglu A, Celenk F, Yilmaz O, Uslu S (2008) Surgical treatment of elongated styloid process: experience of 61 cases. Skull Base 18(5):289–95. https://doi.org/10.1055/s-0028-1086057
Chung C-P, Beggs C, Wang P-N, Bergsland N, Shepherd S, Cheng C-Y et al (2014) Jugular venous reflux and white matter abnormalities in Alzheimer’s disease: a pilot study. J Alzheimer’s Dis 39(3):601–609. https://doi.org/10.3233/jad-131112
Chung C-P, Hsu H-Y, Chao A-C, Sheng W-Y, Soong B-W, Hu H-H (2007) Transient global amnesia: cerebral venous outflow impairment-insight from the abnormal flow patterns of the internal jugular vein. Ultrasound Med Biol 33(11):1727–1735. https://doi.org/10.1016/j.ultrasmedbio.2007.05.018
Dashti SR, Nakaji P, Hu YC, Frei DF, Abla AA, Yao T et al (2012) Styloidogenic jugular venous compression syndrome: diagnosis and treatment: case report. Neurosurgery 70(3):E795–E799. https://doi.org/10.1227/NEU.0b013e3182333859
Ding J-Y, Zhou D, Pan L-Q, Ya J-Y, Liu C, Yan F et al (2020) Cervical spondylotic internal jugular venous compression syndrome. CNS Neurosci Ther 26(1):47–54. https://doi.org/10.1111/cns.13148
Fritch C, Voronovich Z, Carlson AP (2020) C1 transverse process resection for management of jugular stenosis. Oper Neurosurg (Hagerstown) 19(2):E209–E213. https://doi.org/10.1093/ons/opaa032
Higgins JN, Garnett MR, Pickard JD, Axon PR (2017) An evaluation of styloidectomy as an adjunct or alternative to jugular stenting in idiopathic intracranial hypertension and disturbances of cranial venous outflow. J Neurol Surg B Skull Base 78(2):158–163. https://doi.org/10.1055/s-0036-1594238
Hsu H-Y, Chao A-C, Chen Y-Y, Yang F-Y, Chung C-P, Sheng W-Y et al (2008) Reflux of jugular and retrobulbar venous flow in transient monocular blindness. Ann Neurol 63(2):247–538. https://doi.org/10.1002/ana.21299
Jayaraman MV, Boxerman JL, Davis LM, Haas RA, Rogg JM (2012) Incidence of extrinsic compression of the internal jugular vein in unselected patients undergoing CT angiography. AJNR Am J Neuroradiol 33(7):1247–50. https://doi.org/10.3174/ajnr.A2953
Karahalios DG, Rekate HIL, Khayata MH, Apostolides PJ (1996) Elevated intracranial venous pressure as a universal mechanism in pseudotumor cerebri of varying etiologies. Neurology 46(1):198–202. https://doi.org/10.1212/wnl.46.1.198
Kharkar S, Hernandez R, Batra S, Metellus P, Hillis A, Williams MA, Rigamonti D (2011) Cognitive impairment in patients with pseudotumor cerebri syndrome. Behav Neurol 24(2):143–8. https://doi.org/10.3233/BEN-2011-0325
King JO, Mitchell PJ, Thomson KR, Tress BM (1995) Cerebral venography and manometry in idiopathic intracranial hypertension. Neurology 45(12):2224–2228. https://doi.org/10.1212/wnl.45.12.2224
Lenck S, Radovanovic I, Nicholson P, Hodaie M, Krings T, Mendes-Pereira V (2018) Idiopathic intracranial hypertension: the veno glymphatic connections. Neurology 91(11):515–522. https://doi.org/10.1212/WNL.0000000000006166
Li M, Gao X, Rajah GB, Liang J, Chen J, Yan F, Bao Y, Jiao L, Zhang H, Ding Y, Ji X, Meng R (2019) Styloidectomy and venous stenting for treatment of styloid-induced internal jugular vein stenosis: a case report and literature review. World Neurosurg 129–32. https://doi.org/10.1016/j.wneu.2019.06.100
Li M, Sun Y, Chan CC, Fan C, Ji X, Meng R (2019) Internal jugular vein stenosis associated with elongated styloid process: five case reports and literature review. BMC Neurol 19(1):112. https://doi.org/10.1186/s12883-019-1344-0
Li M, Sun Y, Chan CC, Fan C, Ji X, Meng R (2019) Internal jugular vein stenosis associated with elongated styloid process: five case reports and literature review. BMC Neurol 19(1):112. https://doi.org/10.1186/s12883-019-1344-0
Mejia-Vergara AJ, Sultan W, Kostas A, Mulholland CB, Sadun A (2021) Styloidogenic jugular venous compression syndrome with papilloedema: case report and review of the literature. Neuroophthalmology 46(1):54–8. https://doi.org/10.1080/01658107.2021.1887288
Mooney J, Lepard J, Akbari SHA, Johnston JM (2020) Styloidogenic jugular venous compression syndrome: a case report and review of the literature. Childs Nerv Syst 36(12):3135–9. https://doi.org/10.1007/s00381-020-04622-6
Nedelmann M, Kaps M, Mueller-Forell W (2009) Venous obstruction and jugular valve insufficiency in idiopathic intracranial hypertension. J Neurol 256(6):964–969. https://doi.org/10.1007/s00415-009-5056-z
Primiani CT, Lawton M, Hillis AE, Hui FK (2022) Pearls & Oy-sters: Cerebral venous congestion associated with cognitive decline treated by jugular release. Neurology 99(13):577–580. https://doi.org/10.1212/WNL.0000000000201037
Sattur MG, Amans M, Fargen KM, Huisman TAGM, Brinjikji W, Hui F, Shingala A, Vosler PS, Pereira VM, Hepworth E, Dehdashti AR, Patsalides A, Lo SL, Spiotta AM (2023) Angiographic evaluation of cranial venous outflow patterns in patients with and without idiopathic intracranial hypertension. Oper Neurosurg (Hagerstown) 24(1):e29–e35. https://doi.org/10.1227/ons.0000000000000413
Scerrati A, Norri N, Mongardi L, Dones F, Ricciardi L, Trevisi G et al (2021) Styloidogenic- cervical spondylotic internal jugular venous compression, a vascular disease related to several clinical neurological manifestations: diagnosis and treatment-a comprehensive literature review. Ann Trans Med. 9(8):718. https://doi.org/10.21037/atm-20-7698
Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 147(8):573–577
Yri HM, Fagerlund B, Forchhammer HB, Jensen RH (2014) Cognitive function in idiopathic intracranial hypertension: a prospective case-control study. BMJ Open 4(4):e004376. https://doi.org/10.1136/bmjopen-2013-004376
Zamboni P, Scerrati A, Menegatti E, Galeotti R, Lapparelli M, Traina L et al (2019) The eagle jugular syndrome. BMC Neurol 19(1):333. https://doi.org/10.1186/s12883-019-1572-3
Zhao X, Cavallo C, Hlubek RJ, Mooney MA, Belykh E, Gandhi S, Moreira LB, Lei T, Albuquerque FC, Preul MC, Nakaji P (2019) Styloidogenic jugular venous compression syndrome: clinical features and case series. Oper Neurosurg (Hagerstown) 17(6):554–561. https://doi.org/10.1093/ons/opz012
Zhou D, Ding J, Asmaro K, Pan L, Ya J, Yang Q et al (2019) Clinical characteristics and neuroimaging findings in internal jugular venous outflow disturbance. Thromb Haemost 119(2):308–318. https://doi.org/10.1055/s-0038-1676815
Zhou D, Ding J-Y, Ya J-Y, Pan L-Q, Yan F, Yang Q et al (2018) Understanding jugular venous outflow disturbance. CNS Neurosci Ther 24(6):473–82. https://doi.org/10.1111/cns.12859
Zhou D, Meng R, Zhang X, Guo L, Li S, Wu W et al (2018) Intracranial hypertension induced by internal jugular vein stenosis can be resolved by stenting. Eur J Neurol 25:365-e13. https://doi.org/10.1111/ene.13512
Zhou D, Meng R, Zhang X, Guo L, Li S, Wu W, Duan J, Song H, Ding Y, Ji X (2018) Intracranial hypertension induced by internal jugular vein stenosis can be resolved by stenting. Eur J Neurol 25(2):365-e13. https://doi.org/10.1111/ene.13512
Zivadinov R, Chung C-P (2013) Potential involvement of the extracranial venous system in central nervous system disorders and aging. BMC Med 11:260. https://doi.org/10.1186/1741-7015-11-260
Acknowledgements
We would like to thank Ms. Elyssa Siegel for her assistance with the illustrations in Figure 2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was conducted retrospectively from data obtained for clinical purposes and approved by the IRB.
Informed consent
IRB approval included a waiver of patient consent.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 507491 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, K., Shah, K., Begley, S.L. et al. Extreme lateral infracondylar approach for internal jugular vein compression syndrome: A case series with preliminary clinical outcomes. Acta Neurochir 165, 3445–3454 (2023). https://doi.org/10.1007/s00701-023-05779-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05779-0