Abstract
Background
Laser interstitial thermal therapy (LITT) has been used to treat brain metastases (BMs) in several countries, and its safety and effectiveness have been confirmed. In most cases, magnetic resonance imaging (MRI) reveals an increase in tumor volume with an enhanced margin after LITT. However, little is known about the relationship between this MRI change and tumor recurrence.
Objective
We report the first case series of BMs treated by LITT in China to evaluate the clinical characteristics and predictive factors of tumor recurrence.
Material and methods
Patients with less than four brain metastatic lesions and a Karnofsky performance status (KPS) > 70 were eligible for study inclusion. Standard LITT procedures were performed, and a follow-up MRI was performed to analyze the radiographic changes, especially the volume ratio of the enhanced margin and the whole lesion on MRI at 30 days postoperatively. All the volume-related data were delineated and calculated using 3D Slicer software. Related predictors were also collected to evaluate the correlation with local tumor control.
Results
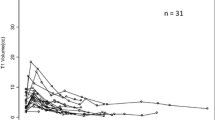
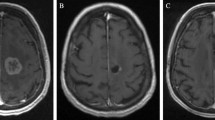
Eighteen patients with nineteen lesions were enrolled for treatment and follow-up. Primary tumor histology included pulmonary carcinoma (n = 11) and breast cancer (n = 4). On average, the tumor size measured 3.01 cm3 (range, 0.40–7.40 cm3), the total ablation time was 13.58 min (range, 2.88–37.15 min), and the complete ablation rate was 92.4% (range, 29.2–100%). Comparing 3s0-day follow-up MRI results with preoperative MRI findings, 18 lesions showed a 2.28-fold (range, 1.21–4.88) volume increase; all the lesions displayed an enhanced component with a volume ratio of 42.35% (range, 10.14–100%). Five patients experienced tumor recurrence, and the local tumor control rates at 90 days and 180 days of follow-up were 68.4% and 66.7%, respectively. Univariate analysis indicated that the primary tumor, ablation rate, and enhanced volume ratio (EVR) > 40% in the 30-day MRI were associated with tumor recurrence, whereas multivariate analysis showed that only EVR > 40% was a predictive factor of local control.
Conclusion
LITT is a minimally invasive method used to ablate brain metastases which can be used as the first-line treatment for BM patients under certain indications. After LITT, most tumors showed volume enlargement on the 30-day MRI scan, and EVR > 40% on the 30-day MRI may indicate late tumor recurrence.





Similar content being viewed by others
Data Availability
The datasets generated and/or analysed during the current study are not publicly available because it is used for further analysis, but are available from the corresponding author on reasonable request.
Abbreviations
- BM:
-
Brain metastases
- LITT:
-
Laser interstitial thermal therapy
- SRS:
-
Stereotactic radiosurgery
- MRI:
-
Magnetic resonance imaging
- KPS:
-
Karnofsky performance status
- CSF:
-
Cerebrospinal fluid
- EVR:
-
Enhanced volume ratio
References
Ahluwalia M, Barnett GH, Deng D et al (2018) Laser ablation after stereotactic radiosurgery: a multicenter prospective study in patients with metastatic brain tumors and radiation necrosis. J Neurosurg 130(3):804–811. https://doi.org/10.3171/2017.11.JNS171273
Beechar VB, Prabhu SS, Bastos D et al (2018) Volumetric response of progressing post-SRS lesions treated with laser interstitial thermal therapy. J Neurooncol 137(1):57–65
Bown SG (1983) Phototherapy of tumors. World J Surg 7(6):700–709. https://doi.org/10.1007/BF01655209
Carpentier A, McNichols RJ, Stafford RJ, Itzcovitz J, Guichard JP, Reizine D et al (2008) Real-time magnetic resonance-guided laser thermal therapy for focal metastatic brain tumors. Neurosurg 21(5):818–825. https://doi.org/10.1227/01.neu.0000335007.07381
Carpentier A, McNichols RJ, Stafford RJ et al (2011) Laser thermal therapy: real-time MRI-guided and computer-controlled procedures for metastatic brain tumors. Lasers Surg Med 43(10):943–950
de Bastos DCA, Rao G, Oliva ICG et al (2020) Predictors of local control of brain metastasis treated with laser interstitial thermal therapy. Neurosurg 87(1):112–122
Durnea CM, Siddiqi S, Nazarian D, Munneke G, Sedgwick PM, Doumouchtsis SK (2021) 3D-volume rendering of the pelvis with emphasis on paraurethral structures based on MRI scans and comparisons between 3D Slicer and OsiriX®. J Med Syst 45(3):27. https://doi.org/10.1007/s10916-020-01695-3
Egger J, Kapur T, Nimsky C, Kikinis R (2012) Pituitary adenoma volumetry with 3D Slicer. PLoS One 7(12):e51788. https://doi.org/10.1371/journal.pone.0051788
Egger J, Kapur T, Fedorov A, Pieper S, Miller JV, Veeraraghavan H et al (2013) GBM volumetry using the 3D Slicer medical image computing platform. Sci Rep 3:1364. https://doi.org/10.1038/srep01364
Elder JB, Huntoon K, Otero J, Kaya B, Hatel J, Eltobgy M et al (2019) Histological findings associated with laser interstitial thermotherapy for glioblastoma multiforme. Diagn Pathol 14(1):19. https://doi.org/10.1186/s13000-019-0794-4
Hernandez RN, Carminucci A, Patel P, Hargreaves EL, Danish SF (2019) Magnetic resonanceguided laser-induced thermal therapy for the treatment of progressive enhancing inflammatory reactions following stereotactic radiosurgery, or PEIRs, for metastatic brain disease. Neurosurg 85(1):84–90. https://doi.org/10.1093/neuros/nyy220
Jethwa PR, Barrese JC, Gowda A, Shetty A, Danish SF (2012) Magnetic resonance thermometry-guided laser-induced thermal therapy for intracranial neoplasms: initial experience. Neurosurg 71(1 suppl operative):133–144
Jolesz FA, Bleier AR, Jakab P, Ruenzel PW, Huttl K, Jako GJ (1988) MR imaging of laser-tissue interactions. Radiol 168(1):249–253
Kahn T, Bettag M, Ulrich F, Schwarzmaier HJ, Schober R, Fürst G et al (1994) MRI-guided laser-induced interstitial thermotherapy of cerebral neoplasms. J Comput Assist Tomogr 18(4):519–532
Kim AH, Tatter S, Rao G et al (2020) Laser Ablation of Abnormal Neurological Tissue Using Robotic NeuroBlate System (LAANTERN): 12-month outcomes and quality of life after brain tumor ablation. Neurosurg 87(3):E338–E346. https://doi.org/10.1093/neuros/nyaa071
Lacroix M, Abi-Said D, Fourney DR et al (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95(2):190–198. https://doi.org/10.3171/jns.2001.95.2.0190
Leuthardt EC, Voigt J, Kim AH, Sylvester P (2017) A single-center cost analysis of treating primary and metastatic brain cancers with either brain laser interstitial thermal therapy (LITT) or craniotomy. PharmacoEconomics Open 1(1):53–63. https://doi.org/10.1007/s41669-016-0003-2
Menovsky T, Beek JF, van Gemert MJ, Roux FX, Bown SG (1996) Interstitial laser thermotherapy in neurosurgery: a review. Acta Neurochir 138(9):1019–1026
Patel B, Yang PH, Kim AH (2020) The effect of thermal therapy on the blood-brain barrier and blood-tumor barrier. Int J Hyperthermia 37(2):35–43. https://doi.org/10.1080/02656736.2020.1783461
Rao MS, Hargreaves EL, Khan AJ, Haffty BG, Danish SF (2014) Magnetic resonance-guided laser ablation improves local control for postradiosurgery recurrence and/or radiation necrosis. Neurosurg 74(6):658–667. https://doi.org/10.1227/NEU.0000000000000332
Salehi A, Kamath AA, Leuthardt EC, Kim AH (2018) Management of intracranial metastatic disease with laser interstitial thermal therapy. Front Oncol 8:499. https://doi.org/10.3389/fonc.2018.00499
Schwabe B, Kahn T, Harth T, Ulrich F, Schwarzmaier HJ (1997) Laser-induced thermal lesions in the human brain: short- and long-term appearance on MRI. J Comput Assist Tomogr 21(5):818–825
Sugiyama K, Sakai T, Fujishima I, Ryu H, Uemura K, Yokoyama T (1990) Stereotactic interstitial laser hyperthermia using Nd-YAG laser. Stereotact Funct Neurosurg 54–55:501–505
Sutton CH (1971) Tumor hyperthermia in the treatment of malignant gliomas of the brain. Trans Am Neurol Assoc 96:195–199
Tabouret E, Chinot O, Metellus P, Tallet A, Viens P, Gonçalves A (2012) Recent trends in epidemiology of brain metastases: an overview. Anticancer Res 32(11):4655–4662
Acknowledgements
This study was supported by grants from the National Natural Science Foundation of China (82003075), Beijing Tiantan Hospital Independent Program (HX-A-2022029), and Beijing Hospitals Authority Youth Program (QML20210502).
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Beijing Tiantan Hospital (No. QX2020-018–02). Written informed consent was obtained from each patient (or the legal guardian of pediatric patients) before study enrollment.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Brain Tumors
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xue, Z., Guan, X., Yuan, L. et al. Laser interstitial thermal therapy in the treatment of brain metastases: the relationship between changes in postoperative magnetic resonance imaging characteristics and tumor recurrence. Acta Neurochir 165, 1379–1387 (2023). https://doi.org/10.1007/s00701-023-05504-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05504-x