Abstract
Background
The Glasgow Coma Scale (GCS) is considered the gold standard for assessment of unconsciousness in patients with traumatic brain injury (TBI) against which other scales are compared. To overcome the disadvantages of GCS, the Full Outline Of Unresponsiveness (FOUR) score was proposed. We aimed to compare the predictability of FOUR score and GCS for early mortality, after moderate and severe TBI.
Methods
This is a prospective observational study of patients with moderate and severe TBI. Both FOUR and GCS scores were determined at admission. The primary outcome was mortality at the end of 2 weeks of injury.
Results
A total of 138 (117 males) patients were included in the study. Out of these, 17 (12.3 %) patients died within 2 weeks of injury. The mean GCS and FOUR scores were 9.5 (range, 3–13) and 11 (0–16), respectively. The total GCS and FOUR scores were significantly lower in patients who did not survive. At a cut-off score of 7 for FOUR score, the AUC was 0.97, with sensitivity of 97.5 and specificity of 88.2 % (p < 0.0001). For GCS score, AUC was 0.95, with sensitivity of 98.3 % and specificity of 82.4 % with cut-off score of 6 (p < 0.0001). The correlation coefficient was 0.753 (p < 0.001) between the GCS and FOUR scores.
Conclusions
The predictive value of the FOUR score on admission of patients with TBI is no better than the GCS score.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic brain injury (TBI) is a major cause of death and disability worldwide. To assess the level of consciousness after TBI, Teasdale and Jennett in 1974 described a coma scale known as the Glasgow Coma Scale (GCS) [15]. It incorporates three components: eye, verbal, and motor responses with a maximum of four, five, and six points; and a minimum of one point in each category, respectively. The GCS is a simple, objective, easy-to-follow scale that is widely accepted to assess the severity of TBI, and is considered the gold standard against which other coma scales are compared. TBI is classified as mild, moderate, or severe, depending on the GCS. In TBI, GCS has frequently been used to predict outcome after head injury. Studies have been done to evaluate the predictive ability of GCS after head injury. Bishara et al. reported a statistically significant relationship between admission GCS and outcome as measured by the Glasgow Outcome Scale (GOS) at 6 months and 12-months post-injury (r = 0.45, p < 0.001) [3]. Similarly, Poon et al. reported 71 % accuracy of GCS using outcome categories of moderate/severe disability and good recovery [10]. However, GCS differentiates poorly between patients with low GCS, and also in intubated patients. Also, there are certain drawbacks of the GCS system such as skewness towards motor score, an inability to assess verbal score in intubated and aphasic patients, and a lack of brainstem reflexes.
In order to overcome the disadvantages of GCS, Widjicks et al. published the Full Outline Of Unresponsiveness (FOUR) score in 2005 [16]. It provides additional information about brainstem function and respiratory drive. The FOUR score is useful even in intubated patients as verbal response is not a component of FOUR score. The four components of FOUR score are: eye tracking, motor response, brainstem function, and respiratory drive. Each category is given 0–4 points, 0 being the worst and 4 being the best. The FOUR score has been found to be superior in the assessment of comatose patients [14].
There is a paucity of literature comparing FOUR score and GCS for prediction of outcome in TBI. In a recently published study by Mc Nett et al., the authors found that the FOUR score is comparable to GCS in terms of predictive ability for functional status, cognitive outcome at 3 months post-injury, and in-hospital mortality [7]. In a similar study by Sadaka et al., the authors found that FOUR score was an accurate predictor of in-hospital mortality, and neurologic outcome. However, in their study, the majority of patients had mild head injuries [11]. We aimed to compare the predictability of FOUR score and GCS for early mortality after moderate and severe TBI.
Materials and methods
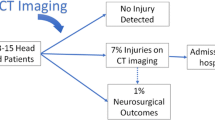
This is a prospective observational study. An approval from the institute’s ethics committee was obtained (Item No. XII, Sl. No. 12.20, Clinical Neurosciences). The study population included consecutive patients with moderate and severe TBI admitted to the emergency department of our hospital over a period of 3 months. The patients were managed as per the standard hospital protocol and CT scans were done as indicated. The patients underwent surgical or medical treatment as required. Both FOUR and GCS scores were determined by the same rater (AS) at admission. The patients were followed up until 2 weeks after injury to look for mortality. The 2-week time period was chosen based on a prognostic calculator proposed by CRASH collaborators [8]. The primary outcome of our study was mortality at the end of 2 weeks. A total of 138 patients were recruited in the study.
Statistical analysis
The predictive value of the GCS and FOUR scores in predicting mortality was established using the receiver operating characteristic (ROC) curve by calculating area under the curve (AUC). Mann–Whitney test was used to compare the two scores between survivors and non-survivors. Spearman’s rank correlation was used to determine the correlation between GCS and FOUR scores. The power of the study was >90 %.
Results
A total of 138 (117 males) patients were included in the study. Out of these, 17 (12.3 %) patients died within 2 weeks of admission to the hospital. The mean age of patients was 38 years (SD 15.5). The Marshal CT scan grading was I, II, III, IV, V, and VI in 7, 78, 13, 5, 28, and 7 patients, respectively. The mean GCS and FOUR scores for the entire patient cohort were 9.5 (SD 2.4) and 11 (SD 3), respectively (Table 1). The total FOUR and GCS scores were higher in patients who survived than those who did not. The mean FOUR scores were 12 and 4.9 in survivors and non-survivors, respectively (p value < 0.001). The mean GCS scores were 10 and 4.7 in survivors and non-survivors respectively (p value < 0.001). The score for the individual components of both GCS and FOUR were also lower in patients who did not survive (Tables 2 and 3). When using a cut-off score of 7 for FOUR score, the AUC was 0.97 with sensitivity of 97.5 % and specificity of 88.2 % (p < 0.0001). Similarly, with a cut-off score of 6 for the GCS score, AUC was 0.95 with sensitivity of 98.3 % and specificity of 82.4 % (p < 0.0001) (Fig. 1). When using the same cut-off of 7 for FOUR score, 76.5 % of patients who did not survive had FOUR score <7, while all the survivors had FOUR score ≥ 7. Similarly for GCS, 76.5 % of non-survivors had GCS < 6, and all the survivors had GCS ≥ 6 (Pearson’s Chi-square value <0.001). Spearman’s correlation showed a correlation coefficient of 0.758 between GCS and FOUR score with p value of < 0.001 (Fig. 2). This indicates a good-to-very good correlation between the two scores. When analyzing FOUR score in seven patients who had GCS of 3, FOUR scores were 2 in three patients, 3 in one patient, and 4 in three patients, and none of them survived. Similarly, amongst nine patients who had FOUR score <5, all except two patients had GCS 3 (one each had GCS 4 and 5), and none survived. This indicates that at the lowest scores the correlation between FOUR and GCS scores is nearly perfect in predicting mortality. Logistic regression analysis was used to determine which components of the score can be used to predict early mortality after adjusting for age. The results showed that although the FOUR score in total can be used to predict mortality, individually, none of the components were significantly associated with mortality. When applied to GCS, GCS as a whole and its motor component independently were significantly associated with mortality (Table 4).
Discussion
Accurate assessment of the level of unconsciousness is essential for improving communication among health care professionals and for prognosticating outcomes. The most commonly used scale for this purpose in patients with head injury is the Glasgow Coma Scale. The GCS has been used to predict mortality in a number of studies. In a large study of 46,977 head-injured patients, the authors investigated the relationship between GCS and mortality [5]. The results showed a sharp progressive increase in mortality in patients who presented to the emergency room with a GCS score of 3–8. Irrespective of pathology, GCS is a significant predictor of mortality. Even in the Acute Physiology and Chronic Health Evaluation (APACHE) III scoring system for use in general intensive care unit (ICU), the GCS has been found to be more predictive of the outcome than any other single variable [1].
There are certain shortcomings with the use of GCS, which may explain the encountered discrepancies with prognostication using GCS. In intubated patients, the verbal component cannot be assessed. GCS may not detect subtle changes in neurological status and it is difficult to interpret intermediate GCS scores. Any change in respiratory pattern or brainstem reflexes, which reflect the severity of coma, are not accounted for in the calculation of GCS. Moreover, there is skewness towards motor score [2]. In order to overcome the disadvantages of GCS, Widjicks et al. published the Full Outline Of Unresponsiveness (FOUR) score in 2005 [16]. It provides additional information about brainstem function and respiratory drive. The FOUR score is useful even in intubated patients as verbal response is not a component of FOUR score. Since all the components of FOUR score are given equal weightage, the score is linear and may make it a more reliable. The FOUR score has been validated in the evaluation of comatose patients [14]. Both scores are also used as clinical monitoring tool and the added value of the FOUR score is probably in more severe patients in the ICU environment over time.
The FOUR and GCS scores have been compared for assessment of coma due to various causes. Stead et al. found that the inter-reliability of FOUR score and GCS was excellent (Kw = 0.88 and 0.86, respectively). Both predicted the functional outcome and overall survival with and without adjustment for age, sex, and alertness [14]. In a study by Chen et al., the authors found that the predictive value of the FOUR score for 30-day mortality was slightly higher than GCS; however for prediction of poor outcome and favorable outcome after 30 days, both scales showed similar performance. The patient population included mainly TBI, non-traumatic intracerebral hemorrhage, and aneurysmal subarachnoid hemorrhage [4]. There are only four studies comparing FOUR and GCS scores for prediction of outcome exclusively in patients with TBI. In a study by McNett et al. comprising 136 patients admitted to the ICU, the authors compared FOUR and GCS scores at 24 and 72 h for functional and cognitive outcomes, and also compared the scores at same time points with mortality [7]. The FOUR score was found comparable to GCS in terms of predictive ability for functional status, cognitive outcome at 3 months post-injury, and in-hospital mortality [7]. The AUCs for FOUR and GCS scores for predicting mortality were 0.913 and 0.935, respectively. However, the AUCs for other outcome measures were lower. In another study by Sadaka et al. comprising 51 patients admitted to the ICU, the authors found that FOUR and GCS scores were comparable for predicting in-hospital mortality and when outcome was compared using the Glasgow Outcome Scale (GOS) and the modified Rankin scale (mRS) [11]. The AUCs for FOUR and GCS scores for predicting mortality were 0.93 and 0.89. The AUCs for functional outcome measures were relatively low. In the same study, the odds ratio (OR) for in-hospital mortality was 0.64 (0.46–0.88) for FOUR score and 0.63 (0.45–0.89) for GCS. In another study by Jalali et al., 88 patients with TBI (after excluding heavily sedated patients) were recruited from the intensive care unit. Patients were followed up for 2 weeks or hospital discharge to determine mortality. They found that the FOUR score had a better prediction of death than GCS in terms of specificity positive predictive value, negative predictive value, and accuracy [6]. In another study by Okasha et al., 60 patients with TBI were enrolled in the study. The GCS and FOUR score were documented on arrival to the emergency room. The FOUR score showed significantly higher AUC than the GCS score (0.850 vs. 0.796, p = 0.025). The FOUR score and the GCS score were not different in predicting unfavorable outcome (AUC 0.813 vs. 0.779, p = 0.136) and endotracheal intubation (AUC 0.961 vs. 0.982, p = 0.06). Both scores were good at predicting length of stay in an ICU [9]. In a recent multi-institutional study of unselected critically ill patients, the authors compared predictability of FOUR and GCS scores [17]. They found that the AUC for FOUR score was 0.742, whereas GCS was 0.715. The difference was significant. The authors concluded that the FOUR score might be a better prognostic tool of ICU mortality. However, in their patient population, only 19.7 % had neurological illness [17]. The number of patients with TBI is not mentioned. As GCS is primarily intended for patients with TBI, it was not surprising that it performed poorly in this study comprising a large proportion of non-TBI patients. These studies concluded that the FOUR score and GCS performed equally well, but the neurologic detail incorporated in the FOUR score makes it more useful for evaluating patients.
These studies included only patients admitted to an ICU. In the present study, we have taken the admission scores, as evaluation at the time of admission has prognostic importance. We did not include mild TBI (mTBI) cases as mortality after mTBI is very low [13]. Moreover, mortality is not the appropriate outcome measure for mTBI [12]. We also found FOUR and GCS scores to be comparable for prediction of mortality, in terms of AUC, sensitivity, and specificity. Though there are many similarities between the FOUR score motor response and the GCS motor response, the FOUR score motor response was not significant, whilst the GCS motor response was significant. This is due to a lack of abnormal flexion or withdrawal response category in the FOUR score. Other reasons are that the number of motor responses in FOUR score is five, whilst in GCS it is six. There was also good to very good correlation between the FOUR and GCS scores. Our findings confer with other studies.
Limitations of the study
Ours is a single-center study, however this also ensured that other factors such as level of care and management strategy would be similar for all the study subjects. The FOUR score and GCS were assessed by the same investigator, so we cannot comment about inter-rater reliability. As the inter-rater reliability of FOUR and GCS scores is established, we did not feel it necessary to repeat it for our study. As we took early mortality as an outcome measure, hence the predictive ability of these scores for functional outcome cannot be commented upon. If these scores are utilized for continuous care, then other outcome tools like GOS or outcomes of disability are required for comparing the utility of these scores. We did not adjust for other predictors of mortality, like CT scan findings, hypoxia, and hypotension as the primary objective of study was to compare two scoring systems. Only moderate and severe head injury patients were included in the study, so the performance of the scores in mild head injury can only be extrapolated. A multicenter study with larger sample size would be required to confirm the findings of our study.
Conclusions
Though the FOUR score provides details of other neurological examination useful for assessment of comatose patients, the individual components of the FOUR scores were not significant predictors independently. Though GCS has some shortcomings, its accuracy was similar to the FOUR score for predicting mortality. However, the FOUR score can be used in patients with severe coma for sub-categorization of patients with lowest GCS. The predictive value of the FOUR score on admission of patients with TBI is no better than the GCS score.
References
Bastos PG, Sun X, Wagner DP, Wu AW, Knaus WA (1993) Glasgow Coma Scale score in the evaluation of outcome in the intensive care unit: findings from the Acute Physiology and Chronic Health Evaluation III study. Crit Care Med 21:1459–1465
Bhatty GB, Kapoor N (1993) The Glasgow Coma Scale: a mathematical critique. Acta Neurochir 120:132–135
Bishara SN, Partridge FM, Godfrey HP, Knight RG (1992) Post-traumatic amnesia and Glasgow Coma Scale related to outcome in survivors in a consecutive series of patients with severe closed-head injury. Brain Inj 6:373–380
Chen B, Grothe C, Schaller K (2013) Validation of new neurological score (FOUR score) in the assessment of neurosurgical patients with severely impaired consciousness. Acta Neurochir 155:2133–2139
Gennarelli TA, Champion HR, Copes WS, Sacco WJ (1994) Comparison of mortality, morbidity, and severity of 59,713 head injured patients with 114,447 patients with extracranial injuries. J Trauma 37:962–968
Jalali R, Rezaei M (2014) A comparison of the Glasgow Coma Scale score with full outline of unresponsiveness scale to predict patients’ traumatic brain injury outcomes in intensive care units. Crit Care Res Pract 289803. doi:10.1155/2014/289803
McNett M, Amato S, Gianakis A, Grimm D, Philippbar SA, Belle J, Moran C (2014) The FOUR score and GCS as predictors of outcome after traumatic brain injury. Neurocrit Care 21:52–57
MRC CRASH Trial Collaborators, Perel P, Arango M, Clayton T, Edwards P, Komolafe E, Poccock S, Roberts I, Shakur H, Steyerberg E, Yutthakasemsunt S (2008) Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ 336:425–429
Okasha AS, Fayed AM, Saleh AS (2014) The FOUR score predicts mortality, endotracheal intubation and ICU length of stay after traumatic brain injury. Neurocrit Care 21:496–504
Poon WS, Zhu XL, Ng SC, Wong GK (2005) Predicting one year clinical outcome in traumatic brain injury at the beginning of rehabilitation. Acta Neurochir 93(Suppl):207–208
Sadaka F, Patel D, Lakshmanan R (2012) The FOUR score predicts outcome in patients after traumatic brain injury. Neurocrit Care 16:95–101
Shukla D, Devi BI, Agarwal A (2011) Outcome measures for traumatic brain injury. Clin Neurol Neurosurg 13:435–441
Shukla D, Devi BI (2010) Mild traumatic brain injury in adults. J Neurosci Rural Pract 1:82–88
Stead LG, Wijdicks EF, Bhagra A, Kashyap R, Bellolio MF, Nash DL, Enduri S, Schears R, William B (2009) Validation of New Coma Scale, the FOUR score, in the Emergency Department. Neurocrit Care 10:50–54
Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. A practical scale. Lancet 2:81–84
Wijdicks EF, Bamlet WR, Maramattom BV, Manno EM, McClelland RL (2005) Validation of a new coma scale: the FOUR score. Ann Neurol 58:585–593
Widjicks EF, Kramer AA, Rohs T Jr, Hanna S, Sadaka F, O’Brien J, Bible S, Dickess SM, Foss M (2015) Comparison of the full outline of UnResponsiveness score and the Glasgow Coma Scale in predicting mortality in critically ill patients. Crit Care Med 43:439–444
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saika, A., Bansal, S., Philip, M. et al. Prognostic value of FOUR and GCS scores in determining mortality in patients with traumatic brain injury. Acta Neurochir 157, 1323–1328 (2015). https://doi.org/10.1007/s00701-015-2469-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2469-6