Abstract
Purpose
Laparoscopic liver resection (LLR) for hepatocellular carcinoma (HCC) remains controversial, especially for tumors larger than 5 cm. We compared the short- and long-term outcomes of laparoscopic and open liver resection (OLR) for large HCC.
Methods
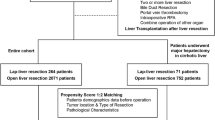
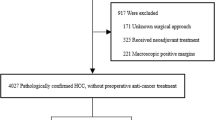
Patients with large HCC after curative hepatectomy were enrolled. To compare the short-term outcomes, propensity score matching (PSM) and inverse probability treatment weighting (IPTW) were performed to reduce the effect of confounding factors, respectively. Subsequently, Cox-regression analyses were conducted to identify the independent risk factors associated with decreased recurrence-free survival (RFS) and poor overall survival (OS).
Result
There were 265 patients enrolled in the final analysis: 146 who underwent OLR and 119 who underwent LLR. There was no significant difference between the OLR and LLR groups according to PSM and IPTW analysis (all P > 0.05). Multivariable analysis revealed that LLR was not independently associated with poorer OS (HR 1.15, 95% CI 0.80–1.67, P = 0.448) or RFS (HR 1.22, 95% CI 0.88–1.70, P = 0.238).
Conclusion
There were no significant differences in perioperative complications or long-term prognosis between LLR and OLR for large HCC, which provides evidence for standard laparoscopic surgical practice with adequate surgeon experience and careful patient selection.



Similar content being viewed by others
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- LLR:
-
Laparoscopic liver resection
- OLR:
-
Open liver resection
- RFS:
-
Recurrence-free survival
- OS:
-
Overall survival
- BMI:
-
Body mass index
- PS:
-
Performance status
- PLT:
-
Platelet count
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate transaminase
- AFP:
-
Alpha-fetoprotein
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- PSM:
-
Propensity score matching
- IPTW:
-
Inverse probability treatment weighting
References
Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. Hepatocell Carcinoma Nat Rev Dis Primers. 2021;7:6.
Morise Z. Developments and perspectives of laparoscopic liver resection in the treatment of hepatocellular carcinoma. Surg Today. 2019;49:649–55.
Morikawa T, Ishida M, Takadate T, Aoki T, Ohtsuka H, Mizuma M, et al. Laparoscopic partial liver resection improves the short-term outcomes compared to open surgery for liver tumors in the posterosuperior segments. Surg Today. 2019;49:214–23.
Chen Y, Yu L, Quan C. Laparoscopic versus open hepatectomy for elderly patients with hepatocellular carcinoma. J BUON. 2020;25:1404–12.
Wang W, Huang Z, Guo B, Liu S, Xiao W, Liang J. Short- and long-term outcomes of laparoscopic hepatectomy in elderly patients with hepatocellular carcinoma. J BUON. 2018;23:971–8.
Wang XT, Wang HG, Duan WD, Wu CY, Chen MY, Li H, et al. Pure laparoscopic versus open liver resection for primary liver carcinoma in elderly patients: a single-center. Case-Matched Study Med (Baltimore). 2015;94: e1854.
El-Gendi A, El-Shafei M, El-Gendi S, Shawky A. Laparoscopic versus open hepatic resection for solitary hepatocellular carcinoma less than 5 cm in cirrhotic patients: a randomized controlled study. J Laparoendosc Adv Surg Tech A. 2018;28:302–10.
Buell J F, Cherqui D, Geller D A, O', Rourke N, Iannitti D, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825–30.
Wakabayashi G. What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection. Hepatobiliary Surg Nutr. 2016;5:281–9.
Ciria R, Gomez-Luque I, Ocaña S, Cipriani F, Halls M, Briceño J, et al. A systematic review and meta-analysis comparing the short- and long-term outcomes for laparoscopic and open liver resections for hepatocellular carcinoma: updated results from the european guidelines meeting on laparoscopic liver surgery, southampton, UK, 2017. Ann Surg Oncol. 2019;26:252–63.
Chen XP. Expert consensus on laparoscopic hepatectomy (2013 version). J Huazhong Univ Sci Technolog Med Sci. 2013;33:791–7.
Ishizawa T, Gumbs AA, Kokudo N, Gayet B. Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg. 2012;256:959–64.
Chan KM, Wang YC, Wu TH, Lee CF, Wu TJ, Chou HS, et al. The preference for anterior approach major hepatectomy: experience over 3 decades and a propensity score-matching analysis in right hepatectomy for hepatocellular carcinoma. Medicine (Baltimore). 2015;94: e1385.
Liang L, Li C, Wang MD, Wang H, Zhou YH, Zeng YY, et al. Development and validation of a novel online calculator for estimating survival benefit of adjuvant transcatheter arterial chemoembolization in patients undergoing surgery for hepatocellular carcinoma. J Hematol Oncol. 2021;14:165.
Liang L, Wang MD, Zhang YM, Zhang WG, Zhang CW, Lau WY, et al. Association of postoperative biomarker response with recurrence and survival in patients with hepatocellular carcinoma and high alpha-fetoprotein expressions (>400 ng/ml). J Hepatocell Carcinoma. 2021;8:103–18.
Strasberg SM, Phillips C. Use and dissemination of the brisbane 2000 nomenclature of liver anatomy and resections. Ann Surg. 2013;257:377–82.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Hullsiek KH, Louis TA. Propensity score modeling strategies for the causal analysis of observational data. Biostatistics. 2002;3:179–93.
Linden A, Adams JL. Combining the regression discontinuity design and propensity score-based weighting to improve causal inference in program evaluation. J Eval Clin Pract. 2012;18:317–25.
D', Agostino R B Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998;17:2265–81.
Shelat VG, Cipriani F, Basseres T, Armstrong TH, Takhar AS, Pearce NW, et al. Pure laparoscopic liver resection for large malignant tumors: does size matter. Ann Surg Oncol. 2015;22:1288–93.
Gil E, Kwon C, Kim JM, Choi GS, Heo JS, Cho W, et al. Laparoscopic liver resection of hepatocellular carcinoma with a tumor size larger than 5 cm: review of 45 cases in a tertiary institution. J Laparoendosc Adv Surg Tech A. 2017;27:799–803.
Fu XT, Tang Z, Shi YH, Zhou J, Liu WR, Gao Q, et al. Laparoscopic versus open left lateral segmentectomy for large hepatocellular carcinoma: a propensity score-matched analysis. Surg Laparosc Endosc Percutan Tech. 2019;29:513–9.
Yang TH, Chen JL, Lin YJ, Chao YJ, Shan YS, Hsu HP, et al. Laparoscopic surgery for large left lateral liver tumors: safety and oncologic outcomes. Surg Endosc. 2018;32:4314–20.
Levi Sandri GB, Spoletini G, Vennarecci G, Francone E, Abu Hilal M, Ettorre GM. Laparoscopic liver resection for large HCC: short- and long-term outcomes in relation to tumor size. Surg Endosc. 2018;32:4772–9.
Kwon Y, Han HS, Yoon YS, Cho JY. Are large hepatocellular carcinomas still a contraindication for laparoscopic liver resection. J Laparoendosc Adv Surg Tech A. 2015;25:98–102.
Chiang MH, Tsai KY, Chen HA, Wang WY, Huang MT. Comparison of surgical outcomes for laparoscopic liver resection of large hepatocellular carcinomas: A retrospective observation from single-center experience. Asian J Surg. 2021;44:1376–82.
Hasegawa K, Kokudo N, Imamura H, Matsuyama Y, Aoki T, Minagawa M, et al. Prognostic impact of anatomic resection for hepatocellular carcinoma. Ann Surg. 2005;242:252–9.
Cho JY, Han HS, Choi Y, Yoon YS, Kim S, Choi JK, et al. Association of remnant liver ischemia with early recurrence and poor survival after liver resection in patients with hepatocellular carcinoma. JAMA Surg. 2017;152:386–92.
Rossi G, Tarasconi A, Baiocchi G, De', Angelis G L, Gaiani F, et al. Fluorescence guided surgery in liver tumors: applications and advantages. Acta Biomed 2018;89:135–40.
Ishizawa T, Zuker NB, Kokudo N, Gayet B. Positive and negative staining of hepatic segments by use of fluorescent imaging techniques during laparoscopic hepatectomy. Arch Surg. 2012;147:393–4.
Huang ZY, Liang BY, Xiong M, Dong KS, Zhang ZY, Zhang EL, et al. Severity of cirrhosis should determine the operative modality for patients with early hepatocellular carcinoma and compensated liver function. Surgery. 2016;159:621–31.
Vega EA, Kutlu OC, Joechle K, De La Cruz N, Ko D, Conrad C. Preoperative prognosticators of safe laparoscopic hepatocellular carcinoma resection in advanced cirrhosis: a propensity score matching population-based analysis of 1799 western patients. J Gastrointest Surg. 2019;23:1157–65.
Halls MC, Cipriani F, Berardi G, Barkhatov L, Lainas P, Alzoubi M, et al. Conversion for unfavorable intraoperative events results in significantly worse outcomes during laparoscopic liver resection: lessons learned from a multicenter review of 2861 cases. Ann Surg. 2018;268:1051–7.
Goh BK, Chan CY, Wong JS, Lee SY, Lee VT, Cheow PC, et al. Factors associated with and outcomes of open conversion after laparoscopic minor hepatectomy: initial experience at a single institution. Surg Endosc. 2015;29:2636–42.
Ai JH, Li JW, Chen J, Bie P, Wang SG, Zheng SG. Feasibility and safety of laparoscopic liver resection for hepatocellular carcinoma with a tumor size of 5–10 cm. PLoS ONE. 2013;8: e72328.
Xu XF, Xing H, Han J, Li ZL, Lau WY, Zhou YH, et al. Risk factors, patterns, and outcomes of late recurrence after liver resection for hepatocellular carcinoma: a multicenter study from China. JAMA Surg. 2019;154:209–17.
Diao YK, Liu JW, Wu H, Wang MD, Fan XP, Chen TH, et al. Long-term oncologic outcomes of liver resection for hepatocellular carcinoma in adolescents and young adults: a multicenter study from a hepatitis B virus-endemic area. Am J Surg. 2021;222:751–8.
Jia HD, Liang L, Li C, Wu H, Wang H, Liang YJ, et al. Long-term surgical outcomes of liver resection for hepatocellular carcinoma in patients with hbv and hcv co-infection: a multicenter observational study. Front Oncol. 2021;11: 700228.
Rajyaguru DJ, Borgert AJ, Smith AL, Thomes RM, Conway PD, Halfdanarson TR, et al. Radiofrequency ablation versus stereotactic body radiotherapy for localized hepatocellular carcinoma in nonsurgically managed patients: analysis of the national cancer database. J Clin Oncol. 2018;36:600–8.
Funding
Funding for the study was provided by Zhejiang Provincial People’s Hospital (No. ZRY2020A004), Health Commission of Zhejiang Province (No.2022KY532, No.2018KY261), General scientific research project of Education Department of Zhejiang Province (No.Y201840617) and Lishui Public welfare technology application research project (No. 2022GYX50).
Author information
Authors and Affiliations
Contributions
K-JZ, LL, Y-KD and Y-MX contributed equally to this work. Dr J-WL and D-SH had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: K-JZ, LL, D-SH and J-WL. Acquisition, analysis, or interpretation of data: D-DW, F-QX, T-WY, W-FL, JC, G-LS, W-FY, YL, and Z-QX. Drafting of the manuscript: K-JZ and LL. Critical revision of the manuscript for important intellectual content: J-GZ and C-WZ. Statistical analysis: K-JZ and Y-KD. Obtained funding: LL. Administrative, technical, or material support: C-WZ, and J-WL. Study supervision: D-SH and J-WL. Correspondence to: Dr. Jun-Wei Liu, or Dr. Dong-Sheng Huang.
Corresponding author
Ethics declarations
Conflict of interest
None reported.
Role of the Funder/Sponsor
The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, KJ., Liang, L., Diao, YK. et al. Short- and long-term outcomes of laparoscopic versus open liver resection for large hepatocellular carcinoma: a propensity score study. Surg Today 53, 322–331 (2023). https://doi.org/10.1007/s00595-022-02576-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02576-7