Abstract
Purpose
Many patients with coronavirus disease 2019 require mechanical ventilation and tracheostomy. However, the timing and indications for tracheostomy are controversial. This study assessed 11 patients with coronavirus disease 2019 who underwent tracheostomy with clinical information and retrospective analyses.
Methods
A single-center retrospective observational study was performed on patients with coronavirus disease 2019 who underwent tracheostomy between 2020 and 2021.
Results
Failure to wean was the most common indication for tracheostomy, followed by extracorporeal membrane oxygenation decannulation and the need for secretion management. After tracheostomy, six patients (54.5%) were liberated from the ventilator. The time from intubation to tracheostomy (21.1 ± 9.14 days) was correlated with the duration of ventilator dependency (36.83 ± 20.45 days, r2 = 0.792, p = 0.018). The mean Acute Physiological and Chronic Health Evaluation II score was significantly lower in the ventilator-liberated group (23 ± 2.77) than in the non-ventilator-liberated group (31 ± 6.13, p = 0.0292). Furthermore, patients with Acute Physiological and Chronic Health Evaluation II scores of < 27 points achieved ventilator liberation and a long-term survival (p = 0.0006).
Conclusions
This study describes the outcomes of a cohort of patients who underwent tracheostomy after intubation for coronavirus disease 2019. The Acute Physiological and Chronic Health Evaluation II score predicted whether or not the patient could achieve ventilator liberation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has resulted in many patients being admitted to the intensive-care unit (ICU) [1]. Approximately 70% of patients admitted to the ICU require mechanical ventilation [2], and tracheostomy is scheduled to wean patients from sedation and ventilatory support, improve communication, facilitate rehabilitation, and eventually reduce long-term complications [2].
There have been a number of reports on the surgical methods, timing of tracheostomy, and its prognosis [3,4,5]. However, while evidence for surgical procedures and prevention of infection by medical staff has been established [2,3,4,5,6], the timing and indication of tracheostomy are controversial. Some reports have shown that patients who undergo earlier tracheostomy tend to achieve earlier ventilator liberation than others [3], and another report mentioned that tracheostomy should be performed approximately 7–14 days after intubation [5]. However, previous studies have had confounding factors, including a selection bias of healthier patients for early tracheostomy [3].
We therefore evaluated 11 patients with COVID-19 who underwent tracheostomy with clinical information and performed a retrospective analysis.
Methods
COVID-19 patients who underwent tracheostomy between 2020 and 2021 were included in this study. COVID-19 was confirmed through a polymerase chain reaction (PCR) assay, development of severe respiratory failure requiring mechanical ventilation, and tracheostomy. Medical charts were reviewed to obtain clinical findings, including patient characteristics and the Acute Physiology and Chronic Health Evaluation II (APACHE II) score.
The obtained data included the age, sex, body mass index (BMI), medical history (e.g., obesity, chronic lung disease, renal failure, liver disease, and diabetes), computed tomography (CT) findings before intubation, indications for tracheostomy, APACHE II score, length of ventilator dependency, and performance status after discharge. CT images before intubation were evaluated for common characteristics of COVID-19, such as ground-glass opacity, consolidation, and a crazy-paving pattern [7]. To quantify the extent of consolidations, each lobe was scored from 0 to 5 as follows: score 0, 0% involvement; score 1, < 5% involvement; score 2, 5–25% involvement; score 3, 26–49% involvement; score 4, 50–75% involvement; and score 5, > 75% involvement [8]. The APACHE II score was calculated from the patient’s age and 12 parameters: PaO2, temperature, mean arterial pressure, arterial pH, heart rate, respiratory rate, sodium, potassium, creatinine, hematocrit, leukocyte count, and Glasgow Coma Scale. In addition, information about each patient’s previous health status (surgery, history of organ insufficiency, and immunocompromised state) was evaluated. The worst parameters in the first four hours of hospitalization were selected to calculate the scores. The ventilator liberation and observed death rates were compared with the APACHE II score. In addition, the accuracy of outcome prediction by the APACHE II system was assessed using a receiver operating characteristics (ROC) curve and Pearson’s correlation coefficient and its significance test. Statistical analyses were performed using the chi-square test, and statistical significance was set at p < 0.05.
This retrospective observational study was approved by the Institutional Ethics Review Board. Furthermore, written informed consent was waived by the review board because only anonymous data were used in this study.
Results
Tracheostomy was performed in 8 male and 3 female COVID-19 patients with acute respiratory failure (Table1). Patients’ ages ranged from 50 to 81 (average, 69.5) years old, and the BMI ranged from 17.8 to 35.2 (average, 25.8) kg/m2. The number of elderly people (≥ 70 years old) was 6 (54.5%). The medical history included renal failure in 6 cases (54.5%), liver disease in 4 cases (36.4%), and diabetes in 6 cases (54.5%). The common chest CT features of this study included ground-glass opacity (100%), consolidation (100%), and a crazy-paving pattern (60%). The CT scores of the consolidation were 7.7 ± 4.24 (range 2–14). All patients developed severe respiratory failure requiring mechanical ventilation and required treatment in the ICU.
Failure to wean was the most common indication for tracheostomy (8 patients, 72.7%), followed by extracorporeal membrane oxygenation (ECMO) decannulation (2 patients, 18.2%), and need for secretion management (1 patient, 9.1%).
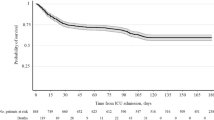
After tracheostomy, 6 patients (54.5%) were liberated from the ventilator. The average duration of ventilator dependency was 36.83 ± 20.45 (range 9–76) days. The average intubation time before tracheostomy in these patients was 21.1 ± 9.14 (range 10–36) days. Although there was no marked difference in the outcomes due to the duration from COVID-19 infection to intubation (p = 0.09), there was a correlation between the time from intubation to tracheostomy and the duration of ventilator dependency (Fig. 1r2 = 0.792, p = 0.018).
The predicted risk of mortality was calculated according to the APACHE II death equation, which showed a perfect correlation between the APACHE II score and the predicted death rate (r2 = 0.8954, p < 0.0001). Although there was no significant difference in the APACHE II score between survivors and non-survivors (p = 0.0658), the mean APACHE II score was 23 ± 2.77 and 31 ± 6.13 in the ventilator-liberated and non-ventilator-liberated groups (p = 0.0292), respectively. The predicted death rate, ventilator liberation rate, and observed death rate according to the APACHE II score are summarized in Table 2, and the receiver operating characteristics curve was constructed from the APACHE II score and ventilator liberation rate (Fig. 2). The APACHE II scoring system was found to be a statistically significant predictive marker of ventilator liberation (area under the curve of 0.900, 95% confidence interval 0.69–1.00, p = 0.0285).
Discussion
We herein report the single-center outcomes of tracheostomy patients with COVID-19 in Japan. This study demonstrated for the first time that the APACHE II score was a predictive marker of the ventilator liberation rate in COVID-19 patients who underwent tracheostomy. We also confirmed that early tracheostomy in these patients resulted in earlier ventilator liberation.
The timing of tracheostomy for COVID-19 has been studied. Previous research has shown that tracheostomy should be performed 7–14 days after intubation to improve the treatment prognosis of patients with COVID-19 [5]. Another study found that patients who underwent earlier tracheostomy tended to achieve earlier ventilator liberation than others [3]. Although several studies have recommended early tracheostomy, they also had a selection bias of healthier patients receiving earlier tracheostomy as a confounding factor [3]; in addition, the overwhelming of medical systems and availability of facilities should be considered when making such decision. Our study showed a similar correlation with previous studies between the duration from intubation to tracheostomy and duration of ventilator dependency. In addition to the timing of tracheostomy, we suggest that the APACHE II score be considered as an indicator of the clinical outcome after tracheostomy.
APACHE II is the most commonly used severity-of-disease scoring system for intensive care. The worst value for physiological variables in the 24 h of patient admission was calculated as an integer score from 0 to 71 [9, 10]. Although several scoring systems have been developed, the APACHE II score is considered particularly useful, as substantial documentation has been based on APACHE II [9, 10]. Because previous studies have revealed that the APACHE II scoring system shows good discrimination for predicting ICU mortality, we hypothesized that the APACHE II scoring system might be a predictive marker of the ventilator liberation rate in COVID-19 patients who underwent tracheostomy. In the present study, the mortality rate was significantly higher at ≥ 27 points than < 27 points (p = 0.0006). Among the patients with < 27 points according to APACHE II, 83.3% (5/6) achieved ventilator liberation and a long-term survival. Because there are no specific surgical indications for tracheostomy that have been defined for COVID-19 patients thus far, tracheostomy should be considered in cases with an APACHE II score of ≤ 26 points in the early phase.
Several limitations associated with the present study warrant mention. First, although our study hypothesized that patients with a low APACHE II score tended to have earlier tracheostomies and higher ventilator liberation rate than those with a higher score, no correlations were observed between the APACHE II score and either timing of intubation (p = 0.49) or the duration of ventilator dependence in the ventilator-liberated patients (p = 0.56). Second, due to the small sample size, we were unable to determine the correlation between the APACHE II score and early tracheostomy or duration of ventilator dependency. In addition, the retrospective nature of the study and small sample size (11 patients over a 2-year period) made it difficult to perform a multivariate analysis or propensity score matching to assess whether or not early tracheostomy does indeed allow for earlier ventilator liberation. For this assessment, further studies that divide patients into two groups (early and late tracheostomy groups) and either prospectively compare ventilator liberation rates or perform a multivariate analysis or propensity score matching are needed. Furthermore, various variants of coronavirus were included in our study population, as this study included patients with long-term morbidity. Finally, this study had no control, including cases of continuous intubation without tracheostomy. In our institution, the mortality rates of patients with COVID-19 who required intensive care and underwent tracheostomy were 38.6% (22/57) and 36.6% (7/11), respectively. However, this is not comparable due to variations in the COVID-19 variant involved and patients’ background characteristics. A further cohort analysis is required to elucidate the potential benefits of tracheostomy.
Conclusions
We reported the outcomes of a cohort of patients who underwent tracheostomy after intubation for COVID-19. Correlations between the APACHE II score and whether or not a patient could achieve ventilator liberation were found. Therefore, the further assessment of outcomes after tracheostomy is required.
References
Torzilli G, Galvanin J, Viganò L, Donadon M, Montorsi M. COVID-19: emerging challenges for oncological surgery. Glob Health Med. 2020;2:197–9. https://doi.org/10.35772/ghm.2020.01039.
Rovira A, Dawson D, Walker A, Tornari C, Dinham A, Foden N, et al. Tracheostomy care and decannulation during the COVID-19 pandemic. A multidisciplinary clinical practice guideline. Eur Arch Otorhinolaryngol. 2021;278:313–21. https://doi.org/10.1007/s00405-020-06126-0.
Chao TN, Harbison SP, Braslow BM, Hutchinson CT, Rajasekaran K, Go BC, et al. Outcomes after tracheostomy in COVID-19 patients. Ann Surg. 2020;272:e181–6. https://doi.org/10.1097/SLA.0000000000004166.
Nishio N, Hiramatsu M, Goto Y, Shindo Y, Yamamoto T, Jingushi N, et al. Surgical strategy and optimal timing of tracheostomy in patients with COVID-19: early experiences in Japan. Auris Nasus Larynx. 2021;48:518–24. https://doi.org/10.1016/j.anl.2020.11.004.
Obata K, Miyata R, Yamamoto K, Byn-Ya N, Kasai T, Inoue H, et al. Tracheostomy in patients with COVID-19: a single-center experience. In Vivo. 2020;34:3747–51. https://doi.org/10.21873/invivo.12224.
Yokokawa T, Ariizumi Y, Hiramatsu M, Kato Y, Endo K, Obata K, et al. Management of tracheostomy in COVID-19 patients: the Japanese experience. Auris Nasus Larynx. 2021;48:525–9.
Ki K, Wu J, Wu F, Guo D, Chen L, Fang Z, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020;55:327–31. https://doi.org/10.1097/RLI.0000000000000672.
Chang YC, Yu CJ, Chang SC, Galvin JR, Liu HM, Hsiao CH, et al. Pulmonary sequelae in convalescent patients after severe acute respiratory syndrome: evaluation with thin-section CT. Radiology. 2005;236:1067–75. https://doi.org/10.1148/radiol.2363040958.
Godinjak A, Iglica A, Rama A, Tančica I, Jusufović S, Ajanović A, et al. Predictive value of SAPS II and Apache II scoring systems for patient outcome in a medical intensive care unit. Acta Med Acad. 2016;45:97–103. https://doi.org/10.5644/ama2006-124.165.
Kulkarni SV, Naik AS, Subramanian N. Apache-II scoring system in perforative peritonitis. Am J Surg. 2007;194:549–52.
Funding
This work was supported by the NCGM COVID-19 Gift Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (NCGM-S-004251-00) and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent for publication
Written informed consent was waived by the review board because only anonymous data were used in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sumiya, R., Nagasaka, S., Okamoto, T. et al. Clinical outcomes after tracheostomy in patients with coronavirus disease 2019: a single-center experience in Japan. Surg Today 53, 130–134 (2023). https://doi.org/10.1007/s00595-022-02541-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-022-02541-4