Abstract
Purpose
Previous studies have reported that sarcopenia increases the risk of postoperative complications following colorectal resection. This retrospective study assessed the postoperative complications of rectal resection associated with sarcopenia.
Methods
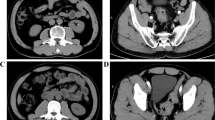
We retrospectively analyzed 262 patients who underwent curative low anterior resection for primary rectal cancer from January 2008 to May 2020 at our institution. The patients were divided into a sarcopenia group (normalized total psoas muscle area < 6.36 cm2/m2 in males and < 3.92 cm2/m2 in females; N = 49) and a non-sarcopenia group (N = 213).
Results
The overall rate of postoperative complications within 30 days of surgery was higher in the sarcopenia group than in the non-sarcopenia group (46.9 vs. 29.6%; P = 0.028). The rate of postoperative remote infections was higher in the sarcopenia group than in the non-sarcopenia group (12.2 vs. 2.8%; P = 0.012). Sarcopenia was found to be a predictor of remote infection by a multivariate analysis (odds ratio, 4.08; 95% confidence interval, 1.12–14.80; P = 0.033).
Conclusion
Sarcopenia diagnosed using the psoas muscle index was found to be an independent predictive factor for postoperative remote infection after curative low anterior resection for rectal cancer.



Similar content being viewed by others
Availability of data and materials
The datasets used and analyzed during this study are available from the corresponding author upon reasonable request.
References
Rosenberg IH. Sarcopenia: origins and clinical relevance. Clin Geriatr Med. 2011;27:337–9.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Age. 2010;39:412–23.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101.
Miyamoto Y, Baba Y, Sakamoto Y, Ohuchi M, Tokunaga R, Kurashige J, et al. Negative impact of skeletal muscle loss after systemic chemotherapy in patients with unresectable colorectal cancer. PLoS ONE. 2015;10: e0129742.
Ida S, Watanabe M, Yoshida N, Baba Y, Umezaki N, Harada K, et al. Sarcopenia is a predictor of postoperative respiratory complications in patients with esophageal cancer. Ann Surg Oncol. 2015;22:4432–7.
Fukushima H, Yokoyama M, Nakanishi Y, Tobisu K, Koga F. Sarcopenia as a prognostic biomarker of advanced urothelial carcinoma. PLoS ONE. 2015;10: e0115895.
Voron T, Tselikas L, Pietrasz D, Pigneur F, Laurent A, Compagnon P, et al. Sarcopenia impacts on short- and long-term results of hepatectomy for hepatocellular carcinoma. Ann Surg. 2015;261:1173–83.
Levolger S, van Vugt JLA, de Bruin RWF, IJzermans JNM. Systematic review of sarcopenia in patients operated on for gastrointestinal and hepatopancreatobiliary malignancies. Br J Surg. 2015; 102:1448–58.
Malietzis G, Aziz O, Bagnall NM, Johns N, Fearon KC, Jenkins JT. The role of body composition evaluation by computerized tomography in determining colorectal cancer treatment outcomes: a systematic review. Eur J Surg Oncol. 2015;41:186–96.
Jochum SB, Kistner M, Wood EH, Hoscheit M, Nowak L, Poirier J, et al. Is sarcopenia a better predictor of complications than body mass index? Sarcopenia and surgical outcomes in patients with rectal cancer. Colorectal Dis. 2019;21:1372–8.
Takeda Y, Akiyoshi T, Matsueda K, Fukuoka H, Ogura A, Miki H, et al. Skeletal muscle loss is an independent negative prognostic factor in patients with advanced lower rectal cancer treated with neoadjuvant chemoradiotherapy. PLoS ONE. 2018;13: e0195406.
Okumura S, Kaido T, Hamaguchi Y, Fujimoto Y, Masui T, Mizumoto M, et al. Impact of preoperative quality as well as quantity of skeletal muscle on survival after resection of pancreatic cancer. Surgery. 2015;157:1088–98.
Hamaguchi Y, Kaido T, Okumura S, Kobayashi A, Hammad A, Tamai Y, et al. Proposal for new diagnostic criteria for low skeletal muscle mass based on computed tomography imaging in Asian adults. Nutrition. 2016;32:1200–5.
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients (in Japanese with English abstract). Nihon Geka Gakkai zasshi. 1984;85:1001–5.
Nishimuta H, Kusachi S, Watanabe M, Asai K, Kiribayashi T, Niitsuma T, et al. Impact of postoperative remote infection on length of stay and medical costs in hospitals in Japan. Surg Today. 2021;51:212–8.
Tomotaki A, Kumamaru H, Hashimoto H, Takahashi A, Ono M, Iwanaka T, et al. Evaluating the quality of data from the Japanese National Clinical Database 2011 via a comparison with regional government report data and medical charts. Surg Today. 2019;49:65–71.
Hasegawa H, Takahashi A, Kakeji Y, Ueno H, Eguchi S, Endo I, et al. Surgical outcomes of gastroenterological surgery in Japan: report of the National Clinical Database 2011–2017. Ann Gastroenterol Surg. 2019;3:426–50.
Paun BC, Cassie S, MacLean AR, Dixon E, Buie WD. Postoperative complications following surgery for rectal cancer. Ann Surg. 2010;251:807–18.
Trejo-Avila M, Bozada-Gutiérrez K, Valenzuela-Salazar C, Herrera-Esquivel J, Moreno-Portillo M. Sarcopenia predicts worse postoperative outcomes and decreased survival rates in patients with colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis. 2021. https://doi.org/10.1007/s00384-021-03839-4.
Nakanishi R, Oki E, Sasaki S, Hirose K, Jogo T, Edahiro K, et al. Sarcopenia is an independent predictor of complications after colorectal cancer surgery. Surg Today. 2018;48:151–7.
Berkel AEM, Klaase JM, de Graaff F, Brusse-Keizer MGJ, Bongers BC, van Meeteren NLU. Patient’s skeletal muscle radiation attenuation and sarcopenic obesity are associated with postoperative morbidity after neoadjuvant chemoradiation and resection for rectal cancer. Dig Surg. 2019;36:376–83.
Bahat G, Turkmen BO, Aliyev S, Catikkas NM, Bakir B, Karan MA. Cut-off values of skeletal muscle index and psoas muscle index at L3 vertebra level by computerized tomography to assess low muscle mass. Clin Nutr. 2021. https://doi.org/10.1016/j.clnu.2021.01.010.
Arai H. Clinical management of sarcopenia: secondary publication of Geriatrics & Gerontology International 2018;18 S1:1–44. JMA J. 2020; 3:95–100.
Nishiguchi S, Hino K, Moriya K, Shiraki M, Hiramatsu A, Nishikawa H. Assessment criteria for sarcopenia in liver disease (first edition): report from the working group for creation of sarcopenia assessment criteria in the Japan Society of Hepatology (in Japanese). Kanzo. 2016;57:353–68.
Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect. 2017;96:1–15.
de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009;37:387–97.
Niitsuma T, Kusachi S, Takesue Y, Mikamo H, Asai K, Watanabe M. Current status of postoperative infections after digestive surgery in Japan: the Japan Postoperative Infectious Complications Survey in 2015. Ann Gastroenterol Surg. 2019;3:276–84.
Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE. Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer. 2012;107:931–6.
Olmez T, Karakose E, Keklikkiran ZZ, Ofluoglu CB, Bas T, Uzun O, et al. Relationship between Sarcopenia and Surgical Site Infection in Patients Undergoing Colorectal Cancer Surgical Procedures. Surg Infect (Larchmt). 2020;21:451–6.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al; Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48:16–31.
Kameyama H, Sakata J, Hanyu T, Ichikawa H, Nakano M, Nagahashi M, et al. Efficacy of preoperative frailty assessment in patients with gastrointestinal disease. Geriatr Gerontol Int. 2021;21:327–30.
Acknowledgements
We would like to thank Editage (www.editage.jp) for the English language editing.
Funding
This study was not supported by any associations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interest
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uehara, H., Yamazaki, T., Iwaya, A. et al. Is radiological psoas muscle area measurement a predictor of postoperative complications after rectal resection for rectal cancer? A retrospective study. Surg Today 52, 306–315 (2022). https://doi.org/10.1007/s00595-021-02346-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02346-x