Abstract
Purpose
To evaluate the effect of scheduled intravenous acetaminophen administration versus nonsteroidal anti-inflammatory drugs on postoperative pain and short-term outcomes after esophagectomy.
Methods
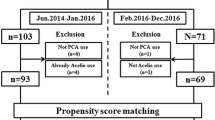
The subjects of this study were 150 consecutive patients who underwent esophagectomy for esophageal cancer. Seventy-seven patients received scheduled intravenous acetaminophen and the other 73 received NSAIDs enterally for postoperative pain management. We compared the postoperative pain and short-term outcomes between the groups. Inverse probability of treatment weighting (IPTW) based on propensity scores was used to control for selection bias.
Results
The visual analog scale (VAS) of postoperative pain was lower in the acetaminophen group than in the NSAIDs group, based on the mean values of chest VAS on postoperative days (PODs) 0, 4, 5, and 6 and the mean values of abdomen VAS on PODs 4, 5, and 6. The incidence of anastomotic leakage and postoperative delirium was lower in the acetaminophen group than in the NSAIDs group (anastomotic leakage, odds ratio (OR) 0.3, p = 0.01; postoperative delirium, OR 0.19, p < 0.01).
Conclusion
Scheduled intravenous acetaminophen administration is effective and feasible for the postoperative pain management of patients undergoing esophagectomy and may be associated with a lower incidence of anastomotic leakage and postoperative delirium.

Similar content being viewed by others
References
Sakatoku Y, Fukaya M, Miyata K, Itatsu K, Nagino M. Clinical value of a prophylactic minitracheostomy after esophagectomy: analysis in patients at high risk for postoperative pulmonary complications. BMC Surg. 2017;17(1):120.
Visser E, Marsman M, van Rossum PSN, Cheong E, Al-Naimi K, van Klei WA, et al. Postoperative pain management after esophagectomy: a systematic review and meta-analysis. Dis Esophagus. 2017;30(10):1–11.
Findlay JM, Gillies RS, Millo J, Sgromo B, Marshall RE, Maynard ND. Enhanced recovery for esophagectomy: a systematic review and evidence-based guidelines. Ann Surg. 2014;259(3):413–31.
Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017;152(7):691–7.
Gupta A, Bah M. NSAIDs in the treatment of postoperative pain. Curr Pain Headache Rep. 2016;20(11):62.
Modasi A, Pace D, Godwin M, Smith C, Curtis B. NSAID administration post colorectal surgery increases anastomotic leak rate: systematic review/meta-analysis. Surg Endosc. 2019;33(3):879–85.
Bhangu A, Singh P, Fitzgerald JE, Slesser A, Tekkis P. Postoperative nonsteroidal anti-inflammatory drugs and risk of anastomotic leak: meta-analysis of clinical and experimental studies. World J Surg. 2014;38(9):2247–57.
Ohkura Y, Shindoh J, Ueno M, Iizuka T, Haruta S, Udagawa H. A new postoperative pain management (intravenous acetaminophen: Acelio®) leads to enhanced recovery after esophagectomy: a propensity score-matched analysis. Surg Today. 2018;48(5):502–9.
Kitagawa H, Namikawa T, Iwabu J. Scheduled intravenous acetaminophen for postoperative management of patients who had thoracoscopic esophagectomy for esophageal cancer. Anticancer Res. 2019;39(1):467–70.
Gupta A, Jakobsson J. Acetaminophen, nonsteroidal anti-inflammatory drugs, and cyclooxygenase-2 selective inhibitors: an update. Plast Reconstr Surg. 2014;134(4 Suppl 2):24S–31S.
Miyata K, Fukaya M, Itatsu K, Abe T, Nagino M. Muscle sparing thoracotomy for esophageal cancer: a comparison with posterolateral thoracotomy. Surg Today. 2016;46(7):807–14.
Kawai R, Abe T, Uemura N, Fukaya M, Saito T, Komori K, et al. Feeding catheter gastrostomy with the round ligament of the liver prevents mechanical bowel obstruction after esophagectomy. Dis Esophagus. 2017;30(6):1–8.
Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118(4):934–44.
Foster B, Twycross R, Mihalyo M, Wilcock A. Buprenorphine. J Pain Symptom Manage. 2013;45(5):939–49.
Pasqualucci V, Tantucci C, Paoletti F, Dottorini ML, Bifarini G, Belfiori R, et al. Buprenorphine vs. morphine via the epidural route: a controlled comparative clinical study of respiratory effects and analgesic activity. Pain. 1987;29(3):273–86.
McPherson ML. Demystifying opioid conversion calculations: a guide for effective dosing. 2nd ed. Bethesda: American Society of Health-System Pharmacists, Inc.; 2018.
Rice TW, Ishwaran H, Blackstone EH, Hofstetter WL, Kelsen DP, Apperson-Hansen C. Recommendations for clinical staging (cTNM) of cancer of the esophagus and esophagogastric junction for the 8th edition AJCC/UICC staging manuals. Dis Esophagus. 2016;29(8):913–9.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–79.
Smith HS. Perioperative intravenous acetaminophen and NSAIDs. Pain Med. 2011;12(6):961–81.
Fjederholt KT, Okholm C, Svendsen LB, Achiam MP, Kirkegård J, Mortensen FV. Ketorolac and other NSAIDs increase the risk of anastomotic leakage after surgery for GEJ cancers: a cohort study of 557 patients. J Gastrointest Surg. 2018;22(4):587–94.
Takeuchi M, Takeuchi H, Fujisawa DV, Miyajima K, Yoshimura K, Hashiguchi S, et al. Incidence and risk factors of postoperative delirium in patients with esophageal cancer. Ann Surg Oncol. 2012;19(12):3963–70.
Fuchita M, Khan SH, Perkins AJ, Gao S, Wang S, Kesler KA, et al. Perioperative risk factors for postoperative delirium in patients undergoing esophagectomy. Ann Thorac Surg. 2019;108:190–5.
Kawano T, Yamanaka D, Aoyama B, Tateiwa H, Shigematsu-Locatelli M, Nishigaki A, et al. Involvement of acute neuroinflammation in postoperative delirium-like cognitive deficits in rats. J Anesth. 2018;32(4):506–17.
Graham GG, Scott KF, Day RO. Tolerability of paracetamol. Drug Saf. 2005;28(3):227–40.
Subramaniam B, Shankar P, Shaefi S, Mueller A, O’Gara B, Banner-Goodspeed V, et al. Effect of intravenous acetaminophen vs placebo combined with propofol or dexmedetomidine on postoperative delirium among older patients following cardiac surgery: the DEXACET randomized clinical trial. JAMA. 2019;321(7):686–96.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jiro Kawakami and his co-authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
595_2020_2001_MOESM2_ESM.xlsx
Analysis of the impact of intravenous acetaminophen vs. NSAIDs on postoperative complications and short-term outcomes with weighted logistic regression and adjustment for chemoradiotherapy.
595_2020_2001_MOESM5_ESM.pptx
Supplementary Fig. 1. Assessment of postoperative pain using adjusted linear regression a. Daily trend of the mean value of chest VAS at rest in the acetaminophen group. b. Daily trend of the mean value of chest VAS at rest in the NSAIDs group. c. Daily trend of the mean value of abdomen VAS at rest in the acetaminophen group. b. Daily trend of the mean value of abdomen VAS at rest in the NSAIDs group.
Rights and permissions
About this article
Cite this article
Kawakami, J., Abe, T., Higaki, E. et al. Scheduled intravenous acetaminophen versus nonsteroidal anti-inflammatory drugs (NSAIDs) for better short-term outcomes after esophagectomy for esophageal cancer. Surg Today 50, 1168–1175 (2020). https://doi.org/10.1007/s00595-020-02001-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-020-02001-x