Abstract
Purpose
The present study aimed to compare robotic-assisted versus laparoscopic distal pancreatic resection and enucleation for potentially benign pancreatic neoplasms.
Methods
Patients were retrieved from a prospectively maintained database. Demographic data, tumor types, and the perioperative outcomes were retrospectively analyzed.
Results
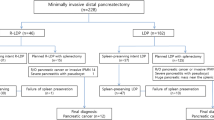
In a 10-year period, 75 patients (female, n = 44; male, n = 31; median age, 53 years [range, 9–84 years]) were identified. The majority of patients had pancreatic neuroendocrine neoplasms (n = 39, 52%) and cystic neoplasms (n = 23, 31%) with a median tumor size of 17 (3–60) mm. Nineteen (25.3%) patients underwent enucleation (robotic, n = 11; laparoscopic, n = 8) and 56 (74.7%) patients underwent distal pancreatic resection (robotic, n = 24; laparoscopic, n = 32), of those 48 (85%) underwent spleen-preserving procedures. Eight (10.7%) procedures had to be converted to open surgery. The rate of vessel preservation in distal pancreatectomy was significantly higher in robotic-assisted procedures (62.5% vs. 12.5%, p = 0.01). Twenty-six (34.6%) patients experienced postoperative complications (Clavien–Dindo grade > 3). Twenty (26.7%) patients developed a pancreatic fistula type B. There was no mortality. After a median follow-up period of 58 months (range 2–120 months), one patient (1.3%) developed local recurrence (glucagonoma) after enucleation, which was treated with a Whipple procedure.
Conclusion
The robotic approach is comparably safe, but increases the rate of splenic vessel preservation and reduces the risk of conversion to open surgery.
Similar content being viewed by others
References
Merchant NB, Parikh AA, Kooby DA. Should all distal pancreatectomies be performed laparoscopically? Adv Surg. 43:283–300. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19845186
Niu X, Yu B, Yao L, Tian J, Guo T, et al. Comparison of surgical outcomes of robot-assisted laparoscopic distal pancreatectomy versus laparoscopic and open resections: a systematic review and meta-analysis. Asian J Surg. 2018;42(1):32–45. https://doi.org/10.1016/j.asjsur.2018.08.011.
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL. Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg. 2012. https://doi.org/10.1097/SLA.0b013e318251ee09.
Mehrabi A, Hafezi M, Arvin J, Esmaeilzadeh M, Garoussi C, Emami G, et al. A systematic review and meta-analysis of laparoscopic versus open distal pancreatectomy for benign and malignant lesions of the pancreas: It’s time to randomize. Surgery (United States). 2015. https://doi.org/10.1016/j.surg.2014.06.081.
Nigri GR, Rosman AS, Petrucciani N, Fancellu A, Pisano M, Zorcolo L, et al. Metaanalysis of trials comparing minimally invasive and open distal pancreatectomies. Surg Endosc. 2010;25(5):1642–51. https://doi.org/10.1007/s00464-010-1456-5.
Soh YF, Kow AWC, Wong KY, Wang B, Chan CY, Liau KH, et al. Perioperative outcomes of laparoscopic and open distal pancreatectomy: our institution’s 5-year experience. Asian J Surg. 2012. https://doi.org/10.1016/j.asjsur.2012.04.005.
Duran H, Ielpo B, Caruso R, Ferri V, Quijano Y, Diaz E, et al. Does robotic distal pancreatectomy surgery offer similar results as laparoscopic and open approach? A comparative study from a single medical center. Int J Med Robot Comput Assist Surg MRCAS. 2014;10(3):280–5. https://doi.org/10.1002/rcs.1569.
Lee SY, Allen PJ, Sadot E, D’Angelica MI, Dematteo RP, Fong Y, et al. Distal pancreatectomy: a single institution’s experience in open, laparoscopic, and robotic approaches. J Am Coll Surg. 2015. https://doi.org/10.1016/j.jamcollsurg.2014.10.004.
Riviere D, Gurusamy KS, Kooby DA, Vollmer CM, Besselink MGH, Davidson BR, et al. Laparoscopic versus open distal pancreatectomy for pancreatic cancer. Cochrane Database Syst Rev. 2016;4:CD011391. https://doi.org/10.1002/14651858.CD011391.pub2.
Xourafas D, Ashley SW, Clancy TE. Comparison of perioperative outcomes between open, laparoscopic, and robotic distal pancreatectomy: an analysis of 1815 patients from the ACS-NSQIP procedure-targeted pancreatectomy database. J Gastrointest Surg. 2017;21(9):1442–52. https://doi.org/10.1007/s11605-017-3463-5.
Corcione F, Esposito C, Cuccurullo D, Settembre A, Miranda N, Amato F, et al. Advantages and limits of robot-assisted laparoscopic surgery: preliminary experience. Surg Endosc Other Interv Tech. 2005;19(1):117–9. https://doi.org/10.1007/s00464-004-9004-9.
Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S. Balestracci S et al Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138(7):777–84. https://doi.org/10.1001/archsurg.138.7.777.
Van Koughnett JA, Jayaraman S, Eagleson R, Quan D, van Wynsberghe A, Schlachta CM. Are there advantages to robotic-assisted surgery over laparoscopy from the surgeon’s perspective? J Robot Surg. 2009;3(2):79–82. https://doi.org/10.1007/s11701-009-0144-8.
Xu SB, Jia CK, Wang JR, Zhang RC, Mou YP. Do patients benefit more from robot assisted approach than conventional laparoscopic distal pancreatectomy? A meta-analysis of perioperative and economic outcomes. J Formos Med Assoc. 2018. https://doi.org/10.1016/j.jfma.2018.05.003.
Eckhardt S, Schicker C, Maurer E, Fendrich V, Bartsch DK. Robotic-assisted approach improves vessel preservation in spleen-preserving distal pancreatectomy. Dig Surg. 2016;33(5):406–13. https://doi.org/10.1159/000444269.
Chen S, Zhan Q, Chen J, Jin J, Deng X, Chen H, et al. Robotic approach improves spleen-preserving rate and shortens postoperative hospital stay of laparoscopic distal pancreatectomy: a matched cohort study. Surg Endosc. 2015;29(12):3507–18. https://doi.org/10.1007/s00464-015-4101-5.
Daouadi M, Zureikat AH, Zenati MS, Choudry H, Tsung A, Bartlett DL, et al. Robot-assisted minimally invasive distal pancreatectomy is superior to the laparoscopic technique. Ann Surg. 2013;257(1):128–32. https://doi.org/10.1097/SLA.0b013e31825fff08.
Goh BKP, Chan CY, Soh HL, Lee SY, Cheow PC, Chow PKH, et al. A comparison between robotic-assisted laparoscopic distal pancreatectomy versus laparoscopic distal pancreatectomy. Int J Med Robot Comput Assist Surg. 2017. https://doi.org/10.1002/rcs.1733.
Kang CM, Kim DH, Lee WJ, Chi HS. Conventional laparoscopic and robot-assisted spleen-preserving pancreatectomy: does da Vinci have clinical advantages? Surg Endosc. 2011;25(6):2004–9. https://doi.org/10.1007/s00464-010-1504-1.
Zhou JY, Xin C, Mou YP, Xu XW, Zhang MZ, Zhou YC, et al. Robotic versus laparoscopic distal pancreatectomy: a meta-analysis of short-term outcomes. PLoS ONE. 2016;11(3):1–13. https://doi.org/10.1371/journal.pone.0151189.
Guerrini GP, Lauretta A, Belluco C, Olivieri M, Forlin M, Basso S, et al. Robotic versus laparoscopic distal pancreatectomy: an up-to-date meta-analysis. BMC Surg. 2017;17(1):1–10. https://doi.org/10.1186/s12893-017-0301-3.
Strijker M, Van Santvoort HC, Besselink MG, Van Hillegersberg R, Borel Rinkes IHM, Vriens MR, et al. Robot-assisted pancreatic surgery: a systematic review of the literature. Hpb. 2012;15(1):1–10. https://doi.org/10.1111/j.1477-2574.2012.00589.x.
Liu R, Liu Q, Zhao ZM, Tan XL, Gao YX, Zhao GD. Robotic versus laparoscopic distal pancreatectomy: a propensity score-matched study. J Surg Oncol. 2017;116(4):461–9. https://doi.org/10.1002/jso.24676.
Lyman WB, Passeri M, Sastry A, Cochran A, Iannitti DA, Vrochides D, et al. Robotic-assisted versus laparoscopic left pancreatectomy at a high-volume, minimally invasive center. Surg Endosc. 2019. https://doi.org/10.1007/s00464-018-6565-6.
Mintziras I, Keck T, Werner J, Fichtner-Feigl S, Wittel U, et al. Implementation of current ENETS guidelines for surgery of small (≤2 cm) pancreatic neuroendocrine neoplasms in the german surgical community: an analysis of the prospective DGAV StuDoQ|Pancreas registry. World J Surg. 2019;43(1):175–82. https://doi.org/10.1007/s00268-018-4751-2.
Kimura W, Yano M, Sugawara S, Okazaki S, Sato T, Moriya T, Hirai I. Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein: techniques and its significance. J Hepato-Biliary-Pancreat Sci. 2010;17(6):813–23. https://doi.org/10.1007/s00534-009-0250-z.
Warshaw AL. Conservation of the spleen with distal pancreatectomy. Arch Surg (Chicago, Ill. : 1960), 1988;123(5):550–553. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/3358679
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, International Study Group on Pancreatic Surgery (ISGPS). The 2016 update of the international study group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161(3):584–91. https://doi.org/10.1016/j.surg.2016.11.014.
Gavriilidis P, Lim C, Menahem B, Lahat E, Salloum C, Azoulay D. Robotic versus laparoscopic distal pancreatectomy—the first meta-analysis. Hpb. 2016;18(7):567–74. https://doi.org/10.1016/j.hpb.2016.04.008.
Kamarajah SK, Sutandi N, Robinson SR, French JJ, White SA. Robotic versus conventional laparoscopic distal pancreatic resection: a systematic review and meta-analysis. Hpb. 2019;21(9):1107–18. https://doi.org/10.1016/j.hpb.2019.02.020.
Kyoung H, Chang H, Kang M. Robot-assisted spleen-preserving distal pancreatectomy : a single surgeon ’ s experiences and proposal of clinical application. Surg Endosc. 2013. https://doi.org/10.1007/s00464-012-2551-6.
Shoup M, Brennan MF, McWhite K, Leung DHY, Klimstra D, Conlon KC. The value of splenic preservation with distal pancreatectomy. Arch Surg (Chicago, Ill: 1960). 2013;137(2):164–168. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11822953
Koukoutsis I, Tamijmarane A, Bellagamba R, Bramhall S, Buckels J, Mirza D. The impact of splenectomy on outcomes after distal and total pancreatectomy. World J Surg Oncol. 2007;5:61. https://doi.org/10.1186/1477-7819-5-61.
Boselli C, Barberini F, Listorti C, Castellani E, Renzi C, Corsi A, et al. Distal pancreatectomy with splenic preservation: a short-term outcome analysis of the Warshaw technique. Int J Surg. 2015. https://doi.org/10.1016/j.ijsu.2015.06.051.
Yu X, Li H, Jin C, Fu D, Di Y, Hao S, et al. Splenic vessel preservation versus Warshaw’s technique during spleen-preserving distal pancreatectomy: a meta-analysis and systematic review. Langenbeck’s Arch Surg. 2015;400(2):183–91. https://doi.org/10.1007/s00423-015-1273-3.
Matsushima H, Kuroki T, Adachi T, Kitasato A, Hirabaru M, Eguchi S. Laparoscopic spleen-preserving distal pancreatectomy Laparoscopic spleen-preserving distal pancreatectomy with and without splenic vessel preservation: the role of the Warshaw procedure Laparoscopic spleen-preserving distal pancreatectomy.
Lü S, Shi X, Wang H, Ji W, Wan T, Xu M, et al. Follow-up studies for long-term postoperative complications of Warshaw operation. Zhonghua Yi Xue Za Zhi. 93(14):1096–1098. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/23902845
Ferrone CR, Konstantinidis IT, Sahani DV, Wargo JA, Fernandez-Del Castillo C, Warshaw AL. Twenty-three years of the Warshaw operation for distal pancreatectomy with preservation of the spleen. Ann Surg. 2011;253:1136–9. https://doi.org/10.1097/SLA.0b013e318212c1e2.
Goh BKP, Chan CY, Lee SY, Chan WH, Cheow PC, Chow PKH, et al. Factors associated with and consequences of open conversion after laparoscopic distal pancreatectomy: initial experience at a single institution. ANZ J Surg. 2017. https://doi.org/10.1111/ans.13661.
Hanna EM, Rozario N, Rupp C, Sindram D, Iannitti DA, Martinie JB. Robotic hepatobiliary and pancreatic surgery: lessons learned and predictors for conversion. Int J Med Robot Comput Assist Surg MRCAS. 2013;9(2):152–9. https://doi.org/10.1002/rcs.1492.
Butturini G, Damoli I, Crepaz L, Malleo G, Marchegiani G, Daskalaki D, et al. A prospective non-randomised single-center study comparing laparoscopic and robotic distal pancreatectomy. Surg Endosc. 2015;29(11):3163–70. https://doi.org/10.1007/s00464-014-4043-3.
Diener MK, Seiler CM, Rossion I, Kleeff J, Glanemann M, Butturini G, et al. Efficacy of stapler versus hand-sewn closure after distal pancreatectomy (DISPACT): a randomised, controlled multicentre trial. Lancet. 2011;377(9776):1514–22. https://doi.org/10.1016/S0140-6736(11)60237-7.
Zhou W, Lv R, Wang X, Mou Y, Cai X, Herr I. Stapler vs suture closure of pancreatic remnant after distal pancreatectomy: a meta-analysis. Am J Surg. 2009;200(4):529–36. https://doi.org/10.1016/j.amjsurg.2009.12.022.
Probst P, Huttner FJ, Klaiber U, Knebel P, Ulrich A, Buchler MW, et al. Stapler versus scalpel resection followed by hand-sewn closure of the pancreatic remnant for distal pancreatectomy. Cochrane Database Syst Rev. 2015;11:Cd008688.
Hüttner FJ, Koessler-Ebs J, Hackert T, Ulrich A, Büchler MW, Diener MK. Meta-analysis of surgical outcome after enucleation versus standard resection for pancreatic neoplasms. Br J Surg. 2015;102(9):1026–36. https://doi.org/10.1002/bjs.9819.
Jin JB, Qin K, Li H, Wu ZC, Zhan Q, Deng XX, et al. Robotic enucleation for benign or borderline tumours of the pancreas: a retrospective analysis and comparison from a high-volume centre in Asia. World J Surg. 2016;40(12):3009–200. https://doi.org/10.1007/s00268-016-3655-2.
Tian F, Hong XF, Wu WM, Han XL, Wang MY, Cong L, et al. Propensity score-matched analysis of robotic versus open surgical enucleation for small pancreatic neuroendocrine tumours. Br J Surg. 2016;103(10):1358–64. https://doi.org/10.1002/bjs.10220.
Zhang RC, Zhou YC, Mou YP, Huang CJ, Jin WW, Yan JF, et al. Laparoscopic versus open enucleation for pancreatic neoplasms: clinical outcomes and pancreatic function analysis. Surg Endosc. 2016;30(7):2657–65. https://doi.org/10.1007/s00464-015-4538-6.
Belfiori G, Wiese D, Partelli S, Wächter S, Maurer E, Crippa S, et al. Minimally invasive versus open treatment for benign sporadic insulinoma comparison of short-term and long-term outcomes. World J Surg. 2018;42(10):3223–300. https://doi.org/10.1007/s00268-018-4628-4.
Drymousis P, Raptis DA, Spalding D, Fernandez-Cruz L, Menon D, et al. Laparoscopic versus open pancreas resection for pancreatic neuroendocrine tumours: a systematic review and meta-analysis. Hpb. 2014;16(5):397–406. https://doi.org/10.1111/hpb.12162.
Heeger K, Falconi M, Partelli S, Waldmann J, Crippa S, Fendrich V, et al. Increased rate of clinically relevant pancreatic fistula after deep enucleation of small pancreatic tumors. Langenbeck’s Arch Surg. 2014;399(3):315–21. https://doi.org/10.1007/s00423-014-1171-0.
Beger HG. Benign tumors of the pancreas—radical surgery versus parenchyma-sparing local resection—the challenge facing surgeons. J Gastrointest Surg. 2018. https://doi.org/10.1007/s11605-017-3644-2.
Fernández-Cruz L, Molina V, Vallejos R, Jiménez Chavarria E, Lõpez-Boado MA, et al. Outcome after laparoscopic enucleation for non-functional neuroendocrine pancreatic tumours. Hpb. 2012;14(3):171–6. https://doi.org/10.1111/j.1477-2574.2011.00422.x.
Falconi M, Zerbi A, Crippa S, Balzano G, Boninsegna L, et al. Parenchyma preserving resections for small nonfunctioning pancreatic endocrine tumors. Ann Surg Oncol. 2010;17:1621–7. https://doi.org/10.1245/s10434-010-0949-8.
Zhou Y, Zhao M, Wu L, Ye F, Si X. Short- and long-term outcomes after enucleation of pancreatic tumors: an evidence-based assessment. Pancreatology. 2016;16(6):1092–8. https://doi.org/10.1016/j.pan.2016.07.006.
Su AP, Ke NW, Zhang Y, Liu XB, Hu WM, et al. Is laparoscopic approach for pancreatic insulinomas safe? Results of a systematic review and meta-analysis. J Surg Res. 2014;186(1):126–34. https://doi.org/10.1016/j.jss.2013.07.051.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Najafi, N., Mintziras, I., Wiese, D. et al. A retrospective comparison of robotic versus laparoscopic distal resection and enucleation for potentially benign pancreatic neoplasms. Surg Today 50, 872–880 (2020). https://doi.org/10.1007/s00595-020-01966-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-020-01966-z