Abstract
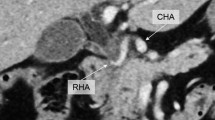
In living donor liver transplantation (LDLT), it is considered safer to reconstruct hepatic arteries (HAs) under a microscope than under conventional loupe magnification, because graft HA stumps are generally thin and short with an average diameter of approximately 2 mm. We first applied microvascular surgical techniques to HA reconstruction for LDLT in 1996. In most cases, we use a disposable double-clip to secure the graft and recipient arteries, and interrupted 8-0 nonabsorbable monofilament sutures. We next started performing resection and reconstruction of the right HA in a surgery for hilar cholangioma using the same technique as in LDLT. Lately, we have started applying microvascular surgical techniques to various digestive surgeries; namely, supercharge and superdrainage in esophageal surgery, vascular reconstruction in free jejunal interposition grafts for cervical esophageal cancer, resection and reconstruction of spontaneous HA aneurysms, jejunal artery reconstruction for spontaneous superior mesenteric artery dissections, and so forth. Mastering this technique is time consuming. However, once a surgeon masters the technique it has almost unlimited applications, and most vital vessels can be safely reconstructed using this method. We herein provide a technical review of the application of microvascular surgical techniques for various digestive surgeries.










Similar content being viewed by others
References
Petrie NC, Chan JK, Chave H, McGuiness CN. The inferior mesenteric vessels as recipients when performing free tissue transfer for pelvic defects following abdomino-perineal resection. A novel technique and review of intra-peritoneal recipient vessel options for microvascular transfer. J Plast Reconstr Aesthet Surg. 2010;63:2133–40.
Cusano A, Fernandes R. Technology in microvascular surgery. Oral Maxillofac Surg Clin N Am. 2010;22:73–90.
Saito A, Sawaizumi M, Imai T, Matsumoto S. Continuous local intraarterial infusion of anticoagulants for microvascular free tissue transfer in primary reconstruction of the lower limb following resection of sarcoma. Microsurgery. 2010;30:376–9.
Chernichenko N, Ross DA, Shin J, Sasaki CT, Ariyan S. End-to-side venous anastomosis with an anastomotic coupling device for microvascular free-tissue transfer in head and neck reconstruction. Laryngoscope. 2008;118:2146–50.
Ross DA, Chow JY, Shin J, Restifo R, Joe JK, Sasaki CT, et al. Arterial coupling for microvascular free tissue transfer in head and neck reconstruction. Arch Otolaryngol Head Neck Surg. 2005;131:891–5.
Uchiyama H, Hashimoto K, Hiroshige S, Harada N, Soejima Y, Nishizaki T, et al. Hepatic artery reconstruction in living-donor liver transplantation: a review of its techniques and complications. Surgery. 2002;131:S200–4.
Harashina T. Use of the untied suture in microvascular anastomoses. Plast Reconstr Surg. 1977;59:134–5.
Miyagi S, Enomoto Y, Sekiguchi S, Kawagishi N, Sato A, Fujimori K, et al. Microsurgical back wall support suture technique with double needle sutures on hepatic artery reconstruction in living donor liver transplantation. Transplant Proc. 2008;40:2521–2.
Harashina T. Use of a continuous suture for back wall repair of end-to-end or end-to-side anastomoses. Plast Reconstr Surg. 1982;69:139–44.
Settmacher U, Stange B, Haase R, Heise M, Steinmüller T, Bechstein WO, et al. Arterial complications after liver transplantation. Transpl Int. 2000;13:372–8.
Yanaga K, Lebeau G, Marsh JW, Gordon RD, Makowka L, Tzakis AG, et al. Hepatic artery reconstruction for hepatic artery thrombosis after orthotopic liver transplantation. Arch Surg. 1990;125:628–31.
Inomoto T, Nishizawa F, Sasaki H, Terajima H, Shirakata Y, Miyamoto S, et al. Experiences of 120 microsurgical reconstructions of hepatic artery in living related liver transplantation. Surgery. 1996;119:20–6.
Mori K, Nagata I, Yamagata S, Sasaki H, Nishizawa F, Takada Y, et al. The introduction of microvascular surgery to hepatic artery reconstruction in living-donor liver transplantation—its surgical advantages compared with conventional procedures. Transplantation. 1992;54:263–8.
Kodama Y, Sakuhara Y, Abo D, Shimamura T, Furukawa H, Todo S, et al. Percutaneous transluminal angioplasty for hepatic artery stenosis after living donor liver transplantation. Liver Transplant. 2006;12:465–9.
Maleux G, Pirenne J, Aerts R, Nevens F. Hepatic artery pseudoaneurysm after liver transplantation: definitive treatment with a stent-graft after failed coil embolisation. Br J Radiol. 2005;78:453–6.
Fistouris J, Herlenius G, Bäckman L, Olausson M, Rizell M, Mjörnstedt L, et al. Pseudoaneurysm of the hepatic artery following liver transplantation. Transplant Proc. 2006;38:2679–82.
Plengvanit U, Chearanai O, Sindhvananda K, Dambrongsak D, Tuchinda S, Viranuvatti V. Collateral arterial blood supply of the liver after hepatic artery ligation, angiographic study of twenty patients. Ann Surg. 1972;175:105–10.
Ikegami T, Kawasaki S, Matsunami H, Hashikura Y, Nakazawa Y, Miyagawa S, et al. Should all hepatic arterial branches be reconstructed in living-related liver transplantation? Surgery. 1996;119:431–6.
Kubota K, Makuuchi M, Takayama T, Harihara Y, Hasegawa K, Aoki T, et al. Simple test on the back table for justifying single hepatic-arterial reconstruction in living related liver transplantation. Transplantation. 2000;70:696–7.
Yanaga K, Tzakis AG, Starzl TE. Partial dearterialization of the liver allograft. Transpl Int. 1990;3:185–8.
Uchiyama H, Harada N, Sanefuji K, Kayashima H, Taketomi A, Soejima Y, et al. Dual hepatic artery reconstruction in living donor liver transplantation using a hepatic graft with 2 hepatic arterial stumps. Surgery. 2010;147:878–86.
Suehiro T, Ninomiya M, Shiotani S, Hiroshige S, Harada N, Minagawa R, et al. Hepatic artery reconstruction and biliary stricture formation after living donor adult liver transplantation using the left lobe. Liver Transplant. 2002;8:495–9.
Uchiyama H, Ikegami T, Soejima Y, Ninomiya M, Kayashima H, Taketomi A, et al. Use of recipient’s left hepatic artery for artery reconstruction in right lobe living donor liver transplantation with duct-to-duct anastomosis. Transplantation. 2010;89:1016–21.
Uchiyama H, Shirabe K, Taketomi A, Soejima Y, Ninomiya M, Kayashima H, et al. Extra-anatomical hepatic artery reconstruction in living donor liver transplantation: can this procedure save hepatic grafts? Liver Transplant. 2010;16:1054–61.
Yang Y, Yan LN, Zhao JC, Ma YK, Huang B, Li B, et al. Microsurgical reconstruction of hepatic artery in A-A LDLT: 124 consecutive cases without HAT. World J Gastroenterol. 2010;16:2682–8.
Margreiter C, Aigner F, Orozco H, Wechselberger G, Ollinger R, Bösmüller C, et al. Hepatic artery reconstruction with inferior mesenteric vein graft in pediatric living donor liver transplantation. Pediatr Transplant. 2008;12:324–8.
Uchiyama H, Soejima Y, Taketomi A, Yoshizumi T, Harada N, Ijichi H, et al. Hepatic artery aneurysm arising from an interposition vein graft four years after auxiliary partial orthotopic liver transplantation. Transpl Int. 2007;20:197–200.
Morita M, Yoshida R, Ikeda K, Egashira A, Oki E, Sadanaga N, et al. Advances in esophageal cancer surgery in Japan: an analysis of 1000 consecutive patients treated at a single institute. Surgery. 2008;143:499–508.
Cerfolio RJ, Allen MS, Deschamps C, Trastek VF, Pairolero PC. Esophageal replacement by colon interposition. Ann Thorac Surg. 1995;59:1382–4.
Davis PA, Law S, Wong J. Colonic interposition after esophagectomy for cancer. Arch Surg. 2003;138:303–8.
Kono K, Sugai H, Omata H, Fujii H. Transient bloodletting of the short gastric vein in the reconstructed gastric tube improves gastric microcirculation during esophagectomy. World J Surg. 2007;31:780–4.
Uchiyama H, Morita M, Toh Y, Saeki H, Kakeji Y, Matsuura H, et al. Superdrainage of the ileocolic vein to the internal jugular vein interposed by an inferior mesenteric vein graft in replacing the esophagus with the right hemicolon. Surg Today. 2010;40:578–82.
Bradford CR, Esclamado RM, Carroll WR. Monitoring of revascularized jejunal autografts. Arch Otolaryngol Head Neck Surg. 1992;118:1042–4.
Seidenberg B, Rosenak SS, Hurwitt ES, Som ML. Immediate reconstruction of the cervical esophagus by a revascularized isolated jejunal segment. Ann Surg. 1959;149:162–71.
Sarukawa S, Asato H, Okazaki M, Nakatsuka T, Takushima A, Harii K. Clinical evaluation and morbidity of 201 free jejunal transfers for oesophagopharyngeal reconstruction during the 20 years 1984–2003. Scand J Plast Reconstr Surg Hand Surg. 2006;40:148–52.
Shirakawa Y, Naomoto Y, Noma K, Ono R, Nobuhisa T, Kobayashi M, et al. Free jejunal graft for hypopharyngeal and esophageal reconstruction. Langenbecks Arch Surg. 2004;389:387–90.
Hemming AW, Reed AI, Fujita S, Foley DP, Howard RJ. Surgical management of hilar cholangiocarcinoma. Ann Surg. 2005;241:693–9.
Miyazaki M, Kato A, Ito H, Kimura F, Shimizu H, Ohtsuka M, et al. Combined vascular resection in operative resection for hilar cholangiocarcinoma: does it work or not? Surgery. 2007;141:581–8.
Nyui S, Inoue S, Sato T, Nakase A. Surgical treatment of a huge hepatic artery aneurysm—a case report. Jpn J Surg. 1991;21:344–7.
Schroeyers P, Lismonde M, Vermonden J, Six C. Management of hepatic artery aneurysm. Case report and literature review. Acta Chir Belg. 1995;95:89–91.
Countryman D, Norwood S, Register D, Torma M, Andrassy R. Hepatic artery aneurysm. Report of an unusual case and review of the literature. Am Surg. 1983;49:51–4.
Akiyama H, Miyazono H, Tsurumaru M, Hashimoto C, Kawamura T. Use of the stomach as an esophageal substitute. Ann Surg. 1978;188:606–10.
Nagai T, Torishima R, Uchida A, Nakashima H, Takahashi K, Okawara H, et al. Spontaneous dissection of the superior mesenteric artery in four cases treated with anticoagulation therapy. Intern Med. 2004;43:473–8.
Takayama H, Takeda S, Saitoh SK, Hayashi H, Takano T, Tanaka K. Spontaneous isolated dissection of the superior mesenteric artery. Intern Med. 2002;41:713–6.
Lamprecht G, Trabold T, Gregor M, Lamberts R. Spontaneous, self-limited, non-atherosclerotic dissection of the superior mesenteric artery. Eur J Gastroenterol Hepatol. 2003;15:437–9.
Oda T, Ono H, Muranaka H, Takai F. The right gastroepiploic artery as an alternative inflow source in acute mesenteric ischemia. J Vasc Surg. 2005;41:1061–4.
Picquet J, Abilez O, Pénard J, Jousset Y, Rousselet MC, Enon B. Superficial femoral artery transposition repair for isolated superior mesenteric artery dissection. J Vasc Surg. 2005;42:788–91.
Casella IB, Bosch MA, Sousa WO Jr. Isolated spontaneous dissection of the superior mesenteric artery treated by percutaneous stent placement: case report. J Vasc Surg. 2008;47:197–200.
Miyamoto N, Sakurai Y, Hirokami M, Takahashi K, Nishimori H, Tsuji K, et al. Endovascular stent placement for isolated spontaneous dissection of the superior mesenteric artery: report of a case. Radiat Med. 2005;23:520–4.
Yoon YW, Choi D, Cho SY, Lee DY. Successful treatment of isolated spontaneous superior mesenteric artery dissection with stent placement. Cardiovasc Interv Radiol. 2003;26:475–8.
Leung DA, Schneider E, Kubik-Huch R, Marincek B, Pfammatter T. Acute mesenteric ischemia caused by spontaneous isolated dissection of the superior mesenteric artery: treatment by percutaneous stent placement. Eur Radiol. 2000;10:1916–9.
Conflict of interest
The authors have no conflict of interest with regard to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uchiyama, H., Shirabe, K., Morita, M. et al. Expanding the applications of microvascular surgical techniques to digestive surgeries: a technical review. Surg Today 42, 111–120 (2012). https://doi.org/10.1007/s00595-011-0032-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-011-0032-5