Abstract
Purpose
The use of electrocautery for tissue dissection is becoming increasingly popular, despite the associated risk of poor wound healing and excessive scarring. We conducted this study to compare the wound complications and early and late clinical results resulting from electrocautery versus the scalpel to create a cutaneous flap during thyroidectomy.
Methods
The subjects of this study were 100 patients, randomized prospectively to either a scalpel group (group S, n = 50) or an electrocautery group (group E, n = 50).
Results
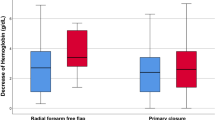
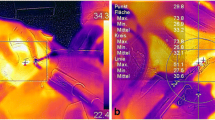
Thickness of tissue damage, postoperative thickness of the flap, discomfort in the neck 7 days after surgery, and hypoesthesia and paresthesia in the neck 3 months after surgery were significantly higher in group E than in group S. There were no significant differences in overall postoperative wound complications, postoperative pain, satisfaction with the cosmetic result, or overall outcome of the operation between the groups. Although the incidence of seroma was higher in group E (20%) than in group S (8%), the difference was not significant.
Conclusion
Although electrocautery was associated with increased histological tissue damage, postoperative flap edema, discomfort, and other complications in the early stage, the clinical and cosmetic results of flaps made using electrocautery or a scalpel were similar and satisfactory 6 months after surgery.
Similar content being viewed by others
References
Miccoli P, Minuto MN, Ugolini C, Pisano R, Fosso A, Berti P. Minimally invasive video-assisted thyroidectomy for benign thyroid disease: an evidence-based review. World J Surg 2008;32:1333–1340.
Ruggieri M, Zullino A, Straniero A, Maiuolo A, Fumarola A, Vietri F, et al. Is minimally invasive surgery appropriate for small differentiated thyroid carcinomas? Surg Today 2010;40:418–422.
Miccoli P, Berti P, Frustaci GL, Ambrosini CE, Materazzi G. Video-assisted thyroidectomy: indications and results. Langenbecks Arch Surg 2006;391:68–71.
Lombardi CP, Raffaelli M, Princi P, De Crea C, Bellantone R. Video-assisted thyroidectomy: report on the experience of a single center in more than four hundred cases. World J Surg 2006;30:794–800.
Terris DJ, Seybt MW, Elchoufi M, Chin E. Cosmetic thyroid surgery: defining the essential principles. Laryngoscope 2007;117:1168–1172.
Chrysos E, Athanasakis E, Antonakakis S, Xynos E, Zoras O. A prospective study comparing diathermy and scalpel incisions in tension-free inguinal hernioplasty. Am Surg 2005;71:326–329.
Yamamoto D, Yamada M, Okugawa H, Yonekura Y, Tanaka K. A comparison between electrocautery and scalpel plus scissor in breast conserving surgery. Oncol Rep 2003;10:1729–1732.
Groot G, Chappell EW. Electrocautery used to create incisions does not increase wound infection rates. Am J Surg 1994;167:601–603.
Barbaros U, Erbil Y, Aksakal N, Citlak G, Isever H, Bozbora A, et al. Electrocautery for cutaneous flap creation during thyroidectomy: a randomised, controlled study. J Laryngol Otol 2008;122:1343–1348.
Porter KA, O’Connor S, Rimm E, Lopez M. Electrocautery as a factor in seroma formation following mastectomy. Am J Surg 1998;176:8–11.
Sheen-Chen SM, Chou FF. A comparison between scalpel and electrocautery in modified radical mastectomy. Eur J Surg 1993;159:457–459.
Kearns SR, Connolly EM, McNally S, McNamara DA, Deasy J. Randomized clinical trial of diathermy versus scalpel incision in elective midline laparotomy. Br J Surg 2001;88:41–44.
Gelman CL, Barroso EG, Britton CT, Haklin MF, Staren ED. The effect of lasers, electrocautery, and sharp dissection on cutaneous flaps. Plast Reconstr Surg 1994;94:829–833.
Liboon J, Funkhouser W, Terris DJ. A comparison of mucosal incisions made by scalpel, CO2 laser, electrocautery, and constant-voltage electrocautery. Otolaryngol Head Neck Surg 1997;116:379–385.
Reeve T, Thompson NW. Complications of thyroid surgery: how to avoid them, how to manage them, and observations on their possible effect on the whole patient. World J Surg 2000;24:971–975.
Rosato L, Avenia N, Bernante P, De Palma M, Gulino G, Nasi PG, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg 2004;28:271–276.
Thomusch O, Machens A, Sekulla C, Ukkat J, Lippert H, Gastinger I, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg 2000;24:1335–1341.
Lennard TWJ. Complications of thyroid surgery. In: Mazzaferri EL, Harmer C, Mallick UK, Kendall-Taylor P, editors. Practical management of thyroid cancer. 1st ed. London: Springer; 2006. p. 165–170.
Sanders LE, Rossi RL, Cady B. Surgical complications and their treatment. In: Cady B, Rossi RL, editors. Surgery of the thyroid and parathyroid glands. 3rd ed. Philadelphia: Saunders International; 1991. p. 326–336.
Schwabegger A, Ninkovic M, Brenner E, Anderl H. Seroma as a common donor site morbidity after harvesting the latissimus dorsi flap: observations on cause and prevention. Ann Plast Surg 1997;38:594–597.
Bellantone R, Lombardi CP, Bossola M, Boscherini M, De Crea C, Alesina PF, et al. Video-assisted vs conventional thyroid lobectomy: a randomized trial. Arch Surg 2002;137:301–304.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarwis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999:20:250–278.
Ikeda Y, Takami H, Sasaki Y, Takayama J, Niimi M, Kan S. Clinical benefits in endoscopic thyroidectomy by the axillary approach. J Am Coll Surg 2003;196:189–195.
Arends MJ, Wyllie AH. Apoptosis: mechanisms and roles in pathology. Int Rev Exp Pathol 1991;32:223–254.
Fukuda Y, Ito Y, Azumi H, Eid NA, Li ZL, Marumo M, et al. Cell death and proliferation in Nd-YAG laser, electrocautery, and scalpel wounds on mice skin. J Dermatol Sci 2002;28:106–118.
Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP. Morbidity of thyroid surgery. Am J Surg 1998;176:71–75.
Dionigi G, Rovera F, Boni L, Castano P, Dionigi R. Surgical site infections after thyroidectomy. Surg Infect (Larchmt) 2006;7suppl 2:117–120.
Dionigi G, Rovera F, Boni L, Dionigi R. Surveillance of surgical site infections after thyroidectomy in a one-day surgery setting. Int J Surg 2008;6suppl 1:s13–s15.
Ozlem N, Ozdogan M, Gurer A, Gomceli I, Aydin R. Should the thyroid bed be drained after thyroidectomy? Langenbecks Arch Surg 2006;391:228–230.
Ayyash K, Khammash M, Tibblin S. Drain vs. no drain in primary thyroid and parathyroid surgery. Eur J Surg 1991;157:113–114.
Samraj K, Gurusamy KS. Wound drains following thyroid surgery. Cochrane Database Syst Rev 2007;17:CD006099.
Graney DO. Anatomy. In: Cummings CW, Fredrickson JM, Harker LA, Krause CJ, Schuller DE, editors. Otolaryngology — head and neck surgery. 1st ed. St. Louis: Mosby; 1986. p. 1573–1586.
O’Connell DA, Diamond C, Seikaly H, Harris JR. Objective and subjective scar aesthetics in minimal access vs conventional access parathyroidectomy and thyroidectomy surgical procedures: a paired cohort study. Arch Otolaryngol Head Neck Surg 2008;134:85–93.
Böhm B, Minner S, Engelhardt T, Rödiger H. Long-term cosmetic results following thyroid resection. Chirurg 2005;76:54–57.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Uludag, M., Yetkin, G., Ozel, A. et al. Wound complications and clinical results of electrocautery versus a scalpel to create a cutaneous flap in thyroidectomy: A prospective randomized trial. Surg Today 41, 1041–1048 (2011). https://doi.org/10.1007/s00595-010-4435-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-010-4435-5