Abstract
Aims
Data are limited regarding how shift work is linked to the development of type 2 diabetes, especially among workers at high risk of diabetes. We examined the risk of diabetes according to shift-work conditions over several years among Japanese adults.
Methods
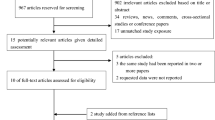
This prospective study enrolled 17,515 workers (age 40–78 years). Shift work was self-reported at annual health examinations over time from 2004 to 2017 and categorized as shift workers or non-shift workers. Diabetes was defined as fasting plasma glucose, random glucose, HbA1c, and self-reported use of antidiabetic medications. The association of shift work and diabetes was quantified using Cox regression.
Results
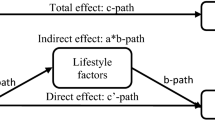
During a follow-up of 8.1 years in median, 2071 incident cases of diabetes were documented. Compared with non-shift work, shift work showed a significantly elevated hazard ratios of developing diabetes. Shift work showed a 19% (95% confidence intervals: 3–37%) higher hazard ratios for diabetes, after adjustment for demographic-, cardiometabolic-, and work-related factors. Further adjustment for lifestyle factors and body mass index did not materially change this association (a 16% increase; 95% confidence intervals, 1–34%). This relationship was replicated among workers with prediabetes.
Conclusions
Engaging in shift work may increase the risk of developing diabetes independently of lifestyle factors and body mass index, even among prediabetic workers.
Similar content being viewed by others
References
Boivin DB, Boudreau P (2014) Impacts of shift work on sleep and circadian rhythms. Pathol Biol Paris 62:292–301
Kubo T (2014) Estimate of the number of night shift workers in Japan. J UOEH 36:273–276
Wefers J, van Moorsel D, Hansen J et al (2018) Circadian misalignment induces fatty acid metabolism gene profiles and compromises insulin sensitivity in human skeletal muscle. Proc Natl Acad Sci U S A 115:7789–7794
Sallinen M, Kecklund G (2010) Shift work, sleep, and sleepiness–differences between shift schedules and systems. Scand J Work Environ Health 36:121–133
Guerrero-Vargas NN, Espitia-Bautista E, Buijs RM, Escobar C (2018) Shift-work: is time of eating determining metabolic health? Evidence from animal models. Proc Nutr Soc 77:199–215
Kivimaki M, Batty GD, Hublin C (2011) Shift work as a risk factor for future type 2 diabetes: evidence, mechanisms, implications, and future research directions. PLoS Med 8:e1001138
Sowah D, Fan X, Dennett L, Hagtvedt R, Straube S (2017) Vitamin D levels and deficiency with different occupations: a systematic review. BMC Public Health 17:519
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA (2010) Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 33:414–420
Mitri J, Muraru MD, Pittas AG (2011) Vitamin D and type 2 diabetes: a systematic review. Eur J Clin Nutr 65:1005–1015
Smith AD, Crippa A, Woodcock J, Brage S (2016) Physical activity and incident type 2 diabetes mellitus: a systematic review and dose-response meta-analysis of prospective cohort studies. Diabetologia 59:2527–2545
Gan Y, Yang C, Tong X et al (2015) Shift work and diabetes mellitus: a meta-analysis of observational studies. Occup Environ Med 72:72–78
Karlsson B, Alfredsson L, Knutsson A, Andersson E, Toren K (2005) Total mortality and cause-specific mortality of Swedish shift- and dayworkers in the pulp and paper industry in 1952–2001. Scand J Work Environ Health 31:30–35
De Bacquer D, Van Risseghem M, Clays E, Kittel F, De Backer G, Braeckman L (2009) Rotating shift work and the metabolic syndrome: a prospective study. Int J Epidemiol 38:848–854
Kawakami N, Araki S, Takatsuka N, Shimizu H, Ishibashi H (1999) Overtime, psychosocial working conditions, and occurrence of non-insulin dependent diabetes mellitus in Japanese men. J Epidemiol Community Health 53:359–363
Suwazono Y, Sakata K, Okubo Y et al (2006) Long-term longitudinal study on the relationship between alternating shift work and the onset of diabetes mellitus in male Japanese workers. J Occup Environ Med 48:455–461
Eriksson AK, van den Donk M, Hilding A, Ostenson CG (2013) Work stress, sense of coherence, and risk of type 2 diabetes in a prospective study of middle-aged Swedish men and women. Diabetes Care 36:2683–2689
Hansen AB, Stayner L, Hansen J, Andersen ZJ (2016) Night shift work and incidence of diabetes in the danish nurse cohort. Occup Environ Med 73:262–268
Shan Z, Li Y, Zong G et al (2018) Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: results from two large US cohorts of female nurses. BMJ 363:k4641
Morikawa Y, Nakagawa H, Miura K et al (2005) Shift work and the risk of diabetes mellitus among Japanese male factory workers. Scand J Work Environ Health 31:179–183
Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M (2012) Prediabetes: a high-risk state for diabetes development. Lancet 379:2279–2290
NCD Risk Factor Collaboration (2016) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 387:1513–30
Kuwahara K, Honda T, Nakagawa T et al (2015) Associations of leisure-time, occupational, and commuting physical activity with risk of depressive symptoms among Japanese workers: a cohort study. Int J Behav Nutr Phys Act 12:119
Honda T, Kuwahara K, Nakagawa T, Yamamoto S, Hayashi T, Mizoue T (2015) Leisure-time, occupational, and commuting physical activity and risk of type 2 diabetes in Japanese workers: a cohort study. BMC Public Health 15:1004
Hu H, Nakagawa T, Honda T et al (2019) Low serum creatinine and risk of diabetes: the Japan Epidemiology Collaboration on Occupational Health Study. J Diabetes Investig 10(5):1209–1214
American Diabetes Association (2019) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care 42:S13–S28
Zoto E, Cenko F, Doci P, Rizza S (2019) Effect of night shift work on risk of diabetes in healthy nurses in Albania. Acta Diabetol 56:811–813
Acknowledgements
We acknowledge scientific advice for implementing J-ECOH Study from Dr Toshiteru Okubo (National Institute of Occupational Safety and Health, Japan), implementation of data management from Ms Maki Konishi (National Center for Global Health and Medicine), and support for administrative issues from Ms Rika Osawa (National Center for Global Health and Medicine).
Funding
This study was supported in part by the Industrial Health Foundation and a grant from National Center for Global Health and Medicine (28-Shi-1206).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. T. Nakagawa, S. Yamamoto, and T. Honda are occupational physicians in the participating company.
Ethical standards
The ethical approval of the study protocol was obtained at National Center for Global Health and Medicine.
Informed consent
Before obtaining data, announcement about the conduct of the J-ECOH Study was implemented using posters. Participants were not required to provide any informed consent for participation. However, they were allowed at any time to refuse the participation.
Additional information
Managed by Massimo Federici.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Osaki, Y., Kuwahara, K., Hu, H. et al. Shift work and the onset of type 2 diabetes: results from a large-scale cohort among Japanese workers. Acta Diabetol 58, 1659–1664 (2021). https://doi.org/10.1007/s00592-021-01770-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-021-01770-2