Abstract
Aims
Diabetes mellitus (DM) is one of the main risk factors for intracranial cerebral artery stenosis (ICAS), and fasting blood glucose (FBG) might be an effective predictor of ICAS. However, there are a few studies revealing the relationship between FBG and ICAS. We aim to identify the association between FBG and ICAS in Koreans.
Methods
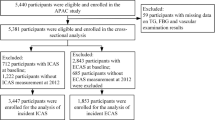
This was a secondary study based on a cross-sectional study. A total of 1011 Korean individuals who were asymptomatic but with high cerebrovascular risk underwent an examination in a Korean medical centre from March 2008 to December 2014. The main measure was FBG, while the main outcome was ICAS. Multivariate logistic regression analyses of FBG in the presence of ICAS were performed to examine the potential association. The author used the data provided by the paper “Association between Serum Alkaline Phosphatase Level and Cerebral Small Vessel Disease” for secondary analysis.
Results
The average age of the participants was 64.2 ± 9.1 years old, and approximately 35% of them were males. There were 24 participants suffering from ICAS in the first FBG tertile (< 5.4 mmol/L), while there were 26 in the second tertile (5.4–7.1 mmol/L) and 50 in the third tertile (≥ 7.1 mmol/L). The non-adjusted relationship between FBG and ICAS was positive. After controlling potential confounders, the association of FPG with ICAS remained positive, as well as in subgroups analysis, such as age, sex, hypertension, diabetes mellitus, hyperlipidaemia and COAD. The association remained unchanged after adjusted sex, age, hypertension, DM, uric acid, hyperlipidaemia, and CAOD (OR = 1.08, 95% CI = 1.02–1.15). The analyses also showed that the positive association was statistically significant (P < 0.05) among individuals without diabetes.
Conclusions
This study showed a positive relationship between FBG and ICAS, which suggests that clinicians may need to be simultaneously concerned about FBG and ICAS.

Similar content being viewed by others
Availability of data and materials
Data can be obtained from appendix of the paper published in the PLOS ONE journal.
Abbreviations
- CAOD:
-
Coronary artery occlusive disease
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- WBCs:
-
White blood cells
- eGFR:
-
Estimated glomerular filtration rate
- GOT:
-
Glutamic oxaloacetic transaminase
- GPT:
-
Glutamic pyruvic transaminase
- ALP:
-
Alkaline phosphatase
- SLI:
-
Silent lacunar infarct
- MS-cWMH:
-
Moderate-to-severe cerebral white matter hyperintensities
- LCAS:
-
Large cerebral arterial stenosis
- ECAS:
-
Extracranial arterial stenosis
- ICAS:
-
Intracranial arterial stenosis
References
Wang J, Wang Y, Chai Z et al (2018) Stenosis length of middle cerebral artery and branch atheromatous disease associated infarct. Int J Neurosci 128:133–139. https://doi.org/10.1080/00207454.2017.1377710
Ju K, Zhong L, Ni X et al (2018) Cerebral vasomotor reactivity predicts the development of acute stroke in patients with internal carotid artery stenosis. Neurol Neurochirurgia Polska 52:374–378. https://doi.org/10.1016/j.pjnns.2017.12.015
Moossy J (1966) Cerebral infarction and intracranial arterial thrombosis. Necropsy studies and clinical implications. Arch Neurol 14:119–123. https://doi.org/10.1001/archneur.1966.00470080003001
Kolominsky-Rabas PL, Weber M, Gefeller O et al (2001) Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke 32:2735–2740. https://doi.org/10.1161/hs1201.100209
Chimowitz MI, Lynn MJ, Howlett-Smith H et al (2006) Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. Curr Cardiol Reports 8:7
Wityk RJ, Lehman D, Klag M et al (1996) Race and sex differences in the distribution of cerebral atherosclerosis. Stroke 27:1974–1980. https://doi.org/10.1161/01.str.27.11.1974
Wong KS, Li H, Lain M et al (2002) Progression of middle cerebral artery occlusive disease and its relationship with further vascular events after stroke. Stroke 33:532.
Weber R, Kraywinkel K, Diener HC et al (2010) Symptomatic intracranial atherosclerotic stenoses: prevalence and prognosis in patients with acute cerebral ischemia. Cerebrovasc Dis 30:188–193.
Luchowski P, Wojczal J, Buraczynska K et al (2015) Predictors of intracranial cerebral artery stenosis in patients before cardiac surgery and its impact on perioperative and long-term stroke risk. Neurol Neurochir Pol 49:395–400. https://doi.org/10.1016/j.pjnns.2015.09.006
Elhfnawy AM, Volkmann J, Schliesser M (2019) Are cerebral white matter lesions related to the presence of bilateral internal carotid artery stenosis or to the length of stenosis among patients with ischemic cerebrovascular events? Front Neurol 10:919. https://doi.org/10.3389/fneur.2019.00919
Zhang Q, Zhao G, Yang N (2019) Fasting blood glucose levels in patients with different types of diseases. Prog Mol Biol Transl Sci 162:277–292. https://doi.org/10.1016/bs.pmbts.2019.01.004
Lee HB, Kim J, Kim SH, Kim S, Kim OJ, Oh SH (2015) Association between serum alkaline phosphatase level and cerebral small vessel disease. PLoS ONE 10(11):e0143355. https://doi.org/10.1371/journal.pone.0143355
Park SY, An SA, Lee HB et al (2013) Different impact of hyperhomocysteinemia on cerebral small vessel ischemia and cervico-cerebral atherosclerosis in non-stroke individuals. Thrombosis Res 131(1):e12–e16. https://doi.org/10.1016/j.thromres.2012.11.011. PMID: 23218488
Chimowitz MI, Lynn MJ, Howlett-Smith H et al (2005) Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. New Engl J Med 352(13):1305–1316. PMID: 15800226
Barnett HJ, Taylor DW, Eliasziw M et al (1998) Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 339:1415–1425. https://doi.org/10.1056/NEJM199811123392002
Fazekas F, Chawluk JB, Alavi A et al (1987) MR signal abnormalities at 1.5 T in Alzheimer's dementia and normal aging. Am J Roentgenol 149(2):351–356. PMID:3496763
Leonards CO, Ipsen N, Malzahn U et al (2012) White matter lesion severity in mild acute ischemic stroke patients and functional outcome after 1 year. Stroke J Cerebral Circulation 43(11):3046–3051. https://doi.org/10.1161/STROKEAHA.111.646554. PMID: 22935398
K/DOQI clinical practice guidelines for chronic kidney disease evaluation, classification, and stratification. Am J Kidney Dis 39:S1–S266 (2002)
Lam TD, Lammers S, Munoz C et al (2013) Diabetes, intracranial stenosis and microemboli in asymptomatic carotid stenosis. Can J Neurol Sci 40:177–181
Holmstedt CA, Turan TN (2013) Atherosclerotic intracranial arterial stenosis: risk factors, diagnosis, and treatment. Lancet Neurol 12(11):1106–1114. https://doi.org/10.1016/S1474-4422(13)70195-9
Zhai FF, Yan S, Li ML et al (2018) Intracranial arterial dolichoectasia and stenosis: risk factors and relation to cerebral small vessel disease. Stroke J Cerebral Circulation 49(5):1135–1140. https://doi.org/10.1161/STROKEAHA.117.020130
Shitara S, Fujiyoshi A, Hisamatsu T et al (2019) Intracranial artery stenosis and its association with conventional risk factors in a general population of Japanese Men. Stroke J Cerebral Circulation 50(10):2967–2969. https://doi.org/10.1161/STROKEAHA.119.025964
Nissen SE, Nicholls SJ, Sipahi I et al (2006) Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA 295(13):1556–1565. https://doi.org/10.1001/jama.295.13.jpc60002
Triggle CR, Ding H (2017) Metformin is not just an antihyperglycaemic drug but also has protective effects on the vascular endothelium. Acta Physiol (Oxf) 219:138–151
Li J, Benashski SE, Venna VR et al (2010) Effects of metformin in experimental stroke. Stroke 41(11):2645–2652. https://doi.org/10.1161/STROKEAHA.110.589697
Jia J, Cheng J, Ni J et al (2015) Neuropharmacological actions of Metformin in stroke. Curr Neuropharmacol 13(3):389–394. https://doi.org/10.2174/1570159x13666150205143555
Li AC, Brown KK, Silvestre MJ et al (2000) Peroxisome proliferator-activated receptor gamma ligands inhibit development of atherosclerosis in LDL receptor-deficient mice. J Clin Invest 106(4):523–531. https://doi.org/10.1172/JCI10370
Calkin AC, Forbes JM, Smith CM et al (2005) Rosiglitazone attenuates atherosclerosis in a model of insulin insufficiency independent of its metabolic effects. Arterioscler Thromb Vasc Biol 25(9):1903–1909. https://doi.org/10.1161/01.ATV.0000177813.99577.6b
Lim S, Lee KS, Lee JE et al (2015) Effect of a new PPAR-gamma agonist, lobeglitazone, on neointimal formation after balloon injury in rats and the development of atherosclerosis. Atherosclerosis 243(1):107–119. https://doi.org/10.1016/j.atherosclerosis.2015.08.037
Kernan WN, Viscoli CM, Furie KL et al (2016) Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med 374(14):1321–1331. https://doi.org/10.1056/NEJMoa1506930
Gaspari T, Liu H, Welungoda I et al (2011) A GLP-1 receptor agonist liraglutide inhibits endothelial cell dysfunction and vascular adhesion molecule expression in an ApoE-/- mouse model [published correction appears in Diab Vasc Dis Res. 2012 Jan;9(1):79]. Diab Vasc Dis Res 8(2):117–124. https://doi.org/10.1177/1479164111404257.
Sato K, Kameda M, Yasuhara T et al (2013) Neuroprotective effects of liraglutide for stroke model of rats. Int J Mol Sci 14(11):21513–21524. Published 2013 Oct 30. https://doi.org/10.3390/ijms141121513.
Wang J, Wu J, Zhang S (2014) Elevated fasting glucose as a potential predictor for asymptomatic cerebral artery stenosis: a cross-sectional study in Chinese adults. Atherosclerosis 237(2):661–665. https://doi.org/10.1016/j.atherosclerosis.2014.10.083
Heianza Y, Arase Y, Kodama S et al (2015) Fasting glucose and HbA1c levels as risk factors for the development of hypertension in Japanese individuals: Toranomon hospital health management center study 16 (TOPICS 16). J Hum Hypertens 29:254–259. https://doi.org/10.1038/jhh.2014.77
Vandenbroucke JP, von Elm E, Altman DG et al (2014) Strengthening the Reporting of Observational Studies in Epidemiology(STROBE): explanation and elaboration. Int J Surg 12:1500–1524. https://doi.org/10.1016/j.ijsu.2014.07.014
Han Y, Qiao H, Chen S et al (2018) ICASMAP investigators. Brain Behav 8(12):e01154. https://doi.org/10.1002/brb3.1154. Epub 2018 Nov 19. PMID:30456898
Acknowledgements
The authors truly appreciate the researchers for providing the original data from their study. They completed the entire study. They are Han-Bin Lee, Jinkwon Kim, Ok-Joon Kim, Seung-Hun Oh (corresponding author) (Department of Neurology, CHA Bundang Medical Center, CHA University, Seongnam, South Korea), Sang-Heum Kim (Department of Radiology, CHA Bundang Medical Center, CHA University, Seongnam, South Korea), and Soonhag Kim (Institute for Bio-Medical Convergence, College of Medicine, Catholic Kwandong University, Gangneung-si, South Korea).
In addition, we would like to express our gratitude to Nature Springer Author Services due to their languages editing. And we all appreciate Dr. Big Sward, for his help during the manuscript revised time.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
DW and DHX contributed to the drafting of the manuscript. FY contributed to the material preparation and data collection and XN contributed to the analysis and interpretation of the data. DHX and TTY contributed to the study conception and revision of the manuscript, and MXL approved the final version of the submitted manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Consent to participate
Informed consent was obtained from all individuals included in the study conducted by Lee HB et al.
Consent to publish
All participants agreed with the informed consent regarding publishing their data.
Ethics approval
The study from which we obtained our data was approved by the hospital ethics review committee (IRB no.: BD-2010–083). Since this is a retrospective secondary analysis study, according to data protection guidelines, it is unnecessary to obtain formal ethical approval. We consulted extensively with the IRB in the first affiliated hospital of Guangzhou University of Chinese Medicine who determined that our study did not need ethical approval.
Additional information
Managed by Massimo Federici.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dan Wu and Dang-han Xu contributed this paper equally.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, D., Xu, D., Ye, F. et al. Association between fasting blood glucose and intracranial cerebral artery stenosis: a secondary analysis based on a retrospective cross-sectional study in Korean adults. Acta Diabetol 58, 749–757 (2021). https://doi.org/10.1007/s00592-020-01646-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-020-01646-x