Abstract
Aims
To compare the impact of triglyceride–glucose index (TyG-index), the product of fasting plasma glucose (FPG) and triglycerides (TG) with FPG, 2 h post-challenge plasma glucose (2 h-PCPG), TG/high-density lipoprotein cholesterol (TG/HDL-C), and homeostasis model assessment of insulin resistance (HOMA-IR) indices for prediction of type 2 diabetes (T2D) in Iranian adults during a median follow-up of 12 years.
Methods
Study population included 4419 (1858 men) subjects with mean age of 40.6 ± 13.2 years. Multivariable Cox proportional hazard models were used to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) for each 1-standard deviation increase in each predictor. Areas under the receiver operating characteristics curves (AUC) and 95% CIs were calculated.
Results
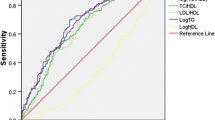
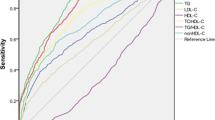
During follow-up, 215 men and 288 women developed T2D. The multivariable HRs for FPG, 2 h-PCPG, TyG-index, HOMA-IR, HOMA2-IR, and TG/HDL-C were 2.20, 1.97, 1.71, 1.33, 1.30, and 1.35 in men and 2.13, 2.11, 1.44, 1.37, 1.32, and 1.36 in women (all P < 0.001). Among the total population, the AUC for FPG [0.752 (0.727–0.776)] was similar to 2 h-PCPG but higher than TyG-index [0.697 (0.673–0.720)], TG/HDL-C [0.644 (0.620–0.669)], HOMA-IR [0.684 (0.659–0.710)], and HOMA2-IR [0.656 (0.630–0.682)]. In men, AUC of TyG-index was higher than TG/HDL-C but did not differ with HOMA-IR indices. In women, the AUC of TyG-index was higher than HOMA2-IR and TG/HDL-C, but was similar to that of HOMA-IR.
Conclusions
FPG is a stronger predictor of T2D than the TyG-index, TG/HDL-C, and HOMA-IR indices. Although TyG-index was better than TG/HDL-C in both genders, it did not rank above HOMA-IR.


Similar content being viewed by others
References
Derakhshan A, Sardarinia M, Khalili D, Momenan AA, Azizi F, Hadaegh F (2014) Sex specific incidence rates of type 2 diabetes and its risk factors over 9 years of follow-up: Tehran Lipid and Glucose Study. PLoS One 9:e102563
Guariguata L (2012) By the numbers: new estimates from the IDF Diabetes Atlas Update for 2012. Diabetes Res Clin Pract 98:524–525
Ghassemi H, Harrison G, Mohammad K (2002) An accelerated nutrition transition in Iran. Public Health Nutr 5:149–155
Eslami A, Mozaffary A, Derakhshan A, Azizi F, Khalili D, Hadaegh F (2017) Sex-specific incidence rates and risk factors of premature cardiovascular disease. A long term follow up of the Tehran Lipid and Glucose Study. Int J Cardiol 227:826–832
Sardarinia M, Akbarpour S, Lotfaliany M, et al (2016) Risk factors for incidence of cardiovascular diseases and all-cause mortality in a middle eastern population over a decade follow-up: Tehran Lipid and Glucose Study. PLoS One 11:e0167623
Kahn S (2003) The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of type 2 diabetes. Diabetologia 46:3–19
Warram JH, Martin BC, Krolewski AS, Soeldner JS, Kahn CR (1990) Slow glucose removal rate and hyperinsulinemia precede the development of type II diabetes in the offspring of diabetic parents. Ann Internal Med 113:909–915
Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling. Diabetes Care 27:1487–1495
Bozorgmanesh M, Hadaegh F, Ghaffari S, Harati H, Azizi F (2010) A simple risk score effectively predicted type 2 diabetes in Iranian adult population: population-based cohort study. Eur J Public Health 21:554–559
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F (2008) The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metabol Syndrome Relat Disord 6:299–304
Abbasi F, Reaven GM (2011) Comparison of two methods using plasma triglyceride concentration as a surrogate estimate of insulin action in nondiabetic subjects: triglycerides × glucose versus triglyceride/high-density lipoprotein cholesterol. Metabolism 60:1673–1676
Lee S-H, Kwon H-S, Park Y-M, Ha H-S, Jeong SH, Yang HK et al (2014) Predicting the development of diabetes using the product of triglycerides and glucose: the Chungju Metabolic Disease Cohort (CMC) study. PLoS One 9:e90430
Navarro-González D, Sánchez-Íñigo L, Pastrana-Delgado J, Fernández-Montero A, Martinez JA (2016) Triglyceride–glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: the Vascular-Metabolic CUN cohort. Prev Med 86:99–105
Janghorbani M, Almasi SZ, Amini M (2015) The product of triglycerides and glucose in comparison with fasting plasma glucose did not improve diabetes prediction. Acta Diabetol 52:781–788
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M et al (2009) Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials 10:5
Ghasemi A, Tohidi M, Derakhshan A, Hasheminia M, Azizi F, Hadaegh F (2015) Cut-off points of homeostasis model assessment of insulin resistance, beta-cell function, and fasting serum insulin to identify future type 2 diabetes: Tehran Lipid and Glucose Study. Acta Diabetol 52:905–915
Unger G, Benozzi SF, Perruzza F, Pennacchiotti GL (2014) Triglycerides and glucose index: a useful indicator of insulin resistance. Endocrinología y Nutrición (English Edition) 61:533–540
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MAG, Hernández-González SO et al (2010) The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metabol 95:3347–3351
Lee ES, Kim JH, Park SE, Park C-Y, Oh K-W, Park S-W et al (2016) Predictive value of triglyceride glucose index for the risk of incident diabetes: a 4-year Retrospective Longitudinal Study. PLoS One 11:e0163465
Navarro-González D, Sánchez-Íñigo L, Fernández-Montero A, Pastrana-Delgado J, Martinez JA (2016) TyG Index change is more determinant for forecasting type 2 diabetes onset than weight gain. Medicine 95:e3646
Zhang M, Wang B, Liu Y, Sun X, Luo X, Wang C et al (2017) Cumulative increased risk of incident type 2 diabetes mellitus with increasing triglyceride glucose index in normal-weight people: the Rural Chinese Cohort Study. Cardiovasc Diabetol 16:30
Akour A, Kasabri V, Boulatova N, Bustanji Y, Naffa R, Hyasat D et al (2017) Levels of metabolic markers in drug-naive prediabetic and type 2 diabetic patients. Acta Diabetol 54:163–170
Wang Y, Yuan Y, Zhang Y, Lei C, Zhou Y, He J et al (2017) Serum 1, 5-anhydroglucitol level as a screening tool for diabetes mellitus in a community-based population at high risk of diabetes. Acta Diabetol 54:425–431
Vasques ACJ, Novaes FS, de Oliveira MdS, Souza JRM, Yamanaka A, Pareja JC et al (2011) TyG index performs better than HOMA in a Brazilian population: a hyperglycemic clamp validated study. Diabetes Res Clin Pract 93:e98–e100
Bastard JP, Lavoie ME, Messier V, Prud’homme D, Rabasa-Lhoret R (2012) Evaluation of two new surrogate indices including parameters not using insulin to assess insulin sensitivity/resistance in non-diabetic postmenopausal women: a MONET group study. Diabetes Metabol 38:258–263
Jagannathan R, Sevick MA, Fink D, Dankner R, Chetrit A, Roth J et al (2016) The 1-hour post-load glucose level is more effective than HbA1c for screening dysglycemia. Acta Diabetol 53:543–550
Noble D, Mathur R, Dent T, Meads C, Greenhalgh T (2011) Risk models and scores for type 2 diabetes: systematic review. BMJ 343:d7163
Hadaegh F, Bozorgmanesh MR, Ghasemi A, Harati H, Saadat N, Azizi F (2008) High prevalence of undiagnosed diabetes and abnormal glucose tolerance in the Iranian urban population: Tehran Lipid and Glucose Study. BMC Public Health 8:176
Acknowledgements
The authors wish to thank the study participants for their enthusiastic cooperation. We would also like to acknowledge Ms. Niloofar Shiva, for critical editing of English grammar and syntax of the manuscript. This manuscript is the result of the MD thesis of Dr Aidin Baghbani-Oskouei.
Funding
This study was supported in part by grant No. 12545-2 from the Shahid Beheshti University of Medical Sciences and by grant No. 121 from the National Research Council of the Islamic Republic of Iran.
Author information
Authors and Affiliations
Contributions
MT, ABO, FH, and FA participated in the conception and design of the study; MT, ABO, and NA carried out the literature search and participated in data collection and analysis; FH, MT, ABO, and NA participated in interpretation of analysis and writing the manuscript; FA and FH participated in final approval of the version to be submitted. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Managed by Massimo Porta.
Rights and permissions
About this article
Cite this article
Tohidi, M., Baghbani-Oskouei, A., Ahanchi, N. et al. Fasting plasma glucose is a stronger predictor of diabetes than triglyceride–glucose index, triglycerides/high-density lipoprotein cholesterol, and homeostasis model assessment of insulin resistance: Tehran Lipid and Glucose Study. Acta Diabetol 55, 1067–1074 (2018). https://doi.org/10.1007/s00592-018-1195-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1195-y